Periodontal ligament
Lec 2 periodontology forth stage Dr. gHayath al-jawadystructure of the periodontal fibers
• The periodontal ligament is the connective tissue that surrounds the root and connects it with the bone.• It is continuous with the connective tissue of the gingiva and communicates with the marrow spaces through vascular channels in the bone.
• the average width is
about 0.2 mm
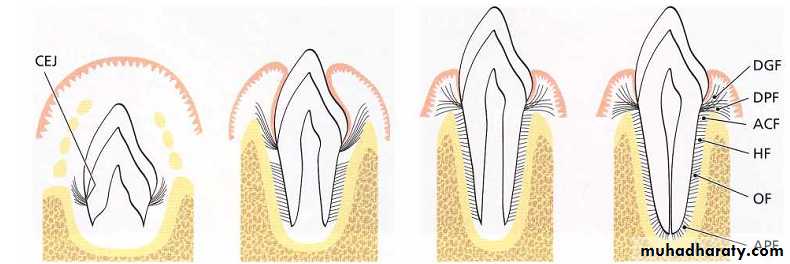
DEVELOPMENT OF PRINCIPAL FIBERS The tooth bud is formed in a crypt of the bone. The collagen fibers produced by the fibroblasts in the loose connective tissue around the tooth bud , during the process of their maturation, embedded into the newly formed cementum immediately apical to the CEJ.These fiber bundles oriented towards the coronal portion of the bony crypt will later form the dent0gingival fiber groups.
First, fibers can be identified entering the most marginal portion of the alveolar bone. Later, more apically positioned bundles of oriented collagen fibers are seen.The orientation of the collagen fiber bundles alters continuously during the phase of tooth eruption. The fibers of the periodontal ligament associate into groups of well-oriented dentoalveolar collagen fibers.
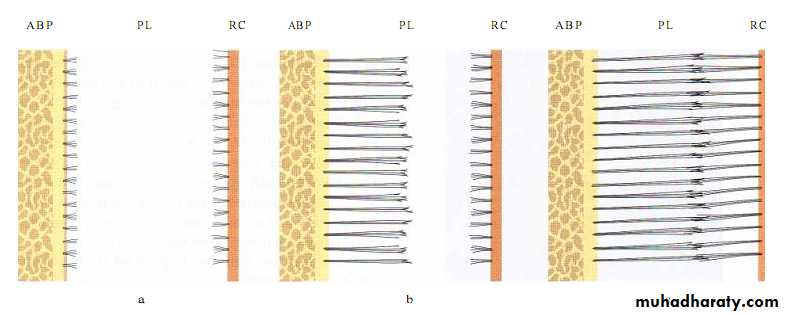
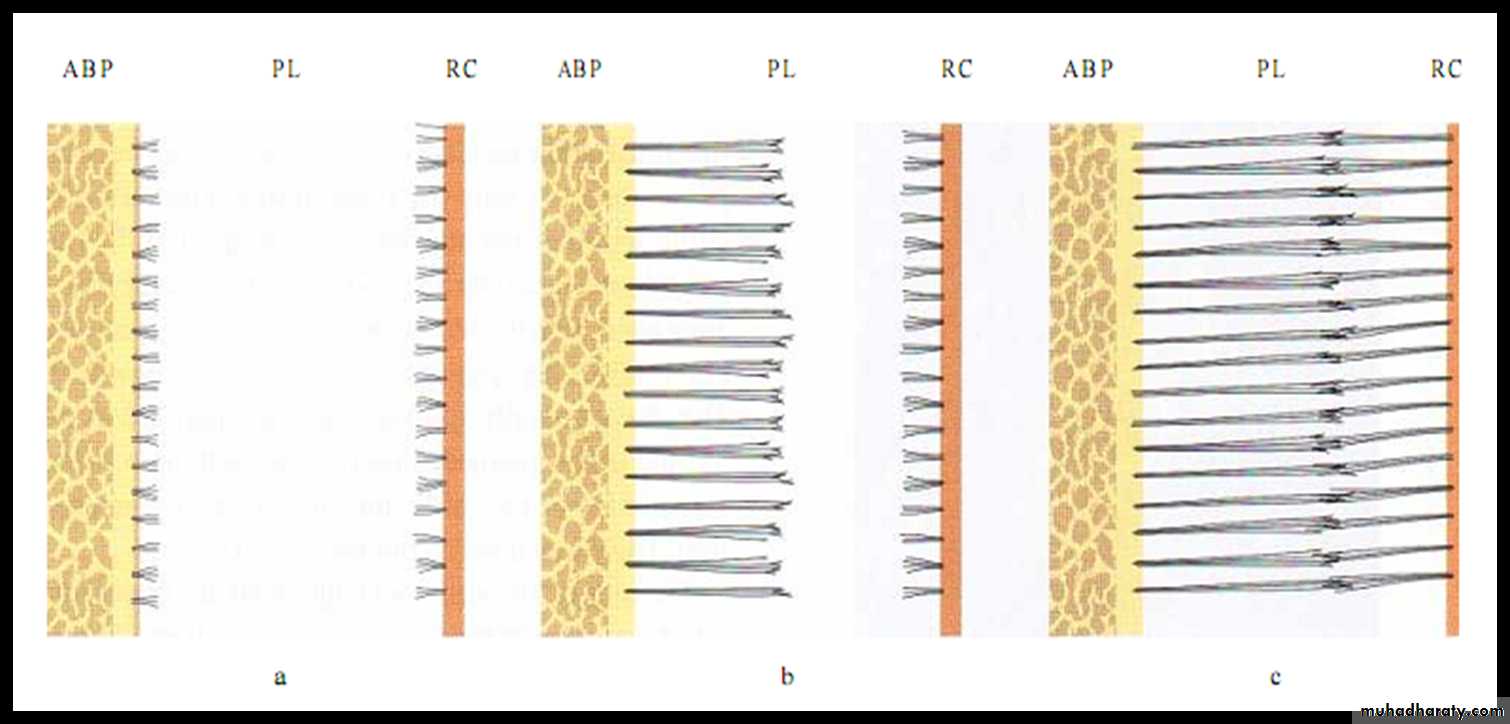
This schematic drawing illustrates the development of the principal fi bers of the periodontal
ligament. The alveolar bone proper (ABP) is seen to the left, the periodontal ligament (PL) is depicted
in the center and the root cementum (RC) is seen tothe right.
How principle f.develop ?
First, small, fine, brush-like fibrils are detected arising from the root cementum and projecting into the PL space. At this stage the surface of the bone is covered by osteoblasts. From the surface of the bone only a small number of radiating, thin collagen fibrils can be seen.
How principle f.develop ?
