Pathology of therespiratory system
Learning Objectives
• Distinguish between the most important diseases of the respiratory system• Describe the types of acquired atelectasis
• Differentiate between various types of COPD
• Demonstrate the main characteristics of different types of emphysema
• Discuss the pathologic characteristics of chronic bronchitis
• Compare between extrinsic and intrinsic asthma
7. Conclude the difference between lobar pneumonia and bronchopneumonia
8. Verify between main histologic types of bronchogenic carcinomas.9. Discuss the main pathologic characteristics of tuberculosis
10. Describe paraneoplastic syndromes in patients with lung cancer
Introduction
Atalectasis
Obstructive Pulmonary Disease (COPD)
Restrictive (Infiltrative) Pulmonary Disease
Vascular Pulmonary Diseases
INFECTIONS
NEOPLASMS
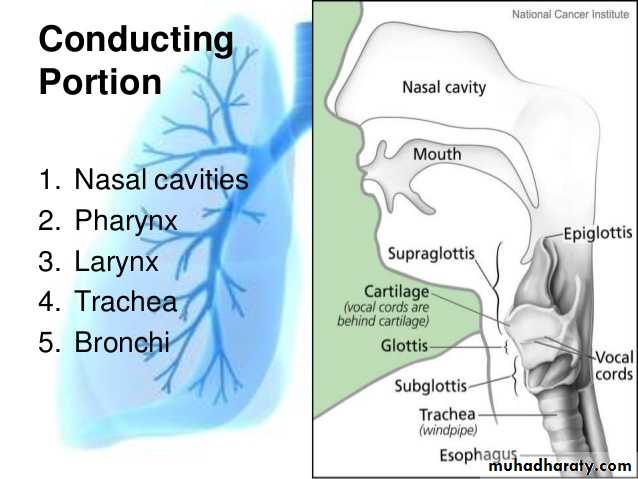
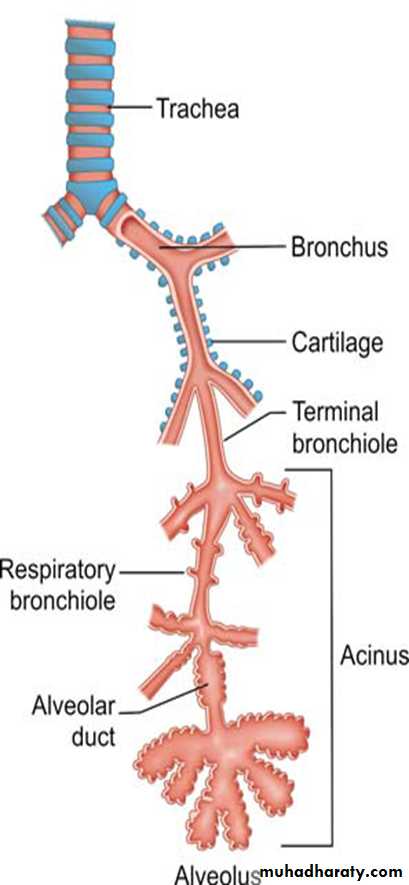
IntroductionThe respiratory system consists of two divisions with distinct structural elements that reflect their unique functions. These include:
The conducting airways, which serve to conduct, clean, warm, and moisten the air.
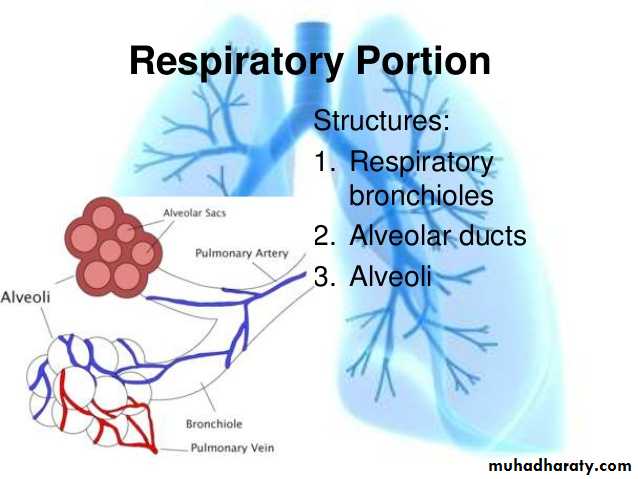
6. T. BronchioleThe respiratory airways, which facilitate gas exchange. These are located entirely within the lung .
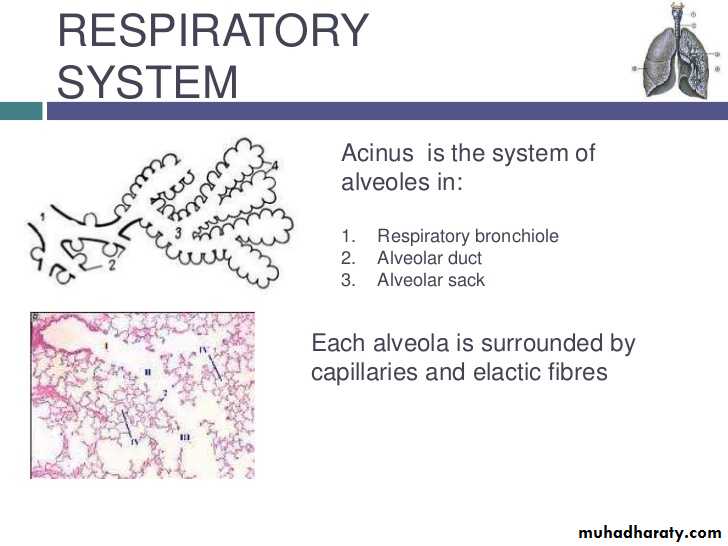
Acinus is the functioning unit of respiratory system
1- respiratory bronchiole(B)
2- alveolar duct(D)
3- alveolar sac(C)
4- Alveoli
a lobule is composed of about 5 acini distal to a terminal bronchiole.
an acinus consists of 3 to 5 generations of respiratory bronchioles and a variable number of alveolar ducts and alveolar sacs.
Atelectasis (collapse)
Definition:Incomplete expansion of the lungs (neonatal atelectasis) or collapse of previously inflated lung (adult atelectasis)
producing areas of relatively airless pulmonary parenchyma.
Types:
Resorption atelectasis
Compression atelectasis (passive atelectasis)
Contraction atelectasis
1- Resorption atelectasis
complete obstruction of an airway.Over time, air is resorbed from the dependent alveoli, which collapse. Since lung volume is diminished, the mediastinum shifts toward the atelectatic lung.
Airway obstruction is caused by:
Most commonly, excessive secretions (e.g., mucus plugs) or exudates within smaller bronchi, as may occur in bronchial asthma, chronic bronchitis, bronchiectasis, and postoperative states.
