1
Arterial system: Long and short
ciliary arteries
Venous system: vortex veins
) ﻋﺪد اﻻوراق
11
(
ﻋﯿﻮن
23
/
1
1
/
2019
.د
ﻋﺰام
Lec: 7
Uveal Tract
Out-lines:
1 Anatomy and physiology of uveal tract.
2 Uveitis nomenclatures.
3 Approach to patient with uveitis.
4 treatment and complications.
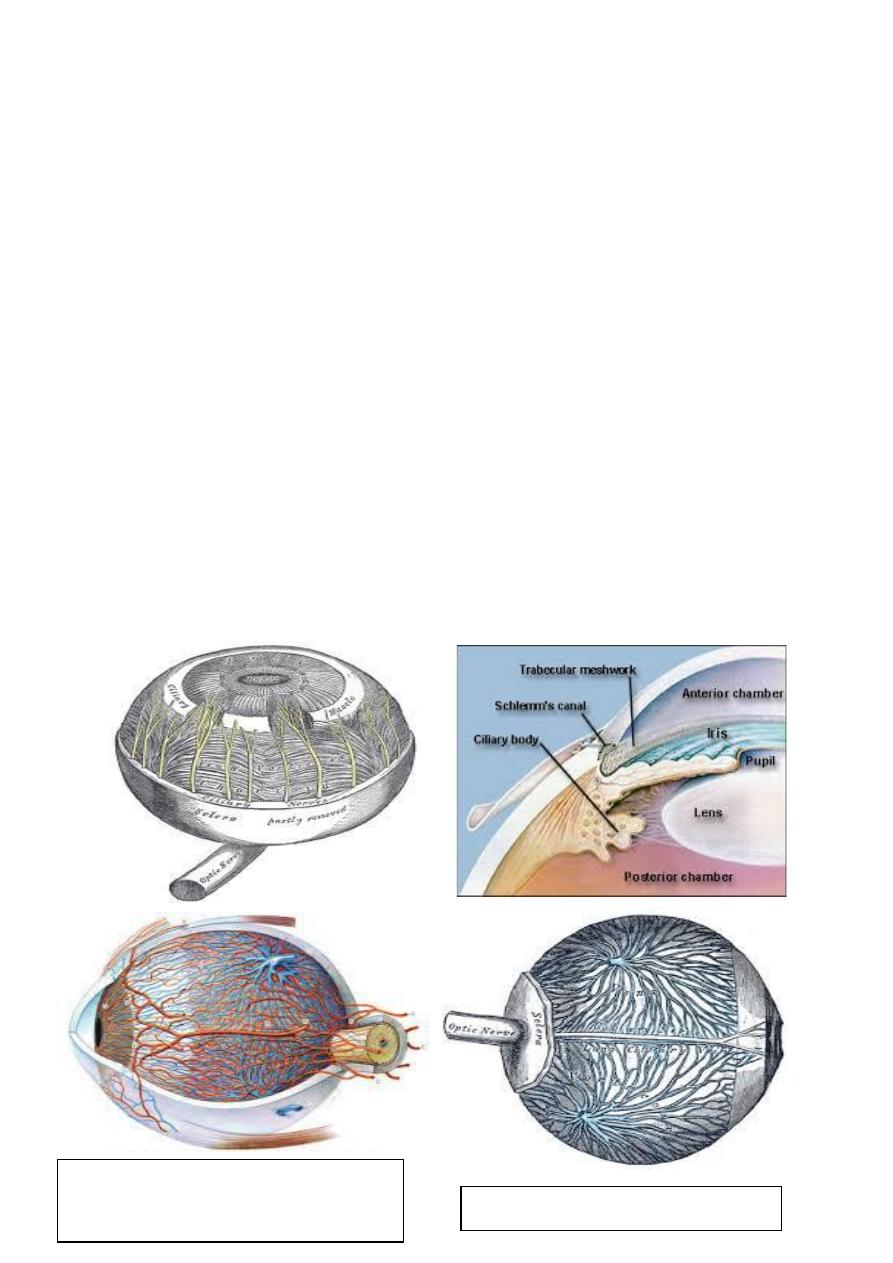
Anatomy and physiology:
Uveal tract /
Anatomy
1 Iris.
2 Ciliary body.
3 Choroid.
2