Later on, the number and thickness of fibers entering the bone increase. These fibers radiate towards the loose connective tissue in the mid-portion of the periodontal ligament area (PL), which contains more or less randomly oriented collagen fibrils. The fibers originating from the cementum are still short while those entering the bone gradually become longer. The terminal portions of these fibers carry finger-like projections.
How principle f.develop ?
The fibers originating from the cementum subsequently increase in length and thickness and fuse in the periodontal ligament space with the fibers originating from the alveolar bone. When the tooth, following eruption, reaches contact in occlusion and starts to function, the principal fibers become organized in bundles and run continuously from the bone to the cementum.
Intermediate plexus (indifferent f. plexus)
Individual f.has 2 separate part one of them is spliced with other ,after eruption; the f. arranged well but not embedded in C.& boneTerminal portions of principal fibers that insert into cementum and bone are termed as Sharpey’s fibers. The principal fibers embedded in the cementum have a small diameter but are more numerous than those embedded in the alveolar bone proper. In addition to these fiber types, small collagen fibers associated with larger principal fibers have been called as “Indifferent fiber plexus of Shefforfold” Development…
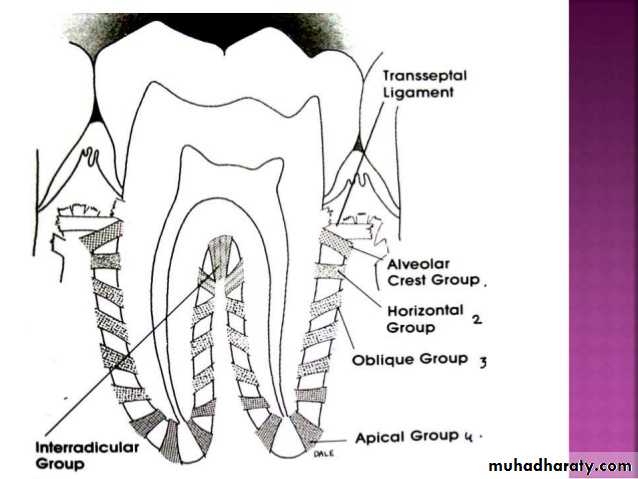
Principal fibers of the periodontal ligament
Alveolar crest group. Alveolar crest fibers extend obliquely from the cementum
just beneath the junctional epithelium to the alveolar crest. Fibers also run fromthe cementum over the alveolar crest and to the fibrous layer of the periosteum
covering the alveolar bone. The alveolar crest fibers prevent the extrusion of the
tooth and resist lateral tooth movements. The incision of these fibers during
periodontal surgery does not increase tooth mobility unless significant
attachment loss has occurred.
Horizontal group. Horizontal fibers extend at right angles to the long axis of the
tooth from the cementum to the alveolar bone.
