Mucogingival surgery
Mucogingival surgery
The term mucogingival surgery was initially introduced by Freidman in 1957 to describe surgical procedures for the correction of relationships between the gingiva and the oral mucous membrane with reference to three specific problem areas:• Attached gingiva.
• Shallow vestibules.
• Frenum interfering with the marginal gingiva.
periodontal plastic surgery
The 1996 World Workshop renamed mucogingival surgery as(periodontal plastic surgery)
a term originally proposed by Miller in 1993 because the term mucogingival surgery did not adequately describe all the periodontal procedures
periodontal plastic surgery
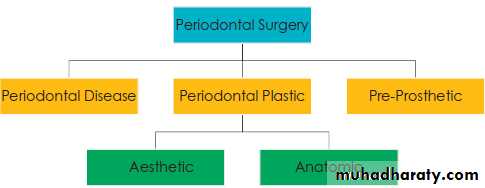
Periodontal plastic surgery is defined as the surgical procedures performed to correct or eliminate anatomic, developmental, or traumatic deformities of the gingiva or alveolar mucosaClassification of periodontal surgery
periodontal plastic surgery It includes the following:
• widening of attached gingiva• deepening of shallow vestibules
• Resection of the aberrant Frenum
• Periodontal prosthetic corrections
• Crown lengthening
• Ridge augmentation
• Aesthetic surgical corrections
• Coverage of the denuded root surface
• Reconstruction of papillae
• Aesthetic surgical correction around implants
• Surgical exposure of unerupted teeth for orthodontics
Mucogingival problems
Pockets extending up to or beyond mucogingival junction.Recession causing denudation of root surfaces.
High frenum and muscle attachment.
Inadequate width of attached gingiva.
contraindications
In patients with advanced age where teeth may last for life without resorting to radical treatment.
Patients with systemic disease.
When patient motivation is inadequate.
In the presence of infection.
Where the prognosis is so poor that tooth loss is inevitable.
objectives
1. Problems associated with attached gingiva2. Problems associated with a shallow vestibule
3. Problems associated with an aberrant frenum
4. Esthetic surgical therapy
5. Tissue engineering
Problems associated with attached gingiva
Problems associated with inadequate width of attached gingiva• Difficulty in maintaining Optimum Gingival Health.
• Improper plaque control.
• Difficulty in maintaining Optimum Gingival Health around abutment teeth.
• Inadequate keratinized tissue for placement of RPD.
Problems Associated With Attached Gingiva
WHY SURGERY?
Rational for Mucogingival surgery was predicated on the assumption that a minimal width of attached gingiva was required to maintain optimal gingival health.
A wide, attached gingiva is more protective against the accumulation of plaque than a narrow or a nonexistent zone.
People who practice good, atraumatic oral hygiene may maintain excellent gingival health with almost no attached gingiva.
individuals whose oral hygiene practices are less than optimal can be helped by the presence of keratinized gingival and vestibular depth.
Problems Associated With Attached Gingiva
