Principles of endodontic surgery
Principles of endodontic surgery
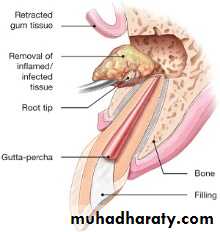
Endodontic surgery is the management or prevention of peri-radicular pathosis by a surgical approach. Peri-radicular surgery (PRS) (endodontic surgery) is a generic term for treatment that encompasses three main categories of surgical endodontic procedures:1. Periapical curettage of persistent peri-radicular disease, including removal of the root apex (root end resection)(Apecoectomy) and retrograde filling of the root canal
2. Surgical repair of root surface irregularities such as external root resorption defects or iatrogenic perforations.
3. Root resection of posterior teeth to remove diseased roots and retention of roots suitable for further coronal restoration.
Conventional endodontic treatment is generally a successful procedure; however, in 10% to 15% of cases the symptoms can persist or spontaneously recur. Findings such: as a draining fistula, pain on mastication, or the incidental noting of a radiolucency increasing in size indicate problems with the initial endodontic procedure.
Periapical Surgery (apicectomy or apicoectomy)
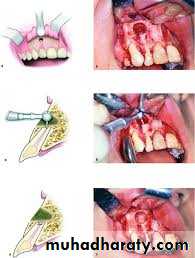
Periapical surgery includes the following:1. Appropriate exposure of the root and apical region
2. Exploration of the root surface for fractures or other pathologic conditions
3. Curettage of the apical tissues
4. Resection of the root apex
5. Retrograde preparation with the ultrasonic tips or microdrills
6. Placement of the retrograde filling material
7. Appropriate flap closure to permit healing and minimize gingival recession
Indications for periapical surgery
• Anatomic problems preventing complete debridement / obturation• Restorative considerations that compromise treatment
• Horizontal root fracture with apical necrosis
• Irretrievable material preventing canal treatment or retreatment
• Procedure errors during treatment
• Large periapical lesions that do not resolve with root canal treatment
Anatomic problems
Calcifications or other blockages,.severe root curvature or constricted canals (i.e., calcific metamorphosis) may compromise root canal treatment, that is, prevent
instrumentation, obturation, or both. A non-obturated and cleaned canal may lead to failure because of continued apical leakage.
Although the outcome may be questionable, it is preferable to attempt conventional root canal treatment or retreatment before apical surgery. If this is not possible, removing or resecting the un-instrumented and unfilled portion of the root and placing a root end filling may be necessary.
Restorative considerations
Root canal retreatment may be risky because of problems that may occur from attempting access through a restoration, such as through a crown on a mandibular incisor. An opening could compromise retention of the restoration or perforate the root.A common requirement for surgery is failed treatment on a tooth that has been restored with a post and core. Many posts are difficult to remove or may cause root fracture if an attempt at removal is made to re-treat the tooth.
Horizontal root fracture
Occasionally, after a traumatic root fracture, the apical segment undergoes pulpal necrosis. Because pulpal necrosis cannot be predictably treated from a coronal approach, the apical segment is removed surgically after root canal treatment of the coronal portion.
Irretrievable material in canal
Canals are occasionally blocked by objects such as broken instruments, restorative materials, segments of posts, or other foreign objects. If evidence of apical pathosis is found, those materials can be removed surgically, usually with a portion of the root. A broken file can be left in the root canal system if the tooth remains asymptomatic.Procedural error
Broken instruments, gross overfills, and perforations may result in failure Although overfilling is not in itself an indication for removal of the material, surgical correction is beneficial in these situations if the tooth becomes symptomatic. Because the obturation of the canal is often dense in these situations, surgical treatment has an excellent prognosis.Large, unresolved lesions after root canal treatment
Occasionally, very large periradicular lesions may enlarge after adequate debridement and obturation.Contraindications for periapical surgery
• Local anatomic factors, such as an inaccessible root end• Tooth with inadequate periodontal support
• Tooth has a vertical root fracture
• Uncooperative patient
• Patients with a severely compromised medical history
• Tooth is unrestorable
• Inexperienced operator with no training
Important considerations in periapical surgery:
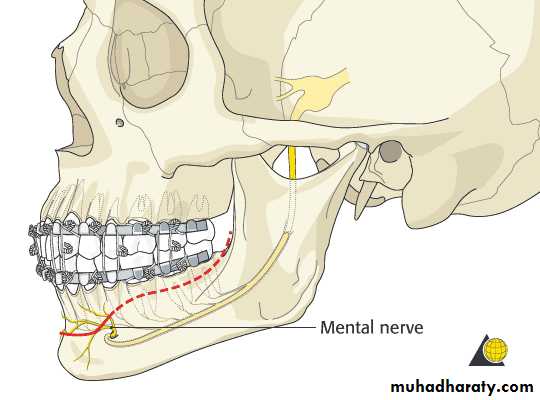
An important consideration is, first, to identify the cause of failure, and then second, to design an appropriate corrective treatment plan.Most oral structures do not interfere with a surgical approach but must be considered. Expertise in operating around a structure such as the maxillary sinus or mental nerve region is imperative before undertaking surgery in these regions.
patient not to exert pressure by forcibly blowing the nose until the surgical wound has healed (for 2 weeks).