Aspiration of foreign bodies
rarely, fragments of bronchial tumors may also lead to airway
obstruction and atelectasis
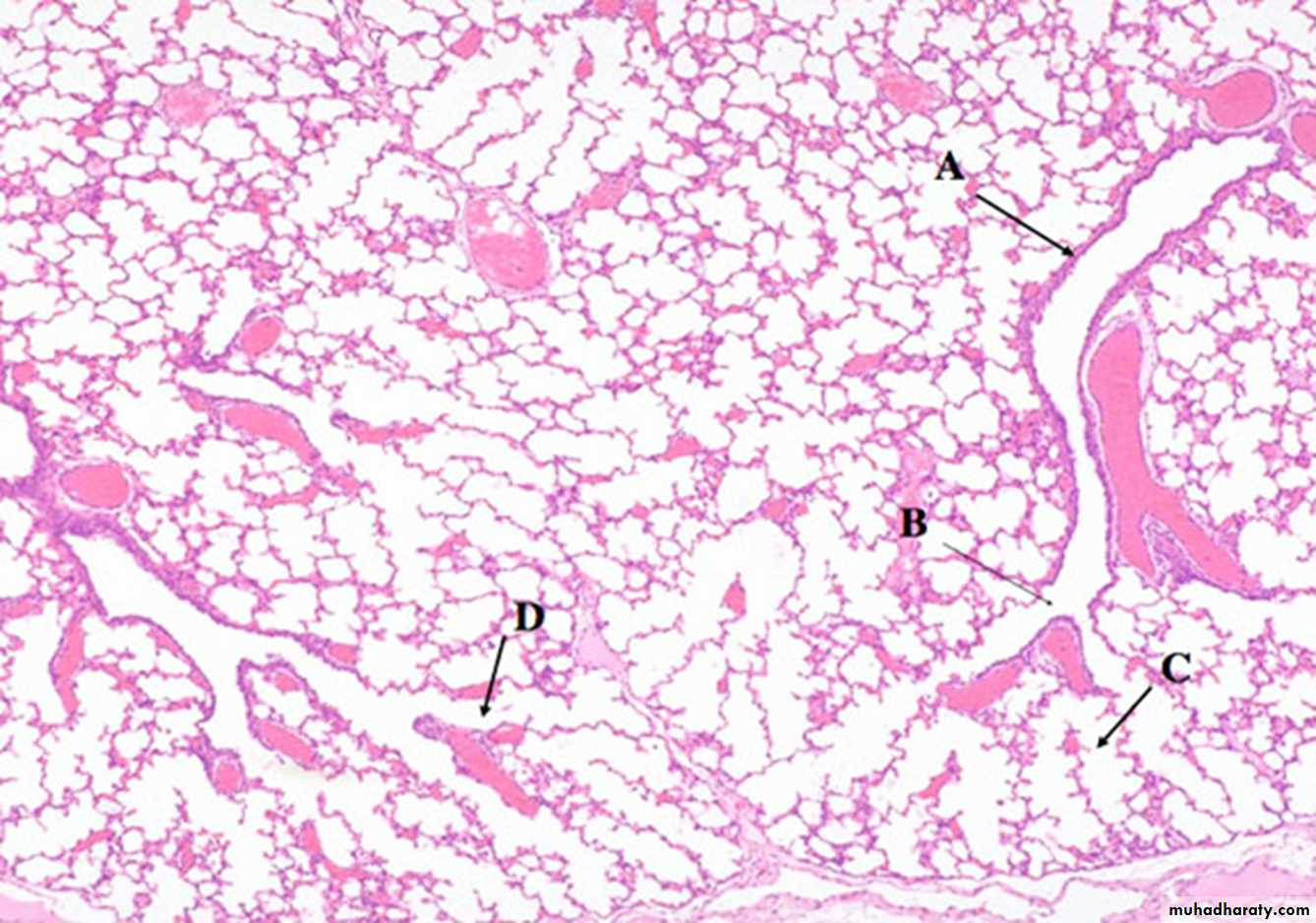
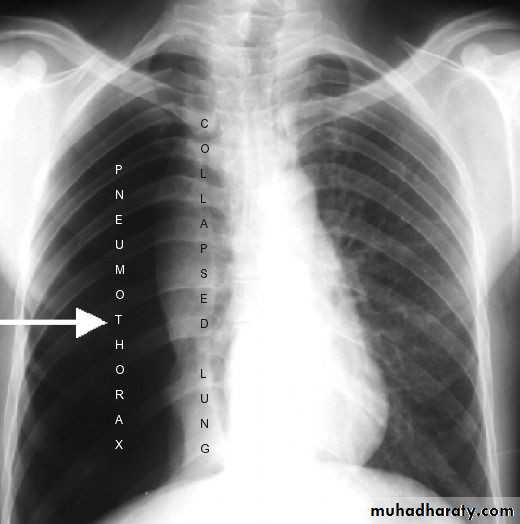
2- Compression atelectasis
results whenever significant volumes of fluid (transudate, exudate or blood), tumor, or air (pneumothorax) accumulate within the pleural cavity.With compression atelectasis, the mediastinum shifts away from the affected lung.
3-Contraction atelectasis
occurs when focal or generalized pulmonary or pleural fibrosis prevents full lung expansion.Which type of atelectasis is irreversible?
Contraction atelectasisEffects of atelectasis:
Hypoxemia due to decreased blood oxygenation and shunting of inadequately oxygenated blood from pulmonary arteries into the pulmonary veins.Superimposed infection of the collapsed lung.
CHRONIC OBSTRUCTIVE PULMONARYDISEASEDefinition
A clinical term used for a group of pathological conditions in which
there is chronic, partial or complete, obstruction to the airflow at any level from trachea to the smallest airways resulting in functional disability of the lungs.
One etiologic factor which is a common denominator in all forms of COPD is smoking.
The following entities are included in COPD:I. Chronic bronchitis
II. Emphysema
III. Bronchial asthma
IV. Bronchiectasis
V. Small airways disease (bronchiolitis)
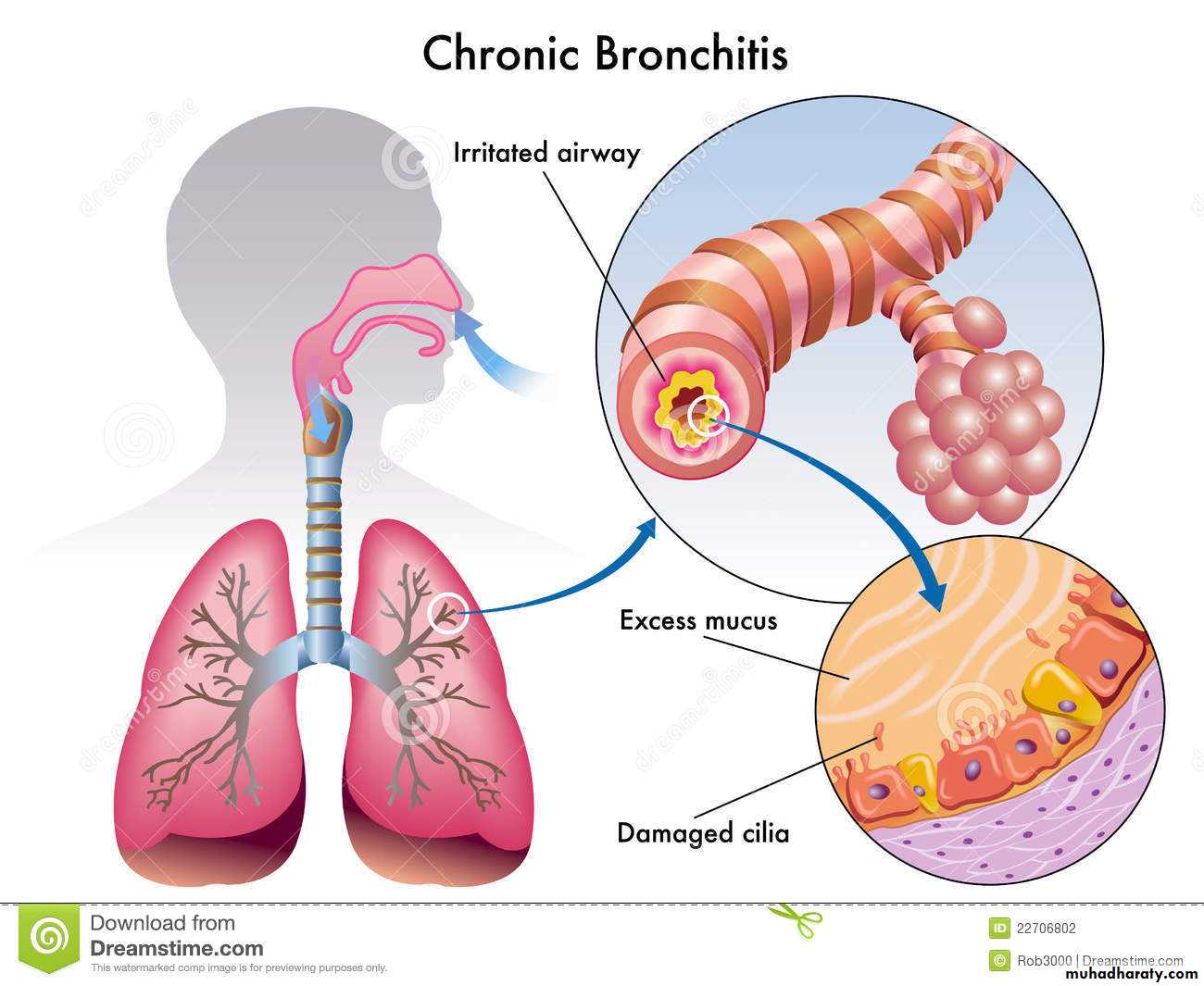
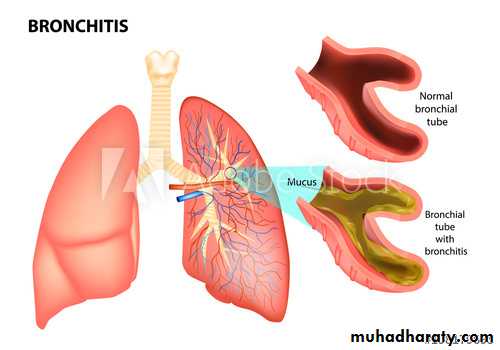
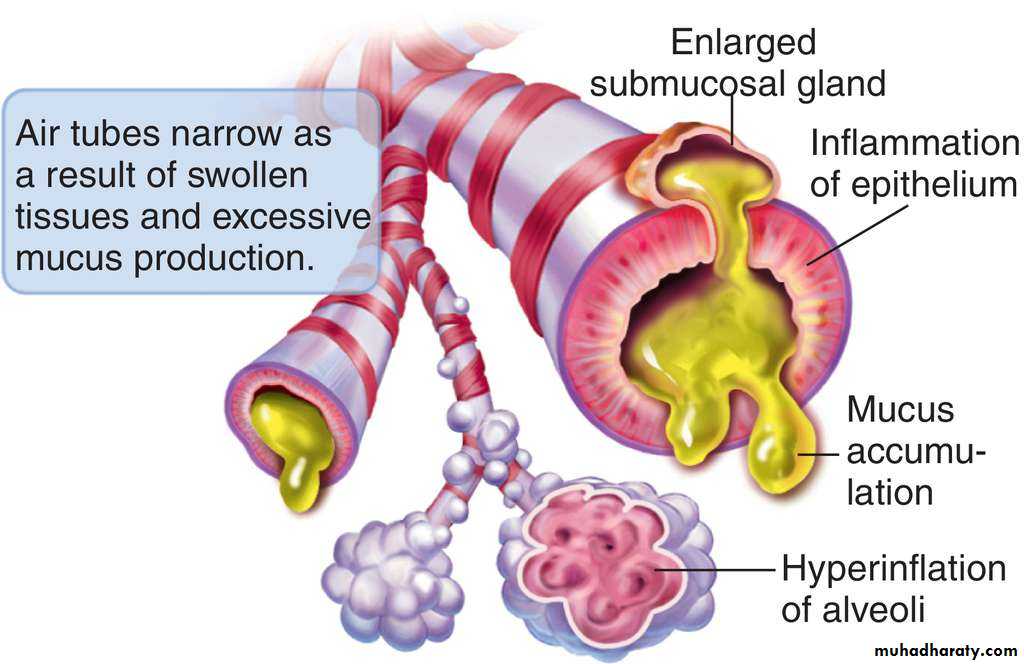
1- chronic bronchitis
Definition
persistent productive cough for at least three months of the year, for two or more consecutive years due to over secretion of mucus.