To improve aesthetics, the objective is the coverage of the denuded root surface. In the maxillary anterior area, covering of the denuded root surface widens the zone of attached gingiva and creates an improved aesthetic result.A wider zone of attached gingiva is also needed around teeth that serve as abutments for fixed or removable partial dentures and in the ridge areas bearing a denture.
Widening the attached gingiva accomplishes four objectives:
• Enhances plaque removal around the gingival margin• Improves aesthetics
• Reduces inflammation around restored teeth
• Allows gingival margin to bind better around teeth and implants with attached gingiva
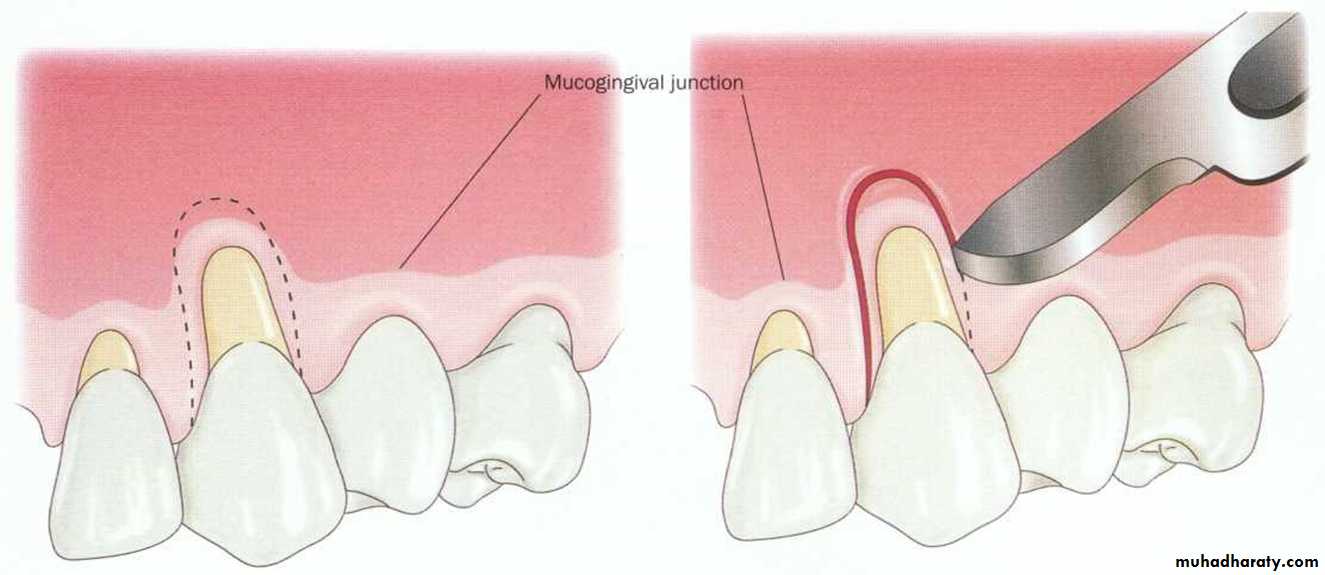
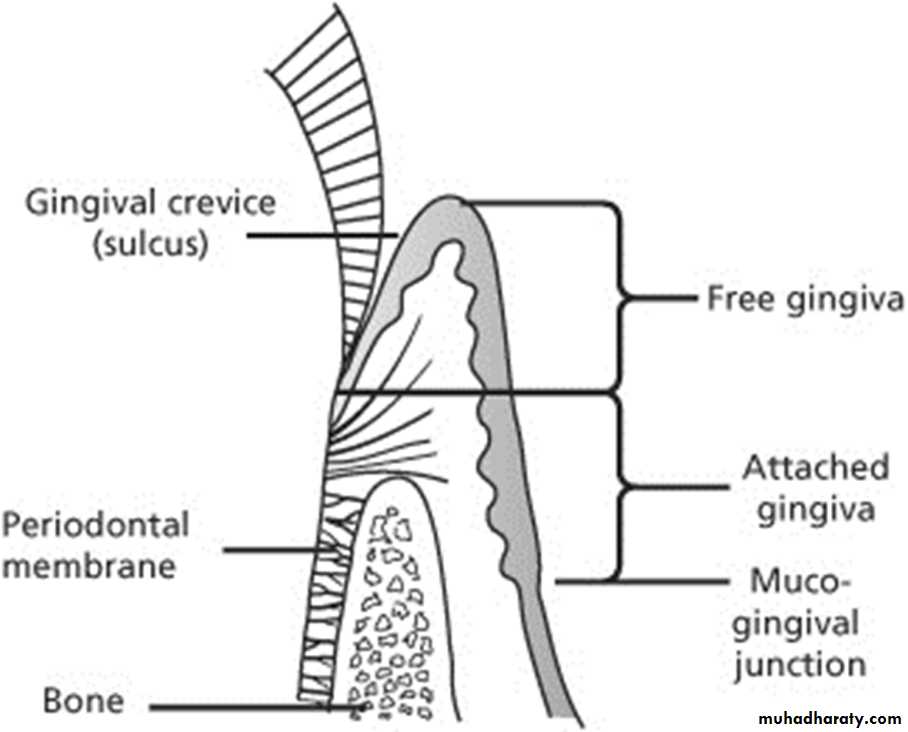
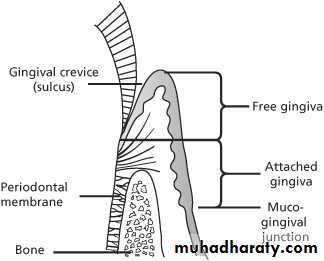
Measurement of Width of Attached Gingiva
Width of attached gingiva can be measured by subtracting pocket or sulcus depth from the distance between free gingival margin to the mucogingival junction.Advantages of Creating Adequate Width of Attached Gingiva
• Proper plaque removal.• Improved esthetics.
• Reduces inflammation around restored teeth.
• Gingival margin binds better around teeth and implants with attached gingiva.
Problems Associated With Shallow Vestibule
Another objective of periodontal plastic surgery is the creation of vestibular depth when it is lacking.With minimal vestibular depth, proper hygiene procedures are jeopardized because there will less space for brush movement.
Minimal A.G with adequate vestibular depth may not require surgical correction if proper atraumatic hygiene is practiced with a soft brush.
Minimal amounts of keratinized attached gingiva with no vestibular depth benefit from mucogingival correction.
Adequate vestibular depth is also necessary for the proper placement of removable prostheses.
Measurement of Vestibular Depth
Depth of vestibule is measured from gingival margin to the bottom of the vestibule.Advantages of Creating Adequate Vestibular Depth
Proper plaque control.
Proper tooth brushing.
Proper placement of removable prosthesis.
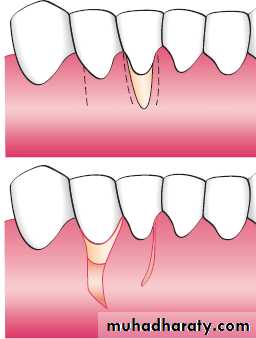
Problems Associated with Aberrant Frenum
A frenum that encroaches on the margin of the gingiva can interfere with biofilm removal, and the tension on the frenum tends to open the sulcus.This condition increases the rate of periodontal recession and contributes to the recurrence of recession, even after treatment.
Problems Associated with Aberrant Frenum
An important objective of periodontal plastic surgery is correction frenal or muscle attachments that may extend coronal to the MGJ.If adequate keratinized, attached gingiva is present coronal to the frenum, it may not be necessary to remove the frenum.
High frenum attachments. A, Frenum between maxillary central incisors. B, Frenum attached to facial surface of maxillary lateral incisors. C, Frenum attached to facial surface of mandibular incisor. D, Frenum attached to facial surface of an incisor.
