SPONDYLOARTHROPATHIESpart 1
Dr. Ali Abdul-Rahman YounisRHEUMATOLOGIST(FIBMS)
SPONDYLOARTHROPATHIES
Spondyloarthropathies (SpAs) comprise a group of related inflammatory musculoskeletal diseases that show overlap in their clinical features and have a shared immunogenetic association with HLA-B27.In axial spondylitis and ankylosing spondylitis, the axial skeleton is predominantly affected.
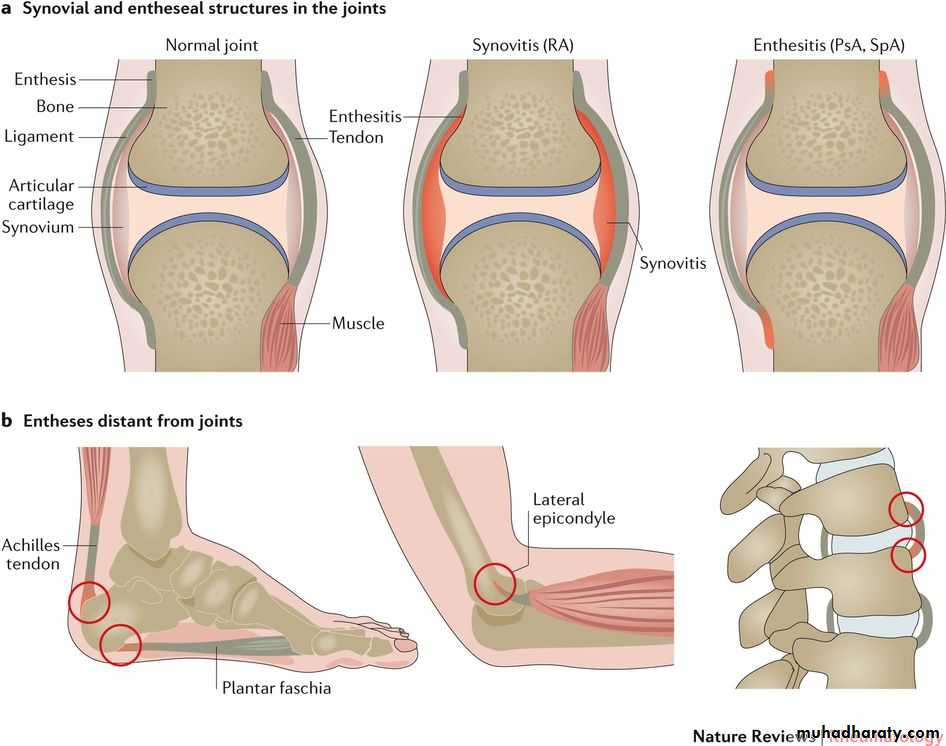
In contrast to RA, in the SpAs there are frequent and notable non-synovial musculoskeletal lesions – mainly inflammatory in nature – of ligaments, tendons, periosteum and other bone lesions.