Oblique group. Oblique fibers, the largest group in the periodontal ligament,
extend from the cementum in a coronal direction obliquely to the bone. They
bear the brunt of vertical masticatory stresses and transform them into tension
on the alveolar bone.
Apical group. The apical fibers radiate in a rather irregular manner from the
cementum to the bone at the apical region of the socket. They do not occur on
incompletely formed roots.
Interradicular group. The interradicular fibers fan out from the cementum to the
tooth in the furcation areas of multirooted teeth.
Types of cells in the periodontal ligament Cellular Elements
Four types of cells have been identified in the PL:• connective tissue cells
• epithelial rest cells
• defense cells
• cells associated with neurovascular elements.
• Connective tissue cells include fibroblasts, cementoblasts, osteoblasts, osteoclasts, and odontoclasts.
These cells synthesize collagen and have also been shown to possess the capacity to phagocytose "old“ collagen fibers and degrade them by enzyme hydrolysis.
• The epithelial rests of Malassez form a latticework in the periodontal ligament and appear as either isolated clusters of cells Epithelial rests proliferate when stimulated, and participate in the formation of periapical cysts and lateral root cysts.
• The defense cells include macrophages, mast cells, and eosinophils
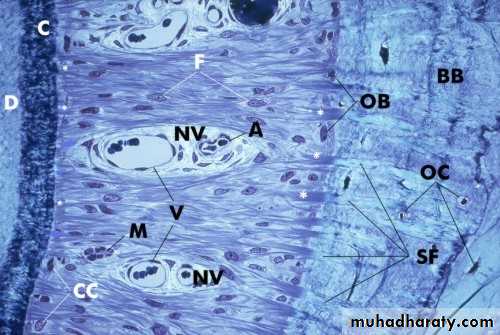
Histological cross-section through a periodontal ligament
A, arteriole; BB, bundle bone; C, cementum; CC, cementocytes; D,dentin; F, fibroblasts; M, cell rests of Malassez; NV, neurovascular
channel; OB, osteoblasts; OC, osteocytes; SF, Sharpeys fibers; V,
thin-walled venules.
Ground Substance:components of the ground substance
It consists of two main components:
glycosaminoglycans such as hyaluronic acid and
proteoglycans, and glycoproteins such as fibronectin and laminin It also has a high water content (70%).
The periodontal ligament may also contain
calcified masses called cementicles, which are adherent to or detached from the root surfaces
Functions of the periodontal ligament
• Physical Function• Formative and Remodeling Function
• Nutritional and Sensory Functions
Physical Functions
• Provision of a soft tissue "casing" to protect the vessels and nerves from injury by mechanical forces.• Transmission of occlusal forces to the bone.
• Attachment of the teeth to the bone.
• Maintenance of the gingival tissues in their proper relationship to the teeth.
• Resistance to the impact of occlusal forces (shock absorption)
Light forces are absorbed by intravascular fluid that is forced out of the blood vessels
Moderate forces are also absorbed by extravascular tissue fluid that is forced out of the
periodontal ligament space into the adjacent marrow spaces
The heavier forces are taken up by the principal fibers
TRANSMISSION OF OCCLUSAL FORCES TO THE BONE : The arrangement of the principal fibres is similar to a suspension bridge or hammock . WHEN A HORIZONTAL OR TIPPLING FORCES IS APPLIED Two phases of tooth movement occur : 1 st with in the confines of the periodontal ligament 2 nd produces a displacement of facial and lingual bony plates In single rooted teeth the axis of rotation is located in the area between the apical third and the middle third of the root. In multirooted teeth, the axis of rotation is located in the bone between the roots
RESISTANCE TO THE IMPACT OF OCCLUSAL FORCES (Shock absorption): 3 Theories have been proposed to describe the mechanism of tooth support A. TENSIONAL THEORY The tensional theory of tooth support describes to the principal fibres of the periodontal ligament. The major responsibility in supporting the tooth and transmitting forces to the bone.
Force is applied to the crown Principal fibres unfold and straightened Transmit the forces to alveolar bone Elastic deformation of the bony socket Finally when the alveolar bone has reached its limit, the load is transmitted to the basal bone
B.VISCOELASTIC Theory It considers the displacement of the tooth to be largely controlled by fluid movements, with fibres having only a secondary role. When forces are transmitted to the tooth, the extra cellular fluid passes from the periodontal ligament into the marrow spaces of bone through foramina in the cribri form plate. After depletion tissue fluids, the fiber bundles absorb the slack and tighten. This leads to blood vessel stenosis. Arterial back pressure causes ballooning of the vessels, and passage of blood ultra filtrates into the tissues, there by replacing the tissue fluids.
Formative and Remodeling Function
Cells of the periodontal ligament participate in the formation and resorption of cementum and bone which occur:in physiologic tooth movement;
in the accommodation of the periodontium to occlusal forces;
and
in the repair of injuries.