Aesthetic Surgical Therapy
Recession of the facial gingival margin alters the proper gingival symmetry and results in an aesthetic problem.A missing papilla creates a space which many address as a “black hole.”
An excessive amount of gingiva in the visible area. This condition is often addressed as a “gummy smile” and may be corrected surgically by crown lengthening.
Tissue Engineering
Tissue engineering and the use of biologic mediators in periodontal plastic surgery has become a reality in recent years as the result of the demand for noninvasive surgical procedures by both the patients and clinicians.Tissue Engineering
Tissue engineering is divided into passive and active categories to recognize the role the cells play in tissue engineering.
Passive Engineering
• Therapies based on guided tissue replacement (GTR) based therapies; barrier membranes
• Biologically based acellular dermal matrix (ADM)
Active Engineering
• Enamel matrix derivative (EMD)
• Growth factors: Recombinant human platelet-derived growth factor BB (rhPDGF-BB) + beta-tricalcium phosphate (β- TCP) + collagen wound dressing
• Cell therapy
• Autologous fibroblast: Isolagen
• Bilayered cell therapy (BLCT): Celltx
• Human fibroblast-derived dermal substitute (HFDDS): Dermagraft
Passive Engineering
Barrier membranes allow certain cell types to proliferate but do not offer an active component.GTR and ADM are both considered passive cell manipulation in which the cells themselves are not biologic mediators.
Passive Engineeringacellular dermal matrix (ADM)
ADM is commercially available under the name AlloDerm, and it is derived from donated human skin.Commercial preparation of this tissue includes a multistep process that removes the epidermis and the cells that can lead to tissue rejection and graft failure without damaging the matrix
The remaining ADM consists of a nondenatured, three - dimensional arrangement of intact collagen fibers, ground substance, and vascular channels.
Active Engineering
In active tissue engineering, the cells are biologically active in the regeneration process.
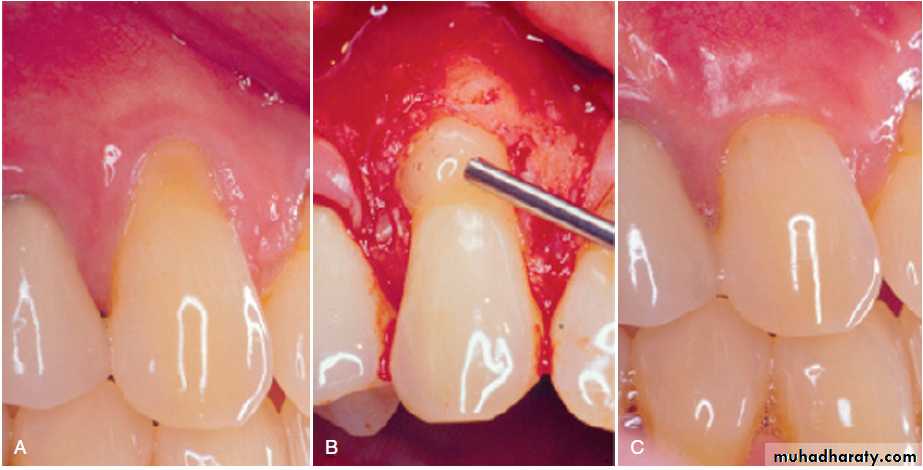
(A) Pretreatment recession defect of 3 mm to be treated with enamel matrix derivative (EMD). (B) Application of EMD to the root surface before coronally advancing the flap with 5-0 plain gut sutures. (C) The 1-year follow-up reveals 100% root coverage and increased keratinized gingiva.
Active Engineering
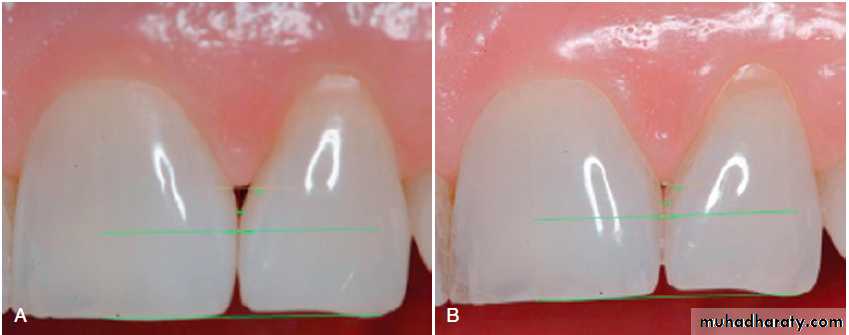
Cell Therapy (Autologous fibroblast)(A) Preoperative view of the open interproximal space. (B) Four months after three injections into the papilla with the patient’s own expanded and concentrated fibroblasts, note the improved papillary form. Green horizontal lines are used for image analysis.
Etiology Of Marginal Tissue Recession
The most common cause of gingival recession and the loss of attached gingiva is abrasive and traumatic tooth brushing habits.Periodontal inflammation and the resultant loss of attachment results in reduced attached gingiva. Advanced periodontal involvement in areas of minimal attached gingiva result in the base of the pocket extending close to, or apical to, the mucogingival junction.
Etiology Of Marginal Tissue Recession
Frenal and muscle attachments that encroach on the marginal gingiva can distend the gingival sulcus, which creates an environment for plaque accumulation.Orthodontic tooth movement through a thin buccal osseous plate may lead to a dehiscence beneath a thin gingiva. This also can lead to the recession of the gingiva.