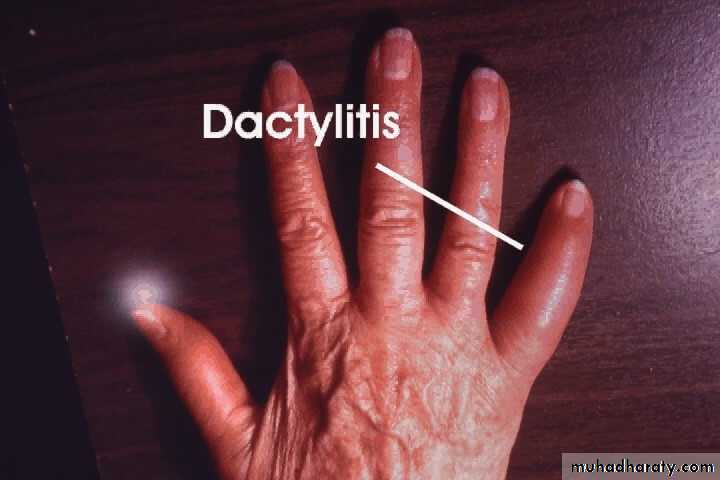
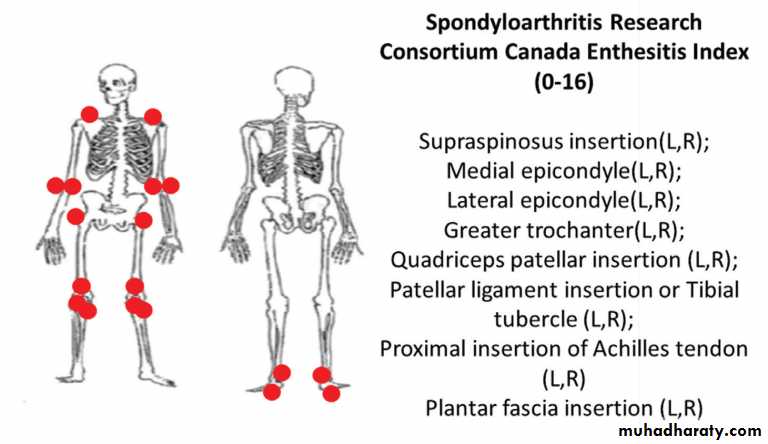
A hallmark lesion of all SpAs is enthesitis, which is inflammation at the site of a ligament or tendon insertion into bone. Dactylitis, inflammation of a whole finger or toe, may also occur
SPONDYLOARTHROPATHIES
It has been estimated that about 1% of the adult population in the USA may have an SpA (about 2.7 million).
There is a striking association with HLA-B27, particularly for ankylosing spondylitis (>95%).
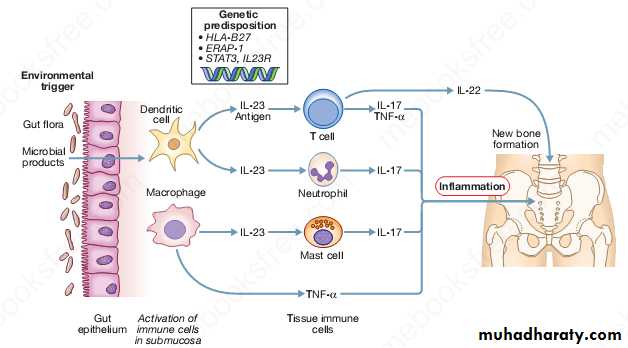
SpA are thought to arise as the result of an aberrant host response to infection and abnormal mucosal immunity mediated through changes in the IL-12,IL-23, and Th17 axis.
Familial clustering not only is common to the specific condition occurring in the proband, but also may extend to other diseases in the spondyloarthropathy group.
SPONDYLOARTHROPATHIES
They include:axial spondyloarthritis
ankylosing spondylitis
reactive arthritis
psoriatic arthritis
arthritis with inflammatory bowel disease (enteropathic spondyloarthritis)
Axial spondyloarthropathy
Axial spondyloarthropathy includes classical ankylosing spondylitis (AS) as well as axial spondyloarthritis (axSpA).Inflammatory changes in the entire axial skeleton are characteristic of axSpA and can be visualized by MRI; structural alterations, such as new bone formation with syndesmophytes and ankylosis, develop later in the course of the disease.
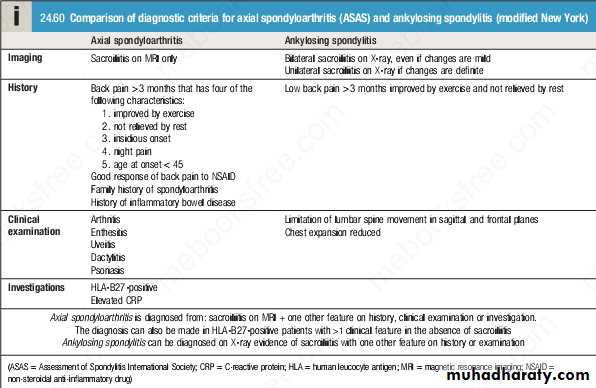
The criteria for diagnosing AS , which require evidence of sacroiliitis on X-ray, are often only able to be applied many years after a patient’s symptoms started.