more common in middle-aged males
Frequently associated with emphysemapathogenesis
The two most important etiologic factors responsible for majority of cases of chronic bronchitis are:• cigarette smoking
• atmospheric pollution.
Other contributory factors are:
• occupation
• Infection
• familial and genetic factors.
Inhalation of irritant will induce hypersecretion of the bronchial mucus glands with excessive mucus production.
Chronic exposure to cigarette smoke results in damage to bronchioles,squamous metaplasia with resultant inflammation, fibrosis, and narrowing.
Cigarette smoke predisposes to infection lead to acute exacerbation in chronic bronchitis.
Irritated airway
Morphology:Hypertrophy and hyperplasia of submucosal mucous glands.
The overlying epithelium frequently shows squamous metaplasia which may be followed by dysplastic changes.chronic inflammatory cells are seen in the mucosa.
Complications:Respiratory failure.
Right Sided heart failure ( core pulmonale).
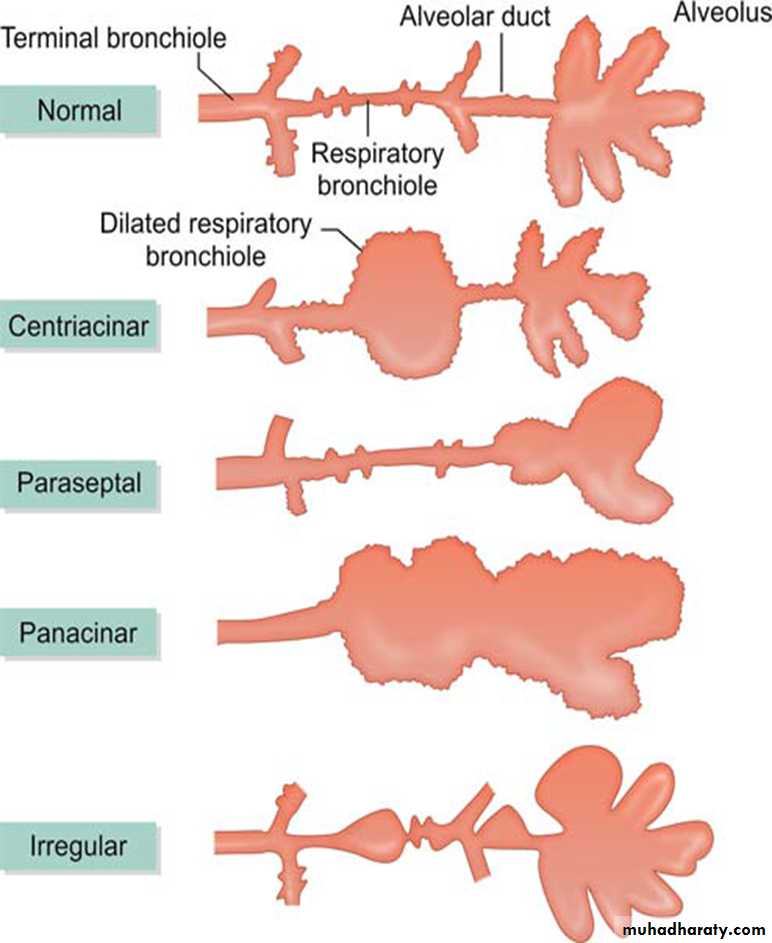
2- Emphysema
Definitionirreversible permanent dilatation of air spaces distal to the terminal bronchioles accompanied by destruction of their walls .
Q: Dilatation of air spaces without destruction is called……………………..
Thus, emphysema is defined morphologically, while chronic bronchitis is defined clinically.Types of emphysema
Types of emphysema
Emphysema is classifed according to the anatomic distribution into four major types:1. Centriacinar (centrilobular) emphysema
(a) Affects central or proximal part of acini and spares the distal part .(b) More common in upper lobes
(c) Predominantly seen in heavy smokers in association with chronic bronchitis
(d) May coexist with coal worker’s pneumoconiosis (walls of emphysematous spaces
demonstrate large amounts of pigment)
(e) Peribronchial and bronchiolar spaces commonly show inflammation
2. Panacinar (panlobular) emphysema
(a) Acini are uniformly enlarged from the level of respiratory bronchiole to terminal
blind alveolar sac
(b) More common in lower zones and anterior margin of lungs. Most severe at the bases
(c) Associated with a-1 antitrypsin (a-1 AT) deficiency
3. Paraseptal (distal acinar)
(a) Distal part of acinus is involved; proximal part is normal(b) Localized along pleura and perilobular septae
(c) Usually seen in upper part of lungs; adjacent to areas of fibrosis and atelectasis
(d) Spontaneous pneumothorax is a common complication
(e) Characteristic finding is presence of multiple, continuous and enlarged airspaces 0.5–2 cm, forming cyst-like structures.
4. Irregular (paraseptal) emphysema
(a) Irregular involvement of acinus(b) Usually asymptomatic and clinically insignificant
Others Types of Emphysema
Sometimes the term ‘emphysema’ may be applied to certain conditions not conforming strictly to the definition of emphysema.1. Compensatory emphysema: Dilatation of alveoli without destruction of septal walls
in response to loss/removal of lung substance elsewhere2. Obstructive overinflation: Expansion of lung because of air trapped within it. Trapping
of air may be due to Subtotal obstruction: Air enters in inspiration but cannot exit in expiration (ball valve mechanism)
3. Bullous emphysema:
(a) A form of emphysema that produces large sub pleural bullae (blebs . 1 cm in size),
rupture of which may lead to pneumothorax
(b) Usually a consequence of old tuberculosis scarring
4. Interstitial emphysema
(a) Characterized by air entry into connective tissue stroma of lung, mediastinum or
subcutaneous tissue
(b) Causes include an alveolar tear caused by bronchiolar obstruction accompanied by
explosive coughing (whooping cough, bronchitis, etc.) or puncture of the lung due
to a chest wound or a fractured rib
Pathogenesis of Emphysema
Role of ‘Protease–antiprotease’ mechanism:
protease These enzymes responsible for degradation of proteins , present inside neutrophils and macrophages, they are released during certain conditions as during inflammation.
Anitprotease α1- antitrypsin, this is a glycoprotein that is synthesized by the liver and is present in the serum and tissue fluids.
It is the major inhibitor of proteases and is encoded by a gene present on chromosome 14.
Role of Oxidant-antioxidant mechanism:
Neutrophils are a source of:• Oxygen-derived free radicals (inactivate native antiproteases by oxidative injury)
Pathogenesis of alveolar wall destruction in
emphysema by protease-antiprotease mechanismCauses of emphysema?