A, Gingival recession and extreme inflammation around a lower central incisor. B, Advanced recession of mesial root of a first lower molar.
Factors that affect surgical outcome
• Irregularity of teeth:Abnormal tooth alignment is an important cause of gingival deformities.
Location of the gingival margin, width of the attached gingiva, and alveolar bone height and thickness are affected by tooth alignment.
On teeth that are tilted or rotated labially, the labial bony plate is thinner and located further apically than on the adjacent teeth.
Factors that affect surgical outcome
The gingival margin is recessed apically to follow the bone, which leads to the exposure of the root.On the lingual surface of these teeth, the gingiva is bulbous, and the bone margins are closer to the CEJ.
Roots covered with thin bony plates pose a hazard in mucogingival surgery, creates the risk of bone resorption on the periosteal surface.
Factors that affect surgical outcome
• Mucogingival Line:The mucogingival line in the incisor and canine areas is located approximately 3 mm apical to the crest of the alveolar bone on the radicular surfaces and 5 mm interdentally.
In periodontal disease and on malposed, disease-free teeth, the bone margin is located further apically and may extend beyond the mucogingival line.
After inflammation is eliminated, the tissue tends to contract and draw the mucogingival line in the direction of the crown.
Criteria for Selection of Techniques
The following criteria are used for selection of mucogingival techniques:
• Surgical site free of biofilm, calculus, and inflammation.
• Adequate blood supply to the donor tissue.
• Anatomy of the recipient and donor sites.
• Stability of the grafted tissue to the recipient site.
• Minimal trauma to the surgical site.
Surgical site free of biofilm, calculus, and inflammation
Adequate Blood Supply
ALWAYS THINK TO obtain the maximal amount of blood supply to the donor tissue.Gingival augmentation apical to the area of recession provides a better blood supply than coronal augmentation because the recipient site is entirely periosteal tissue.
A pedicle-displaced flap has a better blood supply than a free graft.
Adequate Blood Supply
The Langer subepithelial connective tissue graft (SECTG) procedure and the pouch and tunnel techniques use a split flap with the connective tissue sandwiched between the flaps. This flap design maximizes the blood supply to the donor tissue.Anatomy of the Recipient and Donor Sites
Availability of donor tissue is another anatomic factor that must be considered.
Pedicle displacement of tissue necessitates an adjacent donor site that has gingival thickness and width.
Palatal tissue thickness is also necessary for the connective tissue donor autograft.
Gingival thickness is required at the recipient site for techniques using a split-thickness, sandwich-type flap or the pouch and tunnel techniques.
Anatomy of the Recipient and Donor Sites
The presence or absence of vestibular depth is an important anatomic factor at the recipient site for gingival augmentation.Mucogingival techniques, such as free gingival grafts and free connective tissue grafts, can be used to create vestibular depth and widen the zone of attached gingiva.
Other techniques require vestibular depth to exist before the surgery, including pedicle grafts (i.e., lateral and coronal), the Langer SECTG, and pouch and tunnel procedures.
Stability of the Grafted Tissue to theRecipient Site
Good communication of the blood vessels from the grafted donor tissue to the recipient site requires a stable environment.The least amount of sutures and maximal stability should be achieved.
Minimal Trauma to the Surgical Site
Unnecessary tissue trauma caused by:1- poor incisions,
2- flap perforations, tears,
3-traumatic amd excessive placement of sutures can lead to tissue necrosis.
To minimize tissue trauma;
1-The selection of proper instruments, needles, and sutures is mandatory sharp contoured blades, smaller-diameter needles,
2-Resorbable monofilament sutures all are important factors in achieving atraumatic surgery.
Techniques to Increase Attached Gingiva
Gingival augmentation apical to the area of recession.
No attempt is made to cover the denuded root surface where there is gingival and bone recession.
Gingival augmentation coronal to the recession.
The donor graft tissue (i.e., pedicle or free) is placed covering the denuded root surface.