Surgical procedures around the mental foramen require caution to avoid stretch injury or direct damage to the nerve.
Important to note is that the nerve may have an anterior loop of 2 to 4 mm, so that distance should be accounted for anteriorly.
Factors Associated with Success and Failures in Periapical Surgery:
SUCCESS:Preoperative Factors:
• Dense orthograde fill
• Healthy periodontal status
• No dehiscence
• Adequate crown/root ratio
3. Radiolucent defect isolated to apical one third of the tooth .
4. tooth treated
• Maxillary 1ncisor
• Mesio-buccal root of maxillary molars
Postoperative Factors
• Radiographic evidence of bone fill following surgery
• Resolution of pain and symptoms
• Absence of sinus tract
• Decrease in tooth mobility
FAILURE
Preoperative Factors• Clinical or radiographic evidence of fracture
• Poor or lack of orthograde filling
• Marginal leakage of crown or post
• Poor preoperative periodontal condition
• Radiographic evidence of post perforation
• Tooth treated
A. Mandibular incisor
Postoperative Factors
• Lack of bone repair following surgery• Lack of resolution of pain
• Fistula does not resolve or returns
Pre-operative imaging
Conventional radiograph.
These two-dimensional (2D) images of three- dimensional (3D) structures have their limitations. For example, conventional periapical radiographs do not facilitate accurate predictions in the preoperative assessment for the potential perforation of the maxillary sinus. As a consequence the use of 3D cone-beam computed tomography (CBCT) imaging is now becoming established in preoperative assessment for PRS.
Surgical procedure
Prophylactic antibioticsA preoperative dose of penicillin V (2.0 g) or clindamycin (600 mg) 1 hour before surgery should be considered by the surgeon.
Surgical access
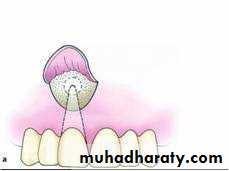
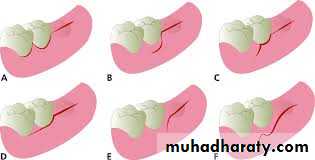
Semilunar flap
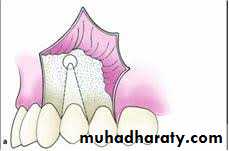
Triangular flap (2 sided flap)
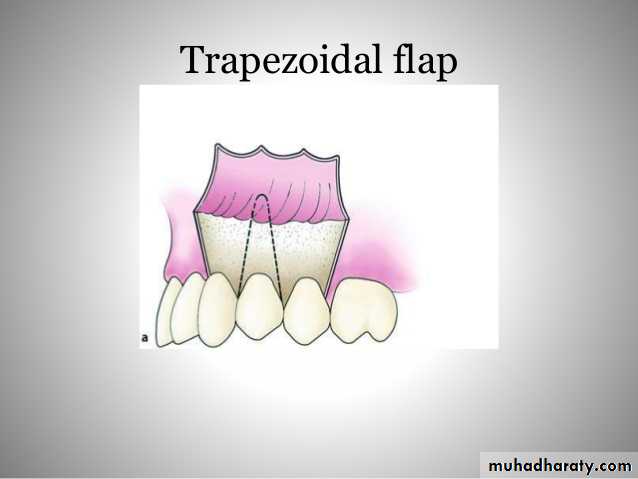
Trapezoidal flap (3 sided flap)Anesthesia:
Incision and reflection:Periapical Exposure:
Curettage:
Root end resection:
Root end preparation and restoration:
Root end filling materials:
Flap replacement and suturing:
Postoperative instructions:
Suture removal and evaluation
To perform biopsy or not:To solve this dilemma logically, certain guidelines have been set up for not to submit tissue for histopathological examination. These guidelines are:
1- Clear evidence of pre-existing endodontic involvement of a tooth (pulpal
necrosis was present, not just a periapical radiolucency).
2- Unilocular radiolucency associated with apical one-third of the tooth.
3- Lesion is not in association with an impacted tooth.
4- No history of malignancy that could represent spread of a metastasis:
5- Patient will return for follow-up examinations and radiographs.
Determination of success:
The treatment outcome of apical surgery should be assessed clinically and radiographically.
Clinical healing is based on the absence of signs and symptoms such as pain, Sinus tract, swelling, apico-marginal communication, and tenderness to palpation or percussion.
Standard radiographic healing classes include complete healing, incomplete healing ("scar tissue formation"), uncertain healing (partial resolution of postsurgical radiolucency), and unsatisfactory healing (no change or an increase in postsurgical radiolucency).
Microsurgical technique:
Fiber opticsA new system, known as endoscopy, is available that uses a very small, flexible fiber bundle that contains a light and an optic system. The optics are connected to a monitor that permits visualization of precise details of the surgical site. This system also gives the clinician the option of videotaping and recording procedures.
Guided tissue regeneration (GTR)