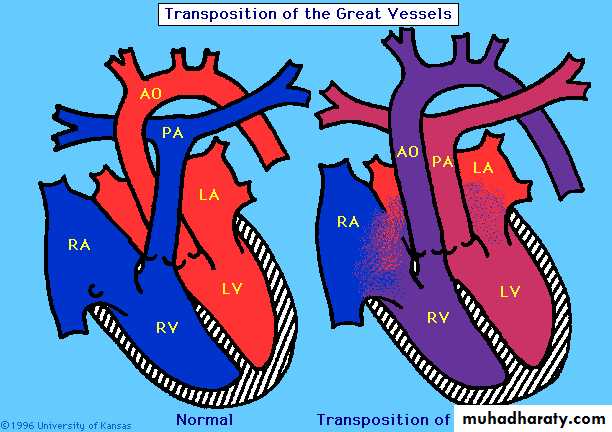
Transposition of Great
Arteries (TGA)• Account for 5% of all CHD
• It is the most common cyanotic disease present in the neonatal period.
• In TGA the aorta arises from Rt ventricle
• Pulmonary artery arises from the Lt ventricle.
• This will result in:
• Desaturated blood return to the Rt side of the heart and pumped back to the body via the aorta• Oxygenated blood from the lungs enter the Lt side of the heart and pumped back to the lungs via the pulmonary artery.
• Death occurs shortly after birth without mixing of the tow circulations.
• This mixing may occurs in atrial level (through a patent foramen ovale or ASD)• Or at ventricles (through a VSD)
• Or at great vessels (through PDA).
• Cyanosis is always present and its severity depend on the amount of mixing between systemic and arterial circulations.
• Tachypnea.
• Single S2, and if there’s no VSD there’s no murmur.
Clinical Features:
• Children with TGA and large VSD may present with signs of heart failure with:
• palpable Lt and Rt V impulses• single S2 and load VSD murmur (pansystolic murmur).
ECG: shows Rt axis deviation and RVH.
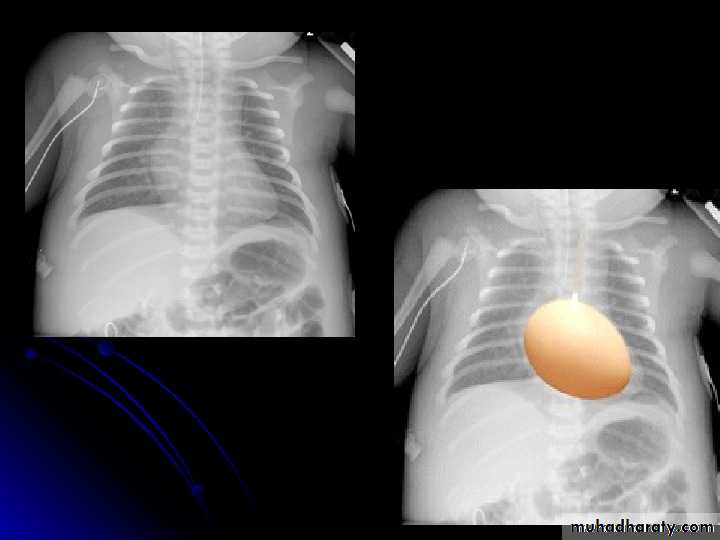
CXR:• increase pulmonary vascularity
• egg on a string caused by narrow superior mediastinum.
Diagnosis:
Echocardiography:
• transposition of great artery• site and amount of the shunt
• any associated anomalies.
• Prostaglandin E1 infusion immediately after birth to maintain the patency of ductus arteriosus and allow mixing of the blood.
• Balloon atrial septostomy done if there’s no response to prostaglandin infusion.
• Complete surgical repair by arterial switch operation. It is usually done within the first 2 weeks of life.
Treatment:
Acquired Heart Diseases
Infective Endocarditis (IEC):• Acute and subacute bacterial endocarditis
• Non-bacterial endocarditis caused by viruses, fungi and other microorganisms.
• It is a significant cause of morbidity and mortality in children and adolescents.
Vascular endothelium damage
Pathogenesis:Jet streams of turbulent blood (from PDA, VSD, or systemic-pulmonary shunt)
Nonbacterial thrombotic embolus
• Prior congenital or rheumatic heart diseases.
• Preceding dental, urinary tract or intestinal procedures.• Intravenous drug use.
• Central venous catheter.
• Prosthetic heart valve.
Predisposing factors:
• Streptococcus Viridans
• Staphylococcus aureus
Causative MO (Etiology):
• Other: St. pneumoniae, H. influenzae, coagulase-negative staphylococci and fungi are less common.
• Blood culture is negative in about 6% of cases
the most
commonSymptoms:
• Early: mild prolonged fever with occasional weight loss.• Or acute and sever onset with high intermittent fever and prostration
• “nonspecific” : fatigue, myalgia, arthralgia, headache, chills, nausea and vomiting, chest and abdominal pain, dyspnea, night sweating and CNS (stroke and seizures).