Smokingα1- antitrypsin deficiency
Morphology:
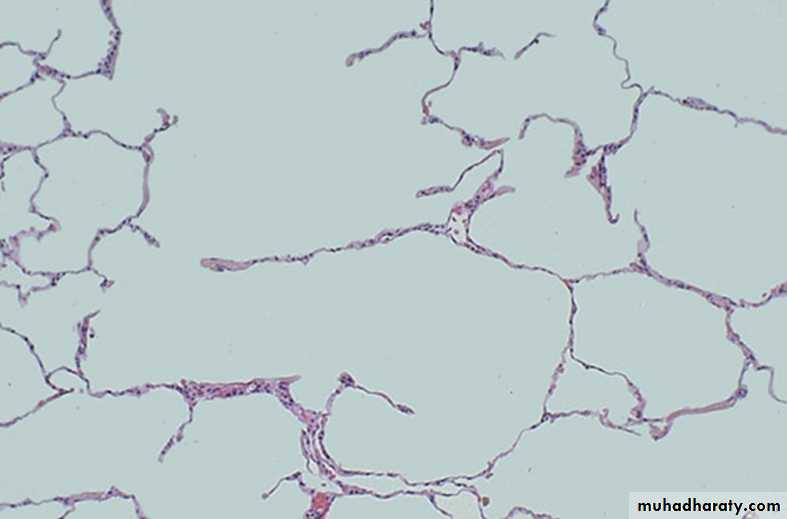
Microscopically there is thinning and destruction of alveolar septae with enlargement of air-spaces.3- Bronchial Asthma
DefinitionA chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, breathlessness, chest discomfort and cough particularly at night and/early morning.
It is associated with variable degree of :
Bronchoconstrictioninflammation of the bronchial walls
increased mucous secretion.
Types
1. Based on frequency and severity of symptoms(a) Mild intermittent
(b) Mild
(c) Moderate
(d) Severe persistent
2. Based on response to steroids
(a) Steroid dependent(b) Steroid resistant
3. Based on initiating factors
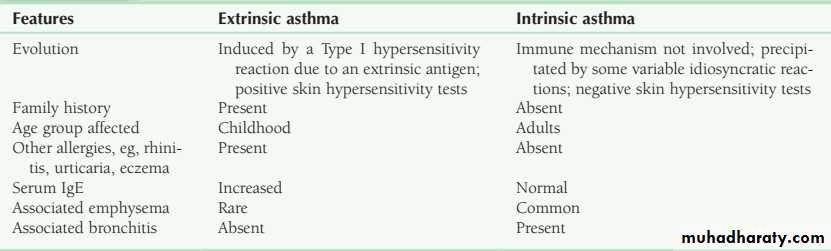
(a) Extrinsic: Induced by an extrinsic antigen and initiated by a Type 1 hypersensitivity reaction
(b) Intrinsic: Initiated by diverse nonimmune mechanisms, eg cold, stress, exercise, precipitated by several factors unique to the patient
4. Based on aetiology
(a) Atopic asthma (Type 1 IgE-mediated response triggered by environmental allergens like food, dust, pollen, animal dander; most common type of asthma; begins in childhood; positive family history and skin reaction)(b) Nonatopic asthma (No identifiable causative external agents; no family history or positive skin test, Triggering agents: respiratory tract infection)
morphology
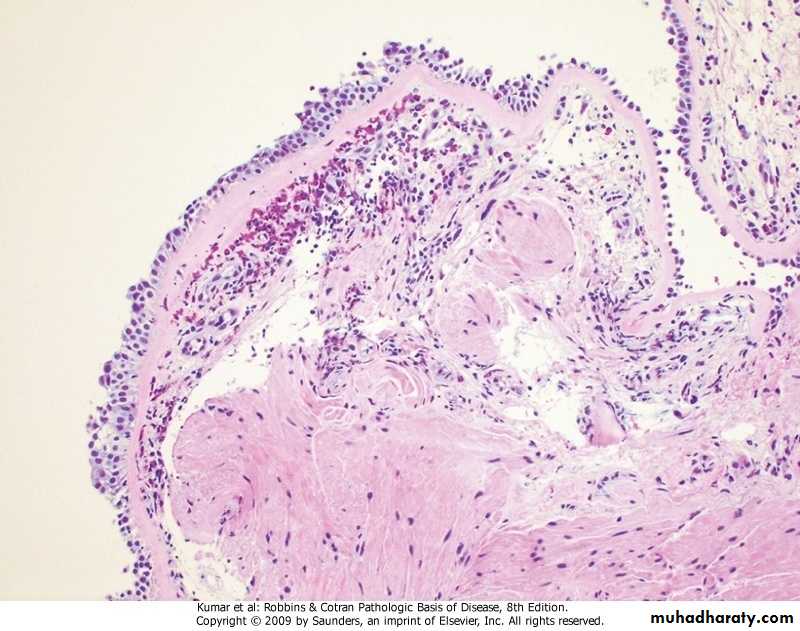
Grossly• Overinflated lungs with small areas of atelectasis• Occlusion of bronchi and bronchioles by thick tenacious mucous plugsMicroscopy• Thickening of basement membrane of bronchial epithelium• Oedema and inflammation in the bronchial walls (cells involved are eosinophils and mast cells)• Presence of Charcot–Leyden crystals (crystalloids made of eosinophil membrane protein)• Mucous plugs in bronchi and bronchioles containing whorls of shed epithelium (Curschmann spirals)• Increase in size of submucosal glands and hypertrophy of bronchial wall muscle
Pathogenesis
• Genetic predisposition to Type I hypersensitivity (atopy) and exposure to certain environmental triggers (inhaled allergens like house dust, mites, pets, etc., viruses like rhinovirus, air pollutants, smoking and drugs like beta adrenergic blockers and aspirin) induce bronchial hyper-responsiveness leading to acute and chronic airway inflammation.• TH2 cells induce bronchial inflammation and secrete cytokines like:
interleukin-4 (which stimulates B cells to produce IgE)
interleukin-5 (which activates eosinophils)
interleukin-13 (which stimulates mucous secretion from bronchial submucous glands)
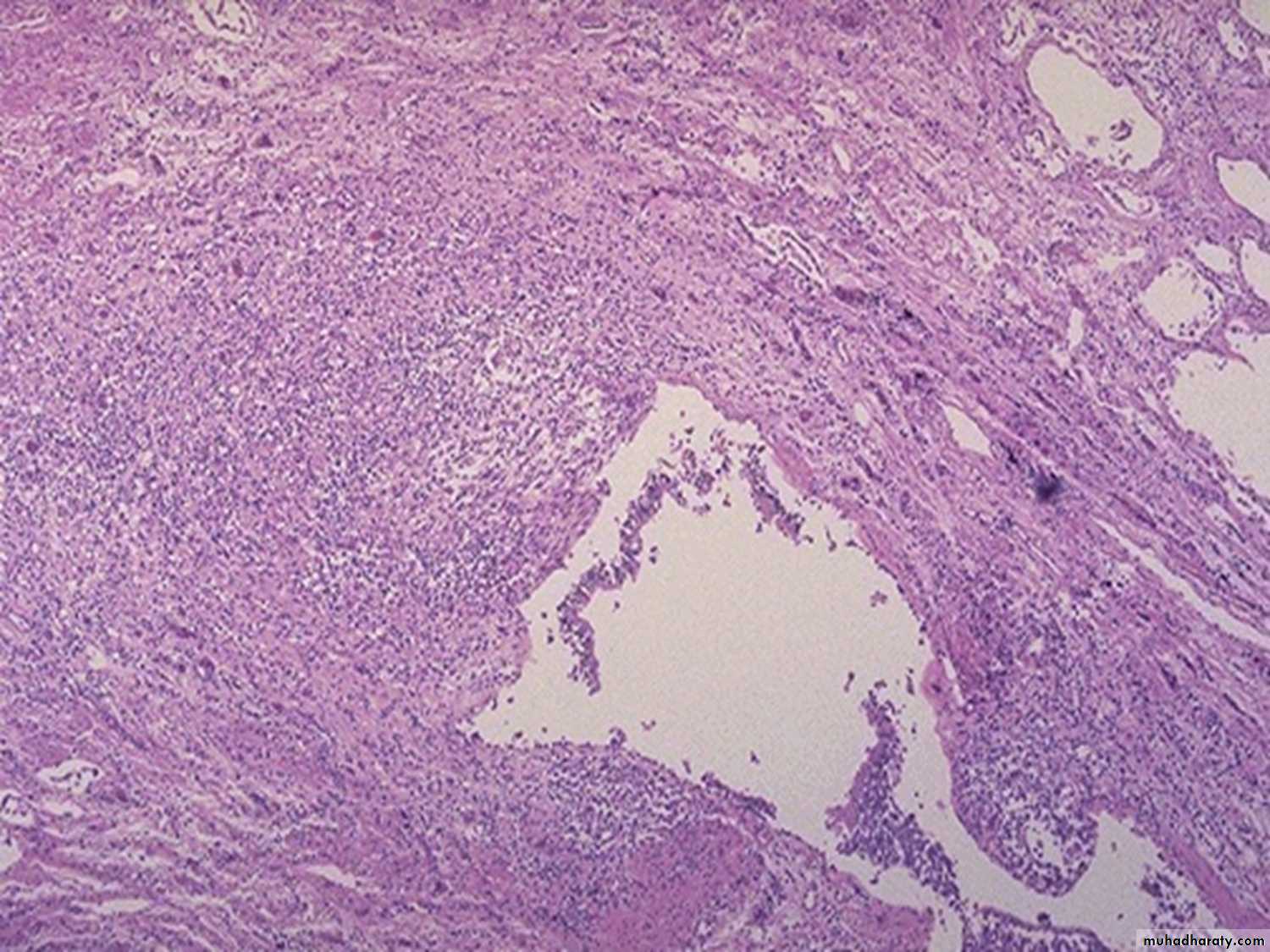
Bronchial asthma, sub-basement membrane fibrosis, eosinophilic inflammation, muscle hypertrophy
Q. Differentiate between extrinsic and intrinsic asthma
Respiratory infection
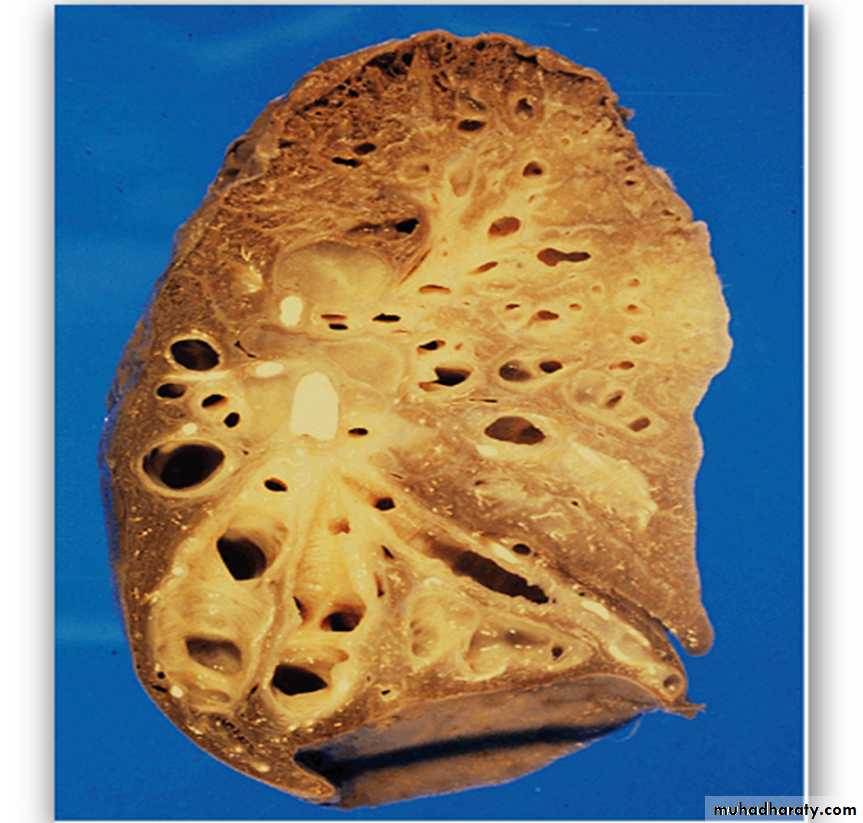
4- BronchiectasisDefinitionAbnormal permanent dilatation of bronchi and bronchioles as a result of destruction of the muscular and elastic components of their walls.
Causes• Congenital
Acquired• Cystic fbrosis (CF): Bronchiectasis associated with CF is secondary to mucous plugging of proximal airways and chronic pulmonary infection, especially with P. aeruginosa.
• Primary ciliary dyskinesia: It presents with immotile or dyskinetic cilia and/or sperms. This may lead to poor mucociliary clearance, recurrent pulmonary infections
and ultimately, bronchiectasis.
A variant of this condition, initially described by Kartagener, comprises the clinical triad of situs inversus, nasal polyps, sinusitis and bronchiectasis due to immotile cilia of the respiratory tract.
• Acquired bronchiectasis