The periodontal ligament is constantly undergoing
remodeling.
Old cells and fibers are broken down and replaced by new ones, and mitotic activity can be observed in the fibroblasts and endothelial cells.
Fibroblasts form the collagen fibers and may also develop into osteoblasts and cementoblasts.
Nutritional and Sensory Functions
Supplies nutrients to the cementum, bone, and gingiva by way of the blood vessels and provides lymphatic drainage.Supplied with sensory nerve fibers capable of transmitting tactile, pressure, and pain sensations by the trigeminal pathways.
Nerve bundles pass into the periodontal
ligament from the periapical area and through
channels from the alveolar bone that follow the
course of the blood vessels.
HOMEOSTATIC MECHANISM The resorption and synthesis are controlled procedures. If there is a long term damage of periodontal ligament, which is not repaired, the bone is deposited in the periodontal space. This results in obliteration of space and ankylosis between bone and the tooth. The quality of tissue changes if balance between synthesis and resorption is disturbed
If there is deprivation of Vit. C which are essential for collagen synthesis, resorption of collagen will continue. So there is progressive destruction and loss of extra cellular substance of ligament. This occurs more on bone side of ligament. Hence, loss of attachment between bone and tooth and at last, loss of tooth.
Thickness of Periodontal Ligament
• Age, location of the tooth, and degree of stress to which the tooth was subjected.• The mesial side is thinner than distal side.
• A tooth that is not in function has a thin periodontal ligament.
• A tooth in functional occlusion has a periodontal ligament
space of approximately 0.25 mm, plus or minus 0.10 mm.
• A tooth subjected to abnormal stress has a considerably
thicker periodontal space.
Cementum
Cementum is the calcified mesenchymal tissue that forms the outer covering of the anatomic root
Function; attach p.d.lig.f. to R.,contribute to process of repair
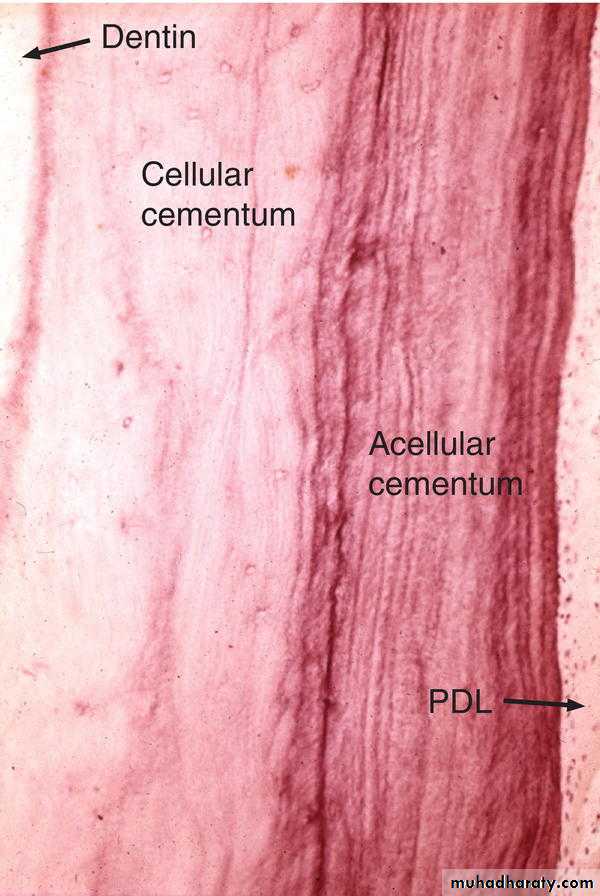
There are two main types of root cementum: acellular (primary) and cellular (secondary)
Both consist of a calcified interfibrillar matrix and collagen
Distribution of cementum on the tooth surface
ACEL, acellular cementum(primary) form with tooth formation ,coronallyCEL,cellular cementum (secondary)formed after tooth eruption in response to functional demand,laiddown on top of primary C.,apically
CVX,cervix
Acellular cementum (AC) showing incremental lines running parallel to the long axis of the tooth. These lines represent the appositional growth of cementum. Note the thin, light lines running into the cementum perpendicular to the surface; these represent Sharpey's fibers of the periodontal ligament (PL). D, Dentin.
Cellular cementum (CC) showing cementocytes lying within lacunae. Cellular cementum is thicker than acellular cementum. Evidence of incremental lines also exists, but they are less distinct than in acellular cementum. The cells adjacent to the surface of the cementum in the periodontal ligament (PL) space are cementoblasts. D, Dentin.
collagen fibers in cementum
There are two sources:Sharpey's (extrinsic) fibers and are formed by the fibroblasts
(intrinsic) and are produced by the cementoblasts