Gingival Augmentation Apical to Recession
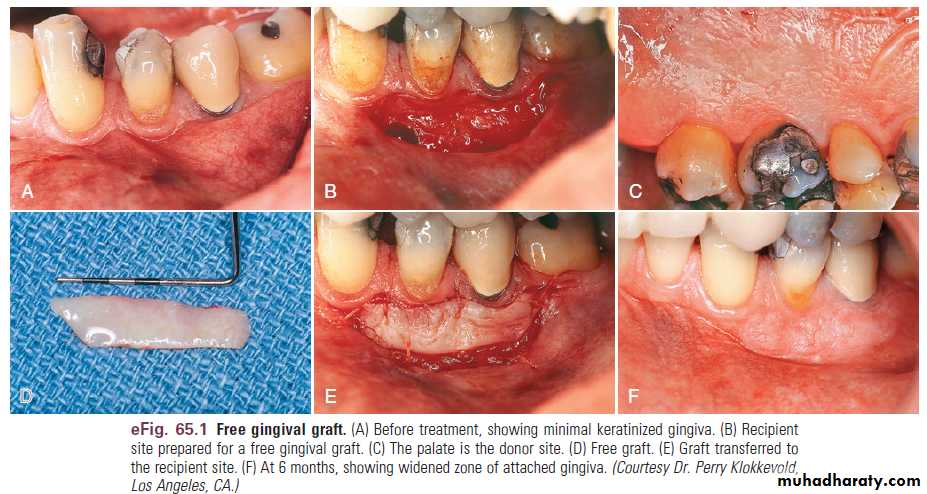
• Free Gingival Autografts.• The Classic Technique
• Variant Techniques
• The accordion technique,
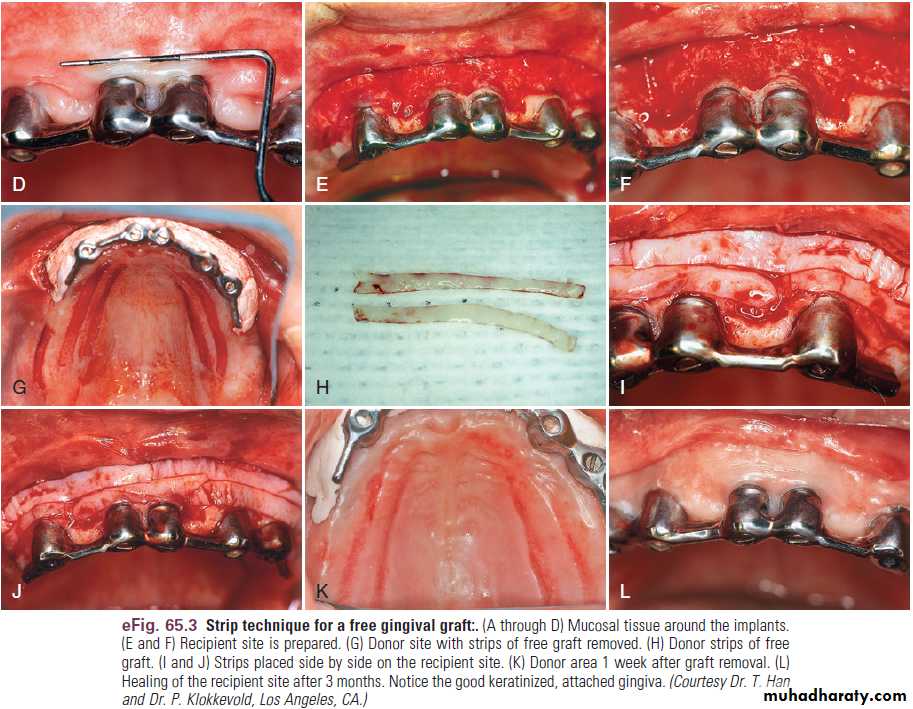
• The strip technique,
• The combination epithelial-connective tissue strip technique.
• Alternative Donor Tissue.
• Acellular dermal matrix (ADM)
Gingival Augmentation Apical to Recession
The Classic TechniqueTechniques to Increase Attached Gingiva
Variant TechniquesTechniques to Increase Attached Gingiva
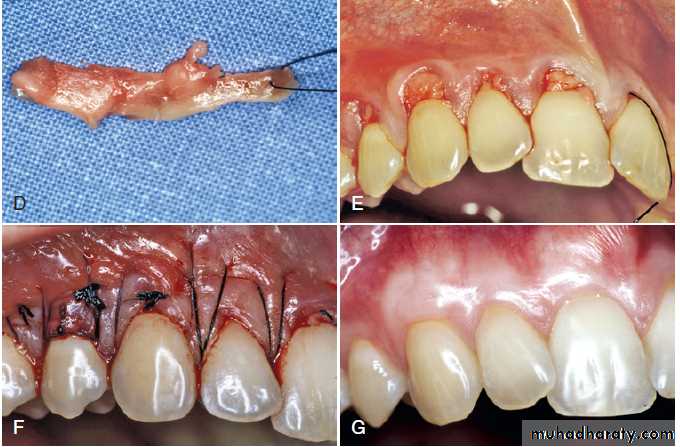
Alternative Donor Tissue. ( ADM )Preoperative view.
(B) Intrasulcular incision.(C) AlloDerm on the surface before insertion into the pouch.
(D) AlloDerm sutured in the pouch.
Techniques to Increase Attached Gingiva
Alternative Donor Tissue(E) Pouch coronally positioned and sutured.
(F) Postoperative view after 1 month.(G) Postoperative view after 1 year.
Gingival Augmentation Apical to Recession
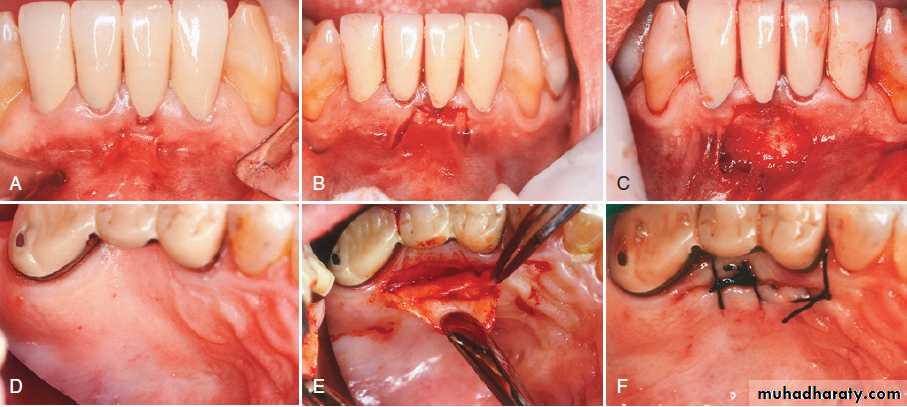
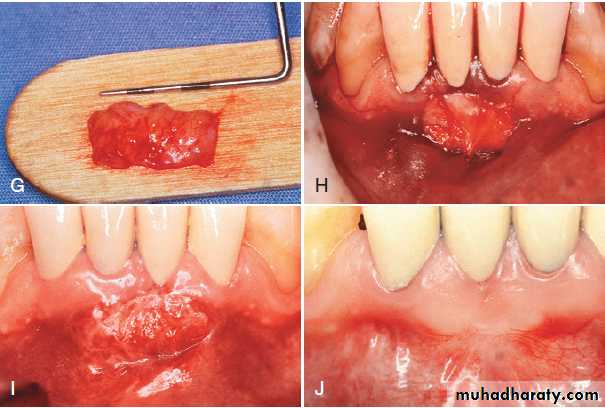
• Free Connective Tissue Autografts.• The advantage of this technique:
• the donor tissue is obtained from the undersurface of the palatal flap, which is sutured back in primary closure.