• Primary infections: Bronchiectasis may result as a consequence of necrotizing infections that are either poorly treated or not treated at all.• Bronchial obstruction: Endobronchial tumours, foreign body impaction, right middle lobe syndrome (results from an abnormal angulation of the lobar bronchus at its origin, predisposing it to obstruction)
Morphology
- Grossly
the lungs may be involved diffusely or segmentally. Bilateral involvement of lower lobes occurs most frequently, more severe in distal airways
widely dilated bronchi
thickening of the bronchial walls
collapse and fibrosis of the parenchyma
Microscopically
1) bronchial epithelium normal, ulcerated or show squamous metaplasia.2) bronchial wall shows acute and chronic inflammatory cells and destruction of muscle and elastic tissue with fibrosis.
3) The intervening lung parenchyma shows fibrosis , while the surrounding lung tissue shows changes of interstitial pneumonia.
4) pleura in the affected area is adherent and shows bands of fibrous tissue between the bronchus and the pleura.
Complications:
Respiratory insufficiencyCor pulmonale
Brain abscesses
Amyloidosis
Restrictive pulmonary disease
DefinitionGroup of diffuse lung disease characterized by reduced expansion of lung parenchyma with decreased total lung capacity.
Restrictive lung disease includes 2 types of conditions:
A. chest wall disorder :1. Kyphoscoliosis
2. Severe obesity
3. Pleural diseases.
4. Neuromuscular disorders that affect the respiratory muscles.
B. interstitial lung diseases
INTERSTITIAL LUNG DISEASESThis is a group of lung diseases that characterized by reduce lung compliance ( i.e more pressure is needed to expand the lungs because they are stiff ).
No airway obstruction.
Classification of interstitial lung diseases (ILDs).
Acute interstitial lung disease:
It characterized by rapid onset of respiratory dysfunction and development of pulmonary edema.
Example adult respiratory distress syndrome (ARDS).
Chronic interstitial lung disease:
Characterized by insidious onset and the development of chronic inflammation and interstitial fibrosis.• WITH PREDOMINANT FIBROSIS Pneumoconiosis
• WITH PREDOMINANT GRANULOMATOUS REACTION Sarcoidosis• IMMUNOLOGIC LUNG DISEASES
• SMOKING-ASSOCIATED ILDs
• IDIOPATHIC
ACUTE RESPIRATORY DISTRESS SYNDROME
(ARDS)(HYALINE MEMBRANE DISEASE)
This is a syndrome that characterized clinically by rapid onset of respiratory distress and arterial hypoxemia, and pathologically by diffuse alveolar damage.
Neonatal ARDS
Adult ARDSCauses
a) Direct lung injury:
1. Diffuse pulmonary infections, chiefly viral pneumonia
2. Oxygen toxicity
3. Inhalation of toxins and irritants e.g. smoke, war gases, nitrogen dioxide, metal fumes etc.
4. Aspiration of gastric contents
5. Near drowning
b) Indirect lung injury:
1. Shock due to sepsis, trauma, burns2. Narcotic overdose
3. Pancreatitis
4. Drugs e.g. salicylates, colchicines
5. Fat embolism
6. Radiation
7. Multiple transfusions
PATHOGENESIS:
The conditions that lead to ARDS cause either endothelial or alveolar epithelial damage.Inflammatory cells will accumulate with subsequent release of powerful mediators ( like oxygen-derived free radicals, proteases, ….) which cause damage to the endothelium ( and/or alveolar epithelium) resulting in increased vascular permeability with subsequent edema
Morphology:
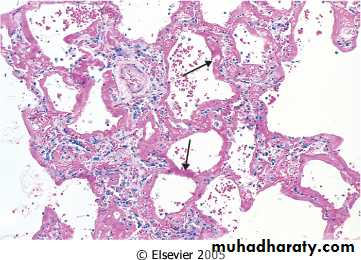
The most characteristic feature is formation of hyaline membrane lining the alveoli.
It consists of protein-rich edema fluid and necrotic epithelial cells.• Early phase of diffuse alveolar damage (DAD). There are hyaline membranes, lining alveoli. High oxygen tensions needed to treat the hypoxia resulting from DAD and its etiologies further potentiates this disease.