Clinical Features:
• Elevated body temperature.
• Tachycardia.• Petechiae.
• New or changing heart murmur.
• Splenomegaly.
• Signs of heart failure and arrhythmias.
• Clubbing.
• Metastatic infections (Arthritis, meningitis, Mycotic arterial aneurysm, pericarditis, abscesses)
Clinical signs:
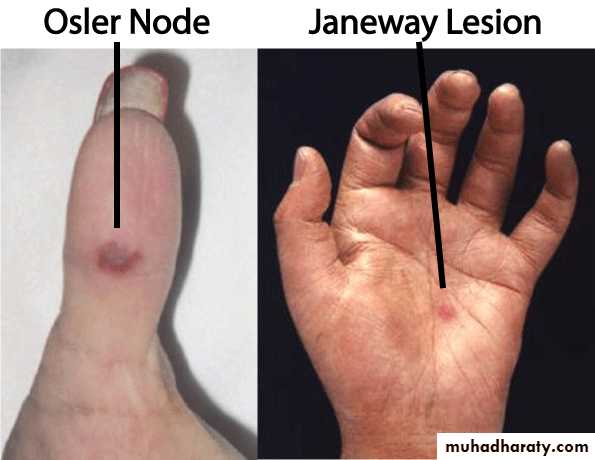
• Classical skin signs: later in the course of the disease and they may be vasculitis caused by circulating Ag-AB complexes. These signs are:
• Osler nodes (tender,
pea-size intradermal nodulesin the pads of the fingers
and toes)
• Janeway lesions (painless small erythematous or hemorrhagic lesions on the palms and soles).
• Splinter hemorrhages (linear lesions beneath the nails).
1. Blood culture:
• Is the main way for confirmation of IEC.
• 3-5 blood samples should obtained after perfect sterilization of skin.
• Causative agent is recovered from the first 2 blood cultures in 90% of the cases.
• The bacteremia is low grade in 80% of cases (<100 colony units\ ml of blood).
Diagnosis:
• Elevated ESR and C-reactive protein.
• CBC: anemia and leukocytosis.• Immune complexes detection.
• Positive rheumatoid factor.
• GUE: hematuria.
• Echocardiography shows evidence of valve vegetation, prosthetic valve dysfunction, myocardial abscess, and new-onset valve insufficiency.
• Heart failure (most common) due to aortic or mitral vegetations.
• Systemic emboli: CNS and pulmonary.• Mycotic aneurysm.
• Valvular obstruction by large vegetation.
• Acquired VSD.
• Heart block due to involvement of conducting system.
Complications:
• Other complications: meningitis, osteomyelitis, arthritis, renal abscess and immune complex-mediated GN.
• Antibiotic therapy immediately once the diagnosis is made.
• Empirical antibiotic therapy include:• Vancomycin (40mg\kg\24 hr in 2-3 divided doses)
• Plus Ceftriaxone (100mg\kg\24 hr once a day).
Treatment:
• Antibiotic therapy should continue for 4-6 weeks and modified according to the blood culture results
• If the cause is St. Viridans :
• crystalline penicillin G (200,000 IU\kg\day) or ceftriaxone
• If the patient is sensitive to penicillin: ceftriaxone plus gentamycin or Vancomycin.
• If the cause is staphylococci:
• naficillin or oxacillin for 6 wk plus gentamycin for 3-5 days (optional).• If the patient is allergic to penicillin: ceftazolin for 6 wk plus gentamycin for 3-5 days (optional).
• If the patient is infected by oxacillin-resistance strains : Vancomycin for 6 wks.
• Treatment of heart failure by:
• diuretics• after load reducing agents
• digoxin.
Prevention:
• Indicated only before dental procedures in patient with:
• Prosthetic cardiac valve.
• Previous IEC.
• Congenital heart diseases:
• Unrepaired cyanotic CHD including palliative shunts.
• Completely repaired CHD with prosthetic materials during the first 6 mo after the procedure.
• Repaired CHD with residual defect at the site or adjacent to the prosthetic device.
• Cardiac transplant recipients.
• Permanently damaged valve by rheumatic heart disease.
• Oral amoxicillin 50 mg\kg.
• If the patient is unable for oral intake:• Ampicillin 50mg\kg IM or IV
• Or Ceftriaxone 50mg\kg IM or IV
• Patients allergic to penicillin and able for oral intake:
• Cephalexin 50 mg\kg
• Or clindamycin 20mg\kg.
• Or Azithromycin or clarithromycin.
Prophylactic antibiotic regimens for dental procedures:
• Patients allergic to penicillin and unable for oral intake:
• Ceftriaxone 50mg\kg IM or IV.
• Or clindamycin 20mg\kg IM or IV.
• Mortality rate 20-25%
• Serious morbidity occur in 50-60% despite of antibiotic therapy.Prognosis:
Thank you for your attention