• The patient has less discomfort postoperatively at the donor site.
• improved aesthetics can be achieved because of a better color match
Gingival Augmentation Apical to Recession
Free Connective Tissue Autografts.(A) Lack of keratinized, attached gingiva buccal to the central incisor. (B) Vertical incisions to prepare the recipient site. (C) Recipient site is prepared. (D) Palate from which connective tissue is removed for donor tissue. (E) Removal of connective tissue. (F) Donor site is sutured.
Gingival Augmentation Apical to Recession
Free Connective Tissue Autografts.
(G) Connective tissue for the graft. (H) Free connective tissue is placed at the donor site. (I) Postoperative healing at 10 days. (J) Final healing at 3 months. Notice the wide, keratinized, attached gingiva.
Gingival Augmentation Apical to Recession
• Apically Displaced Flap• This technique uses a partial-thickness or full-thickness, apically positioned flap to increase the zone of keratinized gingiva.
• Adequate vestibular depth must be present before the surgery to allow apical positioning of the flap
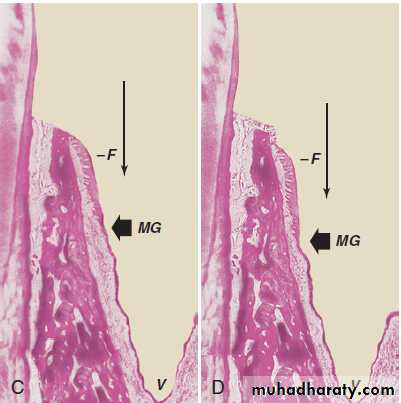
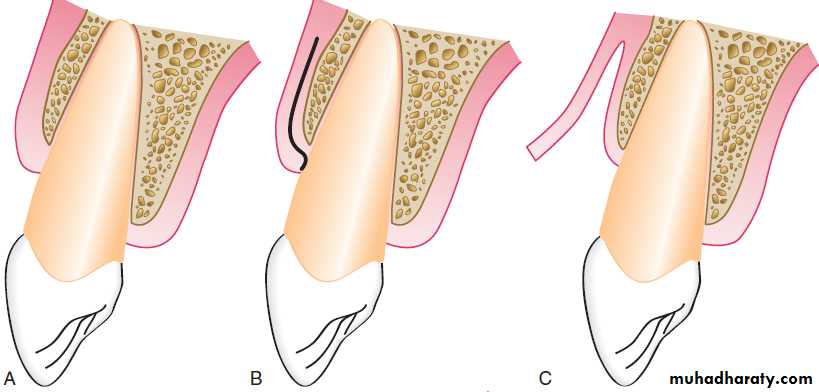
Apically displaced partial-thickness flap. (A) Internal bevel incision (I) separates the inner wall of the periodontal pocket. (B) Partial-thickness flap (F) is separated, leaving periosteum and a layer of connective tissue on the bone. The inner wall of the periodontal pocket (I) is removed, and the tooth is scaled and planed. (C) Partial-thickness flap (F) is displaced apically, with the edge of the flap at the crest of the bone. The vestibular fornix is also moved apically. (D) Partial-thickness flap (F) is displaced apically, with the edge of the flap several millimeters below the crest of the bone. MG, Mucogingival junction; V, vestibular fornix.
Gingival Augmentation Coronal to Recession
The predictability of root coverage can be enhanced by the presurgical examination and the correlation of the recession by using the classification proposed by Miller
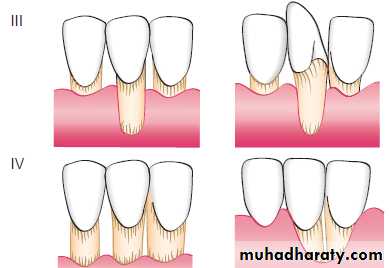
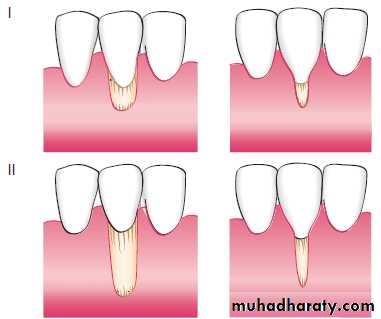
Class I. Marginal tissue recession does not extend to the mucogingival junction. There is no loss of bone or soft tissue in the interdental area. This type of recession can be narrow or wide.