Clinically:
The most important feature is dyspnea with severe acute respiratory failure, hypoxemia, and multiorgan failure.Mortality rate may reach 50%.
Chronic restrictive lung disease with predominant fibrosisPNEUMOCONIOSES
A group of chronic fibrosing diseases of the lung resulting from exposure to organic and inorganic particulates, most commonly mineral dust.
inhalation of mineral dusts, mostly at work, therefore also called occupational lung diseases.
The four most common types of pneumoconioses result form exposure to:
• Exposure• Disease
• Agent
• Coal mining
• Anthracosis
• Simple coal worker pneumoconioses (macule).
• Progressive massive fiborsis.
• Coal dust
• Foundry work, sandblasting, hardrock mining, stone cutting,…
• Silicosis
• Silica
• Mining, milling, and fabrication; installation & removal of insulation
• Asbestosis, pleural effusion & plaque, mesothelioma, carcinoma of the lung, larynx, stomach, colon.
• Asbestos
• Mining, fabrication
• Berylliosis
• Beryllium
The type of lung diseases varies according to the nature of inhaled dust . Some dusts are inert and cause no reaction and no damage , while other cause immunological damage & may predispose to T.B or neoplasm
Factors which determined the extent of damage:
Size and shape of particles especially 2-5 µmTheir solubility and physio–chemical characters
The amount of dust retained in the lungsThe additional effect of other irritants such as tobacco smoke
Host factor such as efficiency of clearance mechanism and immune status of the host .Anthracosis & coal worker pneumoconiosis :
Simplest forms of pneumoconiosis , usually universal , harmless , rarely it may progress to progressive massive fibrosis.Silicosis :
May be encountered in sandblasting, mining, stone cutting, tunneling, ceramics…..
It induces progressive inflammation lead to the formation of fibrotic masses .
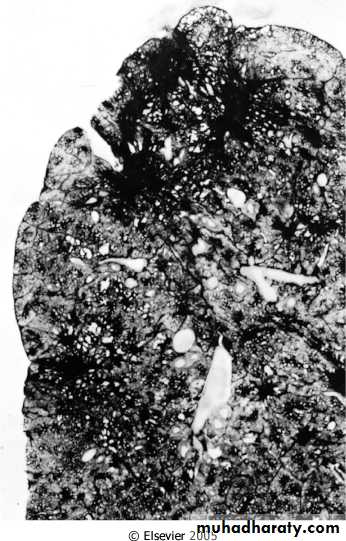
It may associated with increased susceptibility to T.B & lung cancer.Morphology
-Gross, fibrotic nodules and scars in the upper zones of the lungs.Fibrotic lesions may also occur in the hilar lymph nodes and pleura.
-Microscope, concentric layers of hyalinized collagen.
Collagenous silicotic nodule
Chronic restrictive lung disease with predominant granulomatous reaction
Sarcoidosis
Definitions:
It is a multisystem disease of unknown etiology characterized by non-caseating granulomas in many tissues and organs. It is one of the cases of interstitial (restrictive) lung diseases.
Epidemiology:
Affects adults of both sexes.It is more common in black people.
High prevalence among non-smokers.Shows familial and racial clustering and association with certain HLA as HLA-A1 & HLA-B8.
Etiology & pathogenesis:
The etiology remains unknown.Evidence suggest that it is a disease of disordered immune regulation (cell mediated immune response to unidentified antigen ) in genetically predisposed individuals exposed to certain environmental agents.
The process is driven by CD4 helper/inducer T-cells, which accumulate in the pulmonary interstitium, secrete cytokines (as IL-2 and interferon-γ), resulting in T-cell expansion and macrophage activation.
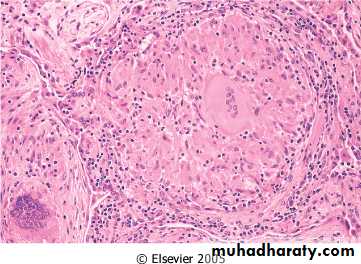
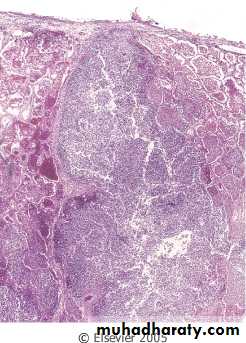
Morphology:
The histological hallmark of sarcoidosis is the presence of non-caseating epithelioid granuloma, irrespective of the organ involved.
WHAT is granuloma?
These are nodular collection of epithelioid histiocytes, rimmed by an outer zone of lymphocytes (CD4 helper). Scattered multinucleated giant cell may be seen. More peripherally, a layer of fibroblasts is present, which proliferate and lay down collagen that replace the granuloma.Organs involved:
Lungs: In 90% of cases. Multiple granulomas in the interstitium ending in interstitial fibrosis and development of core plumonale.Lymph nodes: 75-90% of cases. Intrathoracic and paratracheal lymph nodes. In 30% of cases peripheral lymph nodes.
Skin involvement: erythema nodosum and subcutaneous nodules.
Eye and lacrimal glands involvement: iritis and iridocyclitis (causing corneal opacity and glaucoma), choroditis, retinitis, and optic nerve involvement (blindness). Inflammation of the lacrimal glands may suppress lacrimation (sicca syndrome).Salivary glands: Painful enlargement of the parotid glands and may leads to xerostomia (dry mouth).
Hepatic, splenic, and bone marrow involvement.
Virtually any organ may be involved such as the heart.Clinical course:
Asymptomatic and discovered accidentally by routine chest x-ray (hilar LN enlargement).Respiratory symptoms ( cough, dyspnea,..)
Peripheral lymphadenopathy, cutaneous lesions, eye involvement, or heptosplenomegally.Constitutional symptoms as fever, fatigue, weight loss,…
Diagnosis:Demonstration of non-caseating granuloma in lung or lymph node biopsy.
However, other causes of granuloma as mycobacterial and fungal infection and berylliosis have to be rolled out.Prognosis:
Progressive chronic course with episodes of relapse and remission.
60-70% of patients recover (steroid therapy) with no residual manifestations.20% develop permanent lung dysfunction or visual impairment.
Vascular lung diseases• Diseases of the heart affect the lungs and diseases of the lungs affect the heart.
• This is because of the peculiar characteristics of pulmonary vasculature.• The pressure in the pulmonary arteries is much lower than in the systemic arteries.
• General diseases of vascular origin occurring in the lungs
Pulmonary hypertension
Definition :Elevated systolic blood pressure in the pulmonary arterial circulation above 30 mmHg.
Types:
primary (idiopathic)
secondary; more common may be due to
Passive pulmonary hypertension due to diseases that passively raise pressure in the pulmonary veins.
hyperkinetic (Reactive) pulmonary hypertension due to causes in which the blood enters the pulmonary arteries in greater volume or at a higher pressure circulation.
Vaso-occlusive pulmonary hypertension.
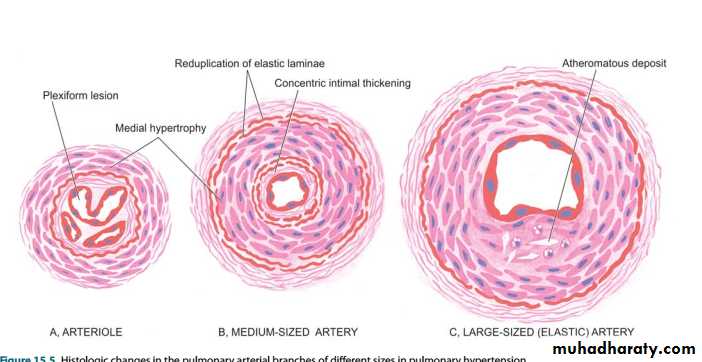
Histologic changes in the pulmonary arterial branches of different sizes in pulmonary hypertension.
PULMONARY INFECTIONS
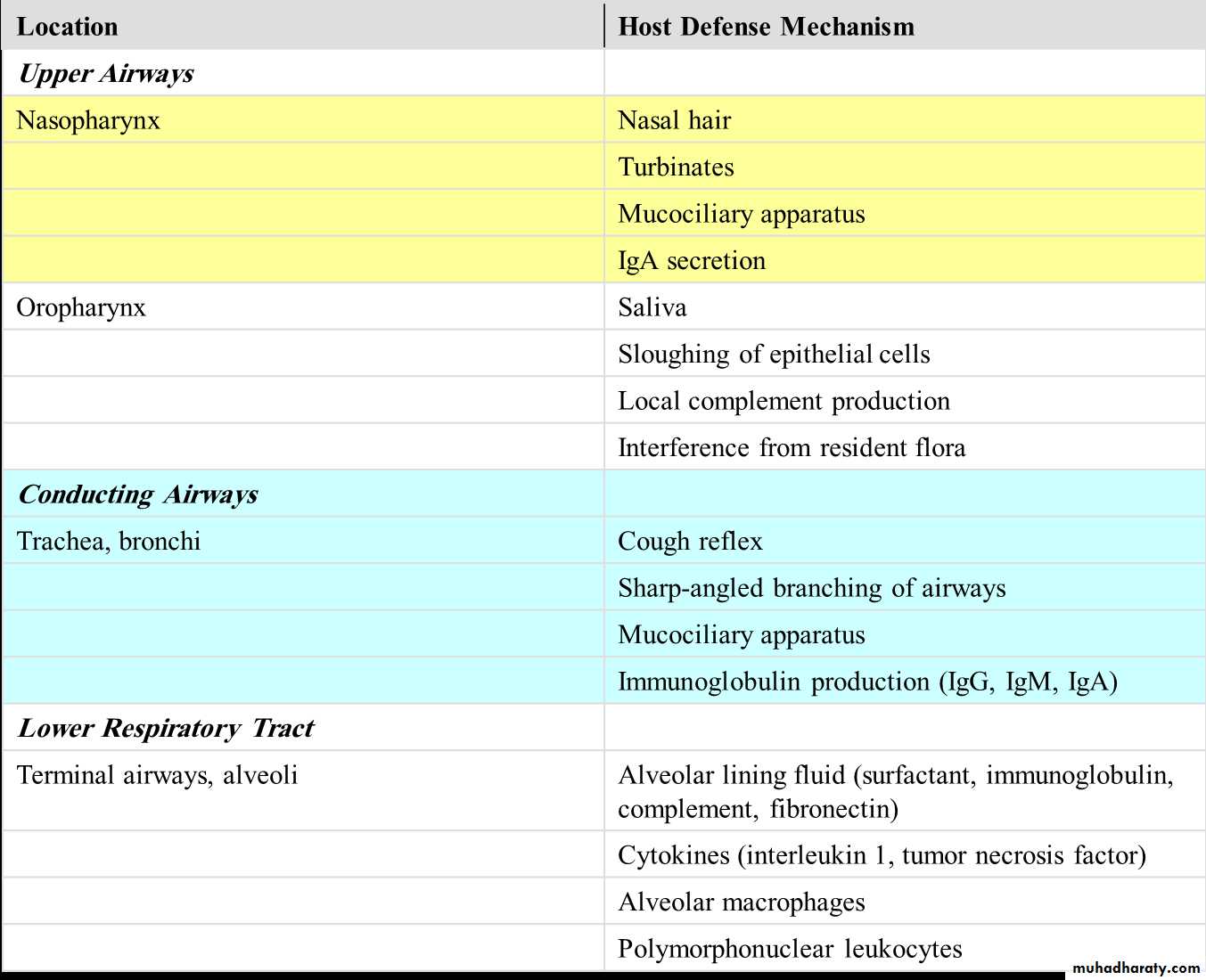
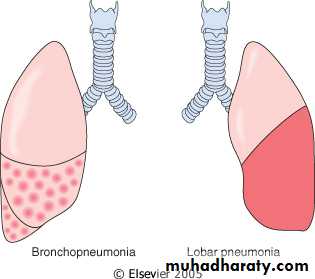
The normal lung is free of bacteria because of the presence of a number of lung defense mechanisms at different levels .Failure of these defense mechanisms result in pneumonias. These conditions are as under:
1. Altered consciousness The oropharyngeal contents may be aspirated in states causing unconsciousness e.g. in coma2. Depressed cough and glottic reflexes allow aspiration of gastric contents e.g. in old age, pain from trauma or thora co abdo minal surgery, neuromuscular disease
3. Impaired mucociliary transport cigarette smoking, viral respiratory infections, immotile cilia syndrome, inhalation of hot or corrosive gases and old age.
4. Impaired alveolar macrophage function Pneumonias may occur when alveolar macrophage function is impaired e.g. by cigarette smoke, hypoxia, starvation, anaemia, pulmonary oedema and viral respiratory infections.
5. Endobronchial obstruction The effective clearance mechanism is interfered in endobronchial obstruction from tumour, foreign body, cystic fbrosis and chronic bronchitis.
6. Immunocompromised states Disorders of lymphocytes including conge nital and acquired immunodefciencies
Pneumonia
Definition
Inflammation of the lung parenchyma distal to the terminal bronchioles
Pathogenesis
The microorganisms gain entry into the lungs by one of the following four routes:1. Inhalation of the microbes present in the air.2. Aspiration of organisms from the nasopharynx ororopharynx.3. Haematogenous spread from a distant focus of infection.4. Direct spread from an adjoining site of infection
Classification of pneumonia
I. On the basis of the anatomic region of the lung parenchyma involved, pneumonias are traditionally classifed into 3 main types:1. Lobar pneumonia2. Bronchopneumonia (or Lobular pneumonia)3. Interstitial pneumonia.II. Based on the clinical settings in which infection occurred (pneumonia syndrome):
1. Community acquired Acute pneumonia
2. Community acquired Atypical pneumonia
3. Hospital-acquired pneumonia
4. Aspiration (inhalation) pneumonia
5. Chronic pneumonia
6. Pneumonia in an immunocompromised host
7. Necrotizing pneumonia and lung abscess
III. Based on etiology , pneumonias are classifed as :A. Bacterial pneumoniaB. Viral pneumoniaC. Pneumonias from other etiologies
Community acquired Acute bacterial pneumonia
Bacterial infection is the most common cause of pneumonia or consolidation of one or both lungs.Usually follows a viral upper respiratory tract infection.
The onset is usually abrupt, with high fever, shaking chills, pleuritic chest pain, and a productive mucopurulent cough.
Streptococcus pneumoniae (or pneumococcus) is the most common cause of community-acquired acute pneumonia.
Pneumococcal pneumonia:
Occurs with increased frequency in three groups of individuals. Those with:Chronic diseases such as congestive heart failure, COPD, or diabetes.
Congenital or acquired immunoglobulin defects.Absent splenic function (e.g., sickle cell disease or post splenectomy). WHY?
Morphology :Grossly
1. Broncho-pneumonia (lobular)
Implies a patchy distribution of inflammation that generally involves more than one lobe.
This pattern results from an initial infection of the bronchi and bronchioles with extension into the adjacent alveoli.
2. Lobar pneumonia
The contiguous airspaces of part or all of a lobe are homogeneously filled with an exudate that can be visualized on radiographs as a lobar or segmental consolidation.Streptococcus pneumoniae is responsible for more than 90% of lobar pneumonias.