Not all patients with axSpA will go on to develop AS.
Pathophysiology
Axial SpA and AS arise from an interaction between environmental pathogens and the host immune system in genetically susceptible individuals.There is increasing evidence that axSpA and AS are due to an abnormal host response to the intestinal microbiota with involvement of Th17 cells, which have a key role in mucosal immunity.
This leads to production of various inflammatory cytokines, including IL-12, IL-23, IL-17 and TNF-α, which play vital roles in the pathogenesis of enthesitis and other inflammatory lesions.
There is a strong association between axial spondyloarthropathy and carriage of the major histocompatibility complex (MHC) class I molecule HLA-B27. This is particularly striking in patients defined as having AS, more than 95% of whom are positive for HLA-B27.
Axial spondyloarthritis
Clinical featuresThe cardinal feature of axSpA is inflammatory back pain and early morning stiffness, with low back pain radiating to the buttocks or posterior thighs if the sacroiliac joints are involved.
Symptoms are exacerbated by inactivity and relieved by movement.
Musculoskeletal symptoms may be prominent at entheses, may be episodic and, if persistent, can present as widespread pain and be mistaken for fibromyalgia.
Fatigue is common.
A history of psoriasis (current, previous or in a first-degree relative) and inflammatory bowel symptoms (current or previous) are important clues.
Clinical features
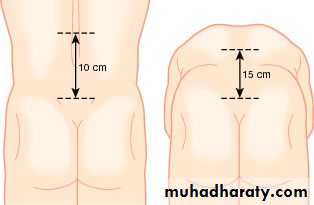
Physical signs include a reduced range of lumbar spine movements in all directions, pain on sacroiliac stressing and a high enthesitis index.
Entheses that are typically affected include Achilles’ insertion, plantar fascia origin, patellar ligament entheses, gluteus medius insertion at the greater trochanter and tendon attachments at humeral epicondyles.
Investigations
The diagnosis is aided by ultrasound or MRI of entheses, or by MRI of the sacroiliac joints and spine.Other findings may include raised ESR and CRP (although these can be normal), anemia and positive HLA-B27.
Faecal calprotectin is a useful screening test for associated inflammatory bowel disease.
Magnetic resonance imaging appearances in sacroiliitis.
Coronal MRI short T1 inversion recovery (STIR) sequence showing bilateral sacroiliitis in axial spondyloarthritis.Management
Patient education, NSAID use (optimally, once daily or slow release taken at bedtime) and physical therapy are key interventions at the outset.For severe and/or persistent peripheral musculoskeletal features of SpA, both sulfasalazine and methotrexate are reasonable therapy choices. These medications have no impact on spinal symptoms or disease progression.
In patients who fail to respond adequately or who cannot tolerate NSAIDs, progression to biologic therapy with either TNF inhibitors or the IL-17 inhibitor secukinumab should be considered .
Anti-TNF therapy is effective for both the axial and peripheral lesions of axSpA, but it is as yet unclear whether anti-TNF therapy modifies the natural history of the disease.
Prognosis
axSpA can remain mild and/or episodic in many patients for many years.
HLA-B27 positivity, high persistent CRP and high functional incapacity are likely to be markers of poor prognosis, if not markers of extension ultimately to AS.Ankylosing spondylitis
Ankylosing spondylitis (AS) is defined by the presence of sacroiliitis on X-ray and other structural changes on spine X-rays, which may eventually progress to bony fusion of the spine.There is a male-to-female ratio of about 3 : 1.
In Europe, more than 90% of those affected are HLA-B27-positive.
The overall prevalence of AS is below 0.5% in most populations.
Over 75% of patients are able to remain in employment and enjoy a good quality of life.
Even if severe ankylosis develops, functional limitation may not be marked, as long as the spine is fused in an erect posture.
Clinical features
Clinical features are the same as in axSpA.AS typically evolves slowly, with fluctuating symptoms of spinal inflammation.
Ankylosis develops in many patients over a period of many years.
Secondary osteoporosis of the vertebral bodies frequently occurs, leading to an increased risk of vertebral fracture.
