APLASTIC ANAEMIA
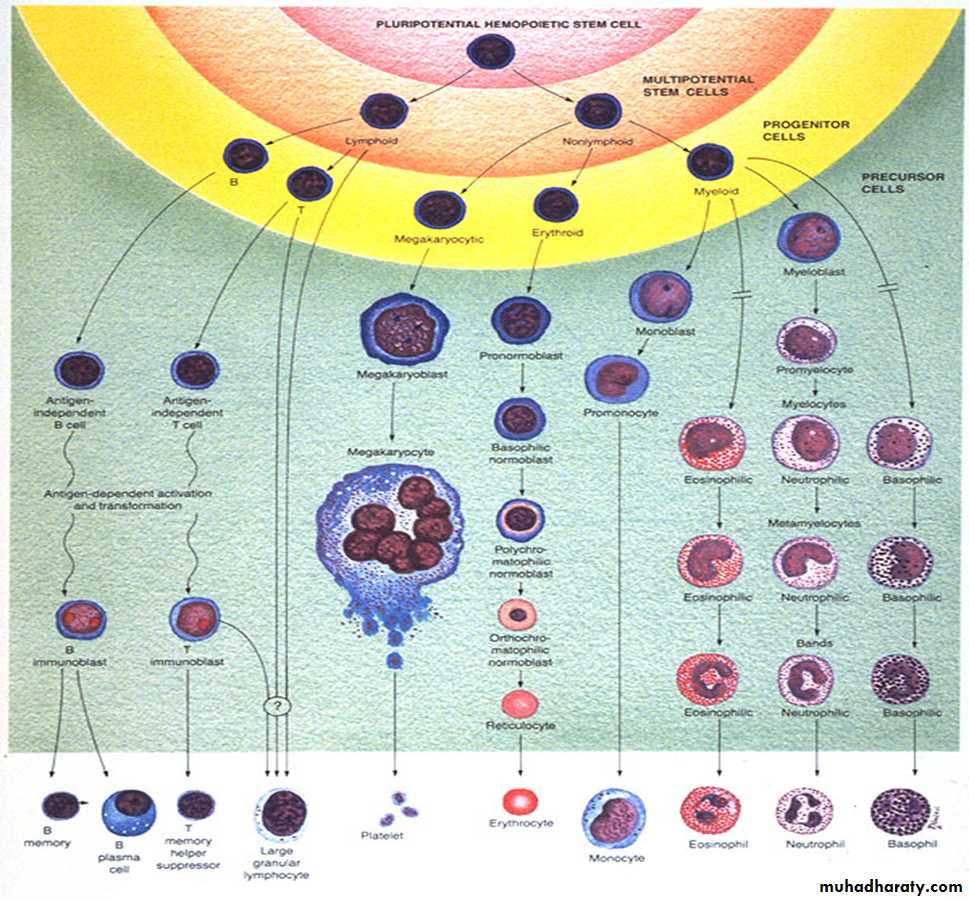
Primary idiopathic acquired aplastic anaemia:The basic problem is failure of the pluripotent stem cells, producing hypoplasia of the bone marrow with a pancytopenia in the blood.
The diagnosis rests on exclusion of other causes of secondary aplastic anaemia and rare congenital causes, such as Fanconi’s anaemia. IAPLASTIC
Clinical features and investigations
symptoms of bone marrow failure,1.Anaemia
2.Bleeding
3. Infection
Complete Blood Count(CBC) :
Pancytopenia.
Reticulocytopenia.
Bone marrow aspiration and biopsy reveal hypocellular marrow.
riaCamitta criteria
The severity of aplastic anaemia is graded according to the Camitta criteria
Severe AA (SAA)
• Marrow cellularity < 25% (or 25–50% with < 30% residual haematopoietic cells), plus at least two of:Neutrophils < 0.5 × 109/L
• Platelets < 20 ×109/L
• Reticulocyte count < 20 × 109/L
Very severe AA (VSAA)
• • As for SAA but neutrophils < 0.2 × 109/L
Non-severe AA (NSAA)
• AA not fulfilling the criteria for SAA or VSAA
Treatment
All patients will require blood product support and aggressive management of infection.The prognosis of severe aplastic anaemia managed with supportive therapy only is poor and more than 50% of patients die, usually in the first year
1.The curative treatment for patients under 35 years of age with severe idiopathic aplastic anaemia is allogeneic Hematopoietic Stem Cell Trasplantation (HSCT) if there is an available donor.
Older patients (35–50) may be candidates if they have no comorbidities.
Those with a compatible sibling donor should proceed to transplantation as soon as possible; they have a 75–90% chance of long-term cure2. In older patients, immunosuppressive therapy(IST) with ciclosporin and antithymocyte globulin. gives 5-year survival rates of 75%.
The thrombopoietin receptor agonist eltrombopag has produced trilineage responses in patients who fail IST and is licensed for this indication
Such patients may relapse or other clonal disorders of haematopoiesis may evolve, such as paroxysmal nocturnal haemoglobinuria, myelodysplastic syndrome and acute myeloid leukaemia
Causes of secondary aplastic anaemia
• DrugsCytotoxic drugs
Antibiotics – chloramphenicol, sulphonamides
Antirheumatic agents – penicillamine, gold,
phenylbutazone, indometacin
Antithyroid drugs
Anticonvulsants
Immunosuppressants – azathioprine
• Chemicals
Benzene toluene solvent misuse – glue-sniffing
Insecticides – chlorinated hydrocarbons (DDT),
organophosphates and carbamates
• Radiation
• Viral hepatitis
• Pregnancy
• Paroxysmal nocturnal haemoglobinuria
The clinical features and methods of diagnosis are the same as for primary idiopathic aplastic anaemia.
An underlying causeshould be treated or removed, but otherwise management is as for the idiopathic form.