Class II. Marginal tissue recession extends to or apical to the mucogingival junction. There is no loss of bone or soft tissue in the interdental area. This type of recession can be subclassified as wide and narrow.
Class III. Marginal tissue recession extends to or apical to the mucogingival junction. There is bone and soft tissue loss interdentally or malpositioning of the tooth facially.
Class IV. Marginal tissue recession extends to or apical to the mucogingival junction. There is severe bone and soft tissue loss interdentally or severe tooth malposition.
Gingival Augmentation Coronal to Recession
The prognoses for classes I and II are good to excellent; whereas for class III, only partial coverage can be expected. Class IV has a very poor prognosis with current techniques.Miller’s classification of denuded roots.
Gingival Augmentation Coronal to RecessionThe following is a list of techniques used for gingival augmentation coronal to the recession (root coverage):
1. Free gingival autograft
2. Free connective tissue autograft
3. Pedicle autografts
• • Laterally (horizontally) positioned flap
• • Coronally positioned flap; includes semilunar pedicle (Tarnow)
6. Subepithelial connective tissue graft (Langer)
7. Guided tissue regeneration
8. Pouch and tunnel technique
Gingival Augmentation Coronal to Recession
Pedicle Autograft
Laterally Displaced Pedicle Flap
• The laterally (horizontally) positioned flap can be used to cover the isolated, denuded root surfaces that have adequate donor tissue adjacent to the recipient site. The vestibular depth must exist to laterally move the pedicle.
Gingival Augmentation Coronal to Recession
Laterally Displaced• Pedicle Flap
Gingival Augmentation Coronal to Recession
Laterally Displaced Pedicle FlapVariant Techniques
A common alternative is the use of converging oblique incisions over the recipient site and a vertical or oblique incision at the distal end of the donor site to allow the flap to have a slightly wider base.
Gingival Augmentation Coronal to Recession
The lateral pedicle, partial-thickness grafts from neighboring edentulous areas can be used to restore attached gingiva on teeth adjacent to edentulous spaces with denuded roots and minimal vestibular depth.The double-papilla flap attempts to cover roots denuded by isolated gingival defects with a flap formed by joining the contiguous halves of the adjacent interdental papillae.
Gingival Augmentation Coronal to Recession
Coronally Displaced Flap
First Technique
two vertical incisions, internal bevel incision is made from the gingival margin to the bottom of the pocket to eliminate the diseased pocket wall, Scale and plane the root surface, Return the flap, and suture it at a level coronal to the pretreatment position.
Variation
gingival augmentation procedure with a free autogenous graft can be performed before the coronally positioned graft
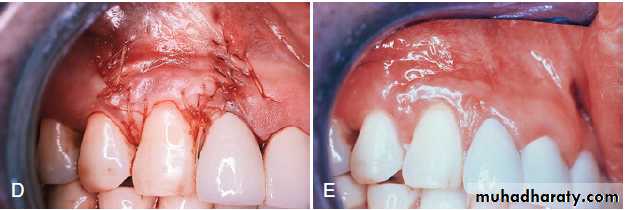
Coronally displaced flap. (A) Preoperative view, showing the recession and the lack of attached gingiva. (B) After placement of a free gingival graft. (C) Three months after placement of the graft. (D) Flap, including the graft, positioned coronally and sutured. (E) Six months later, showing the root coverage and attached gingiva.
Gingival Augmentation Coronal to Recession
Coronally Displaced FlapSecond Technique
• (Semilunar coronally positioned flap)
This technique is simple and predictably provides 2 to 3 mm of root coverage. It can be performed on several adjoining teeth. The technique is indicated for areas where the recession is not extensive (<3 mm) and the facial gingival biotype is thick.
Semilunar coronally positioned flap. (A) Slight recession in the facial aspect of the upper left canine. (B–D) After thorough scaling and root planing of the area, a semilunar incision is made, and the tissue is separated from the underlying bone. The flap collapses, covering the recession. (E) Appearance after 7 weeks, showing coverage of the previous root denudation.
Gingival Augmentation Coronal to Recession
Subepithelial Connective Tissue GraftThe subepithelial connective tissue graft is indicated for larger and multiple defects with good vestibular depth and gingival thickness to allow a split-thickness flap to be elevated.
Subepithelial connective tissue graft for root coverage. (A through E) Sagittal views. (A) Preoperative view of facial recession on a maxillary central incisor. (B) Split-thickness incision for the recipient site. (C) Split-thickness flap is reflected. (D) Connective tissue is placed over the denuded root surface. The apical portion of the donor tissue is placed between the split-thickness flaps. (E) Recipient flap is closed. Subepithelial connective tissue graft is used for root coverage.
Gingival Augmentation Coronal to Recession
Guided Tissue Regeneration Technique for Root CoverageTheoretically, GTR should result in reconstruction of the attachment apparatus, along with coverage of the denuded root surface
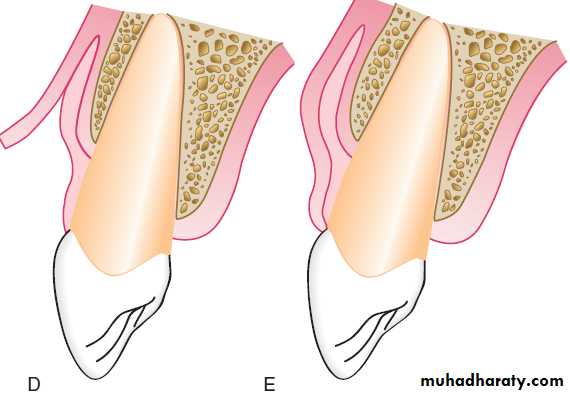
Guided tissue regeneration technique for root coverage. (A) Marked recession of the left maxillary cuspid. (B) Vertical incisions are made, and the membrane is placed over the recession. (C) Flap is sutured over the membrane. (D) Postoperative result, showing complete coverage of recession.