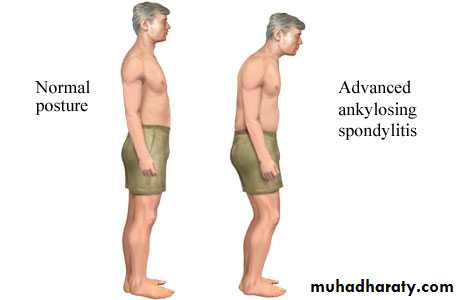
In AS, spinal fusion varies in its extent and in most cases does not cause a gross flexion deformity, but a few patients develop marked kyphosis of the dorsal and cervical spine that may interfere with forward vision. This may prove incapacitating, especially when associated with fixed flexion contractures of hips or knees.
Up to 40% of patients also have peripheral musculoskeletal lesions (asymmetrical, affecting entheses of large joints, such as the hips, knees, ankles and shoulders).
Clinical features
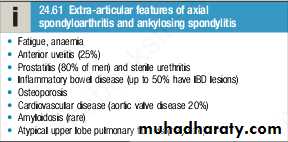
Fatigue is a major complaint and is common to all SpAs, but its cause is unknown.Acute anterior uveitis is a common extra-articular feature, which occasionally precedes joint disease.
Other extra-articular features are occasionally observed but are rare.
Investigations
X-rays of the sacroiliac joint show irregularity and loss of cortical margins, widening of the joint space and subsequently sclerosis, joint space narrowing and fusion.Lateral thoracolumbar spine X-rays may show anterior ‘squaring’ of vertebrae due to erosion and sclerosis of the anterior corners and periostitis of the waist.
Bridging syndesmophytes may also be seen, which are areas of calcification that follow the outermost fibres of the annulus.
In advanced disease, ossification of the anterior longitudinal ligament and facet joint fusion may also be visible. The combination of these features may result in the typical ‘bamboo’ spine.
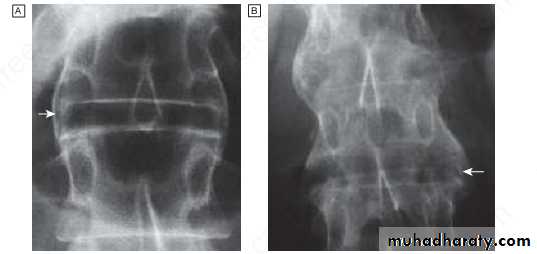
Radiographic changes in spondyloarthritis. A Fine symmetrical marginal syndesmophytes typical of ankylosing spondylitis (arrow).
B Coarse, asymmetrical non-marginal syndesmophytes typical of psoriatic spondylitis (arrow).
‘Bamboo’ spine of advanced ankylosing spondylitis. Note the symmetrical marginal syndesmophytes (arrows), sacroiliac joint fusion and generalised osteopenia
Investigations
Erosive changes may be seen in the symphysis pubis, ischial tuberosities and peripheral joints.
Osteoporosis is common and vertebral fractures may occur.
Atlanto-axial dislocation can arise as a late feature.
DXA scanning is important as part of a fragility fracture assessment.
ESR and CRP are usually raised in active disease but may be normal; anemia is often present. Autoantibodies, such as RF, ACPA and ANA, are negative.
Management
The aims of management are : to relieve pain and stiffness, maintain a maximal range of skeletal mobility and avoid the development of deformities.Mobilizing exercises are important.
A long-acting NSAID at night is helpful for alleviation of morning stiffness.
Anti-TNF or anti-IL-17A therapy should be considered in patients who are inadequately controlled on standard therapy .
Biologic therapies are often highly effective at improving symptoms but it is not clear whether they prevent ankylosis or alter the natural history of the disease.
Management
Local glucocorticoid injections can be useful for persistent plantar fasciitis, other enthesopathies and peripheral arthritis.Oral glucocorticoids may be required for acute uveitis but do not help spinal disease.
Severe hip, knee or shoulder arthritis with secondary OA may require arthroplasty.
Spinal osteotomy, to correct stoop and make eyeline/posture ‘more normal’, can make a significant difference to patients with severe ankylosed kyphotic spines.
THANKS FOR LISTENING