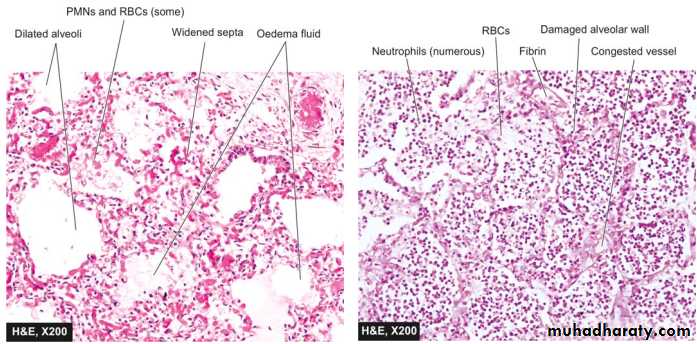
Microscopically
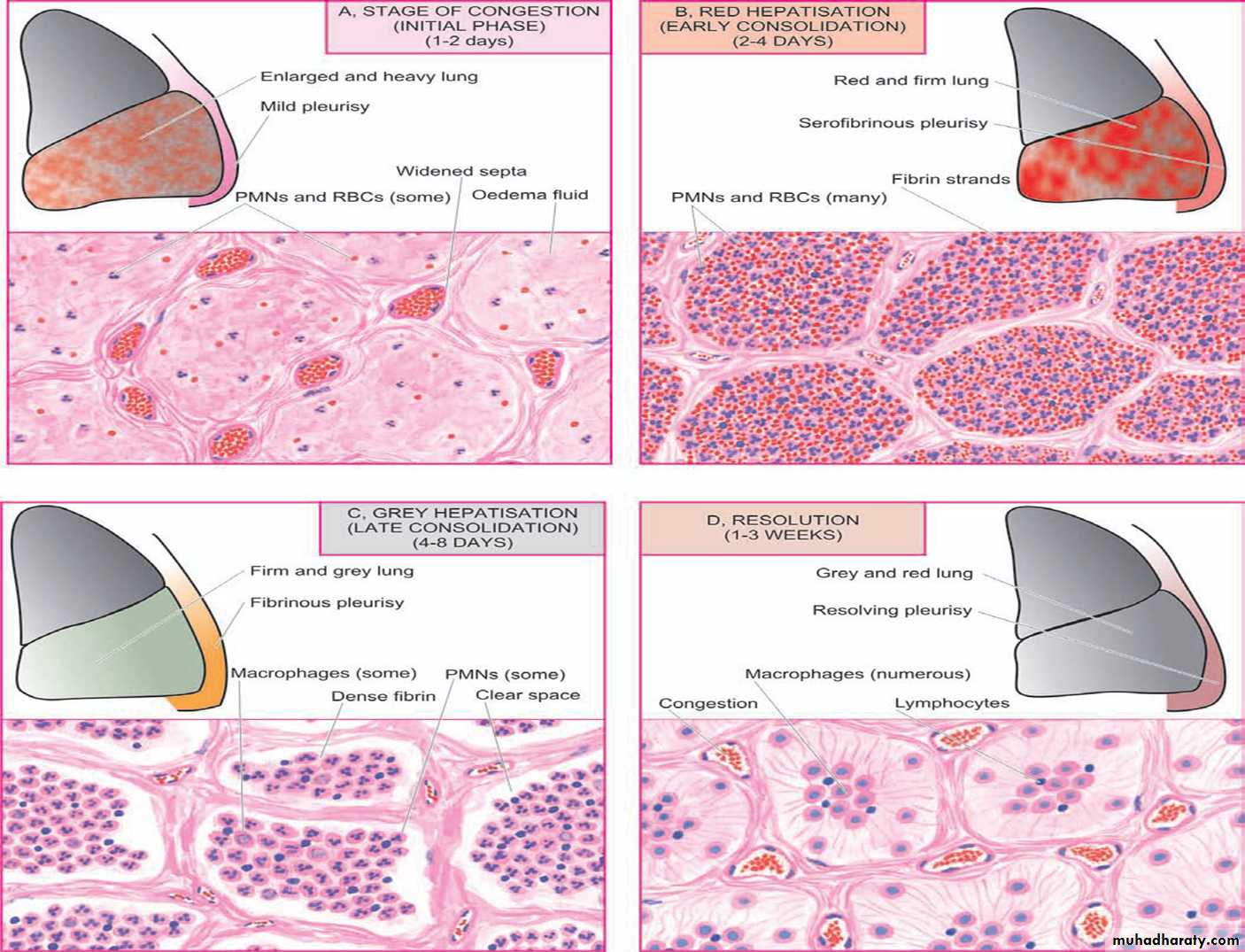
There are four pathological stages of Pneumococcal lobar pneumonia:Congestion.
Red hepatization.
Gray hepatization.
Resolution.
Early antibiotic therapy alters this typical progression.
Congestion:
Early stage, the affected lobe is heavy and red.
Histologically, vascular congestion can be seen, with proteinaceous fluid, scattered neutrophils, and many bacteria in the alveoli.Red hepatization
Ensues within few days, in which the lung lobe has a liver-like consistency; the alveolar spaces are packed with neutrophils, red cells, and fibrinGray hepatization:
Later on the lung appears dry, gray, and firm, because the red cells get lysed, while the fibrinous exudate persists within the alveoli.
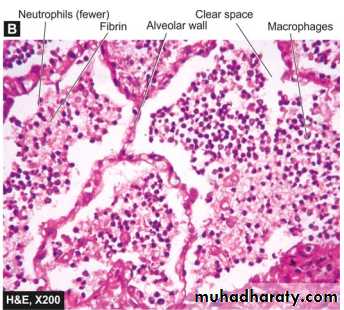
Resolution
follows in uncomplicated cases, as exudates within the alveoli are enzymatically digested and either resorbed or expectorated, leaving the basic architecture intact.Complications:
With appropriate therapy, complete restitution of the lung is the rule for both forms of pneumococcal pneumonia, but in occasional cases complications may occur include:Tissue destruction and necrosis may lead to abscess formation.
Suppurative material may accumulate in the pleural cavity, producing an empyema.Organization of the intra-alveolar exudate may convert areas of the lung into solid fibrous tissue.
Bacteremic dissemination may lead to meningitis, arthritis, or infective endocarditis.
Diagnosis:
• Clinical features.• Radiological examination.
• Gram stained sputum ( high false + result from normal flora).
• Isolation of pneumococci from blood cultures is more specific.
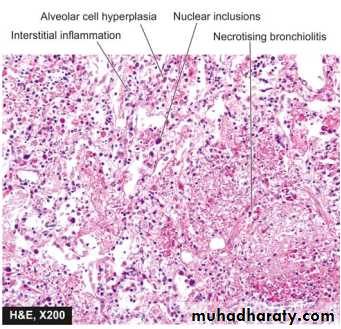
Community-Acquired Atypical Pneumonias
Modest sputum production.
There are no physical findings of consolidation.The white cell count is only moderately elevated.
Bacteria could not be isolated.Causes:
Mostly caused by Mycoplasma pneumoniae. Other agents, include viruses, chlamydiae, and rickettsiae.
Mycoplasma infections are particularly common among children and young adults. They occur sporadically or as local epidemics in closed communities (schools, military camps, prisons).
Pathogenesis:
In the alveoli, there is usually interstitial inflammation.Damage to the respiratory epithelium inhibits mucociliary clearance and predisposes to secondary bacterial infections.
NOSOCOMIAL (HOSPITAL-ACQUIRED) PNEUMONIA:
Defined as pulmonary infections acquired in the course of a hospital stay.Nosocomial infections are common in:
• Patients with severe underlying disease.
• Immunosuppression.• Prolonged antibiotic therapy.
• Patients with invasive access devices such as intravascular catheters.
• Patients on mechanical ventilation.
Causes:
Gram-negative rods (Enterobacteriaceae and Pseudomonas species) and S. aureus are the most common isolates.
ASPIRATION PNEUMONIA:
occurs in:Debilitated patients.
Aspiration of gastric contents either while unconscious (e.g., after a stroke) or during repeated vomiting.The resultant pneumonia is partly chemical, owing to the extremely irritating effects of the gastric acid, and partly bacterial.
Mostly caused by anaerobic bacteria, but recent studies implicate aerobes.
This type of pneumonia is often necrotizing, and abscess formation is a common complication.Lung abscess
Lung abscess refers to a localized area of suppurative necrosis within the pulmonary parenchyma, resulting in the formation of one or more large cavities.Causative agents:
Anaerobic bacteria are present in almost all lung abscesses.
Often there is a mixed anaerobic-aerobic infection; commonly S. aureus.
Infective abscesses occur in 10% to 15% of patients with bronchogenic carcinoma. Thus, when a lung abscess is suspected in an older patient, underlying carcinoma must be considered.
The causative organism may be introduced into the lung by any of the following mechanisms:
• Aspiration of infective material (from carious teeth, infected sinuses,oral surgery, anesthesia, coma, or alcoholic).
• Aspiration of gastric contents, accompanied by infectious organisms from the oropharynx.
• As a complication of necrotizing bacterial pneumonias, esp caused by Staphylococcus aureus, Streptococcus pyogenes, K. pneumoniae, Pseudomonas species, and, rarely, type 3 pneumococci.
• Bronchial obstruction, as in bronchogenic carcinoma.
• Septic embolism, from infective endocarditis of the right side of the heart.
• Hematogenous spread of bacteria ( especially staph)
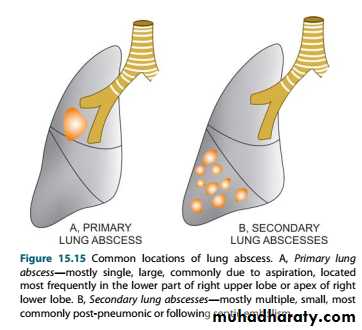
Morphology:
Size: variableSingle or multiple.
The localization and number of abscesses depend on their mode of development ( abscesses resulting from aspiration of infective material are common on the right side)Abscesses that develop in the course of pneumonia or bronchiectasis & those arising from hematogenous seeding are commonly multiple.
Microscopically
There is suppuration surrounded fibrous scarring and mononuclear infiltration.
Clinical Course.
Prominent cough yielding copious amounts of foul-smelling, purulent sputum; occasionally, hemoptysis occurs.Fever and malaise.
Clubbing of the fingers, weight loss, and anemia may all occur.Consequences & complications of lung abscess:
• Rupture into the airways, the contained exudate may be partially drained.• Rupture into the pleural cavity and produce pneumothorax or empyema.
• Embolization of septic material to the brain, giving rise to meningitis or brain abscess.
• Secondary amyloidosis may develop in chronic cases.