Gingival Augmentation Coronal to Recession
Pouch and Tunnel TechniqueAlso referred to as the coronally advanced tunnel technique.
To minimize incisions and the reflection of flaps and to provide abundant blood supply to the donor tissue.
An advantage of this technique is thickening of the gingival margin after healing
Pouch and tunnel technique for root coverage. (A) Preoperative view, showing gingival recession. (B) A sulcular incision is made from the mesial to the facial line angles. (C) A tunnel is made through the papilla using a blunt incision. (D) A connective tissue graft is taken from the palate. (E) The connective tissue is placed through the papillary tunnel and apically beneath the pouch. (F) The facial gingival margin covers the connective tissue using horizontal mattress sutures interdentally. (G) Postoperative view, showing complete root coverage and a thickened gingival margin at 3 months.
Techniques To Deepen Vestibule
The presence of adequate vestibular depth is important for both oral hygiene and retention of prosthetic appliances.Numerous surgical techniques have been proposed to accomplish the objective of deepening the vestibule.
The classic clinical studies indicated that deepening of the vestibule by non–free graft procedures were not successful when evaluated years later.
Predictable deepening of the vestibule can only be accomplished by the use of free autogenous graft techniques.
Techniques to Remove the Frenum
Frenectomy and Frenotomy
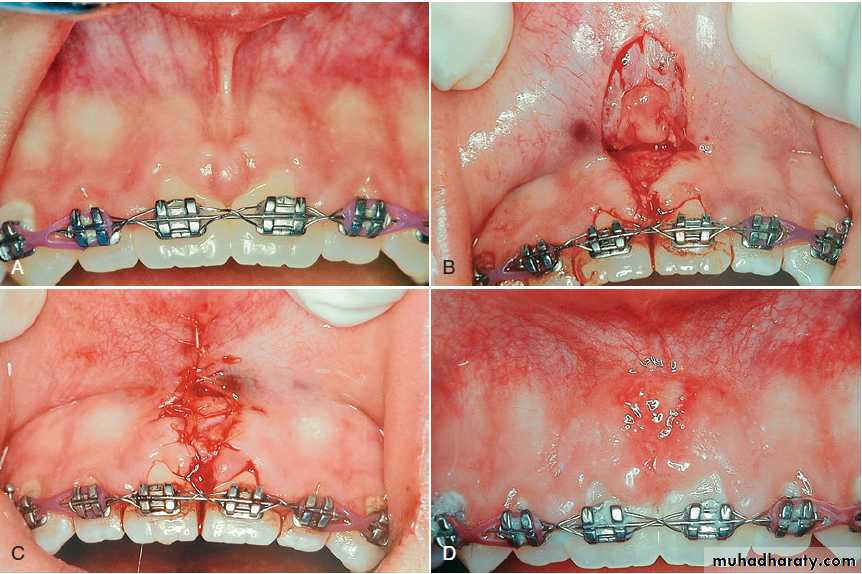
Frenectomy is complete removal of the frenum, including its attachment to underlying bone, and it may be required in the correction of an abnormal diastema between the maxillary central incisors.
Frenotomy is relocation of the frenum, usually in a more apical position.
Techniques to Remove the Frenum
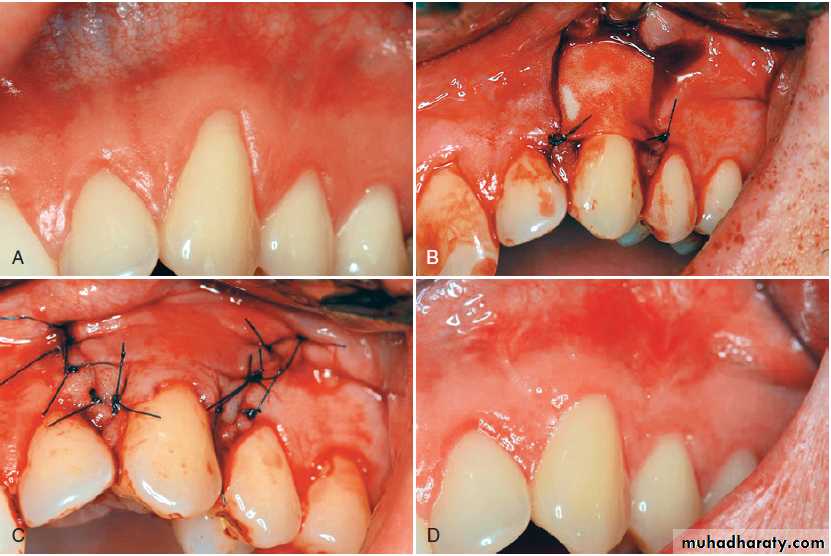
Removal of the frenum. (A) Preoperative view of frenum between the two maxillary central incisors. (B) Removal of the frenum from the lip and gingiva. (C) The site is sutured after a connective tissue graft is placed over the wound. (D) Postoperative view at 2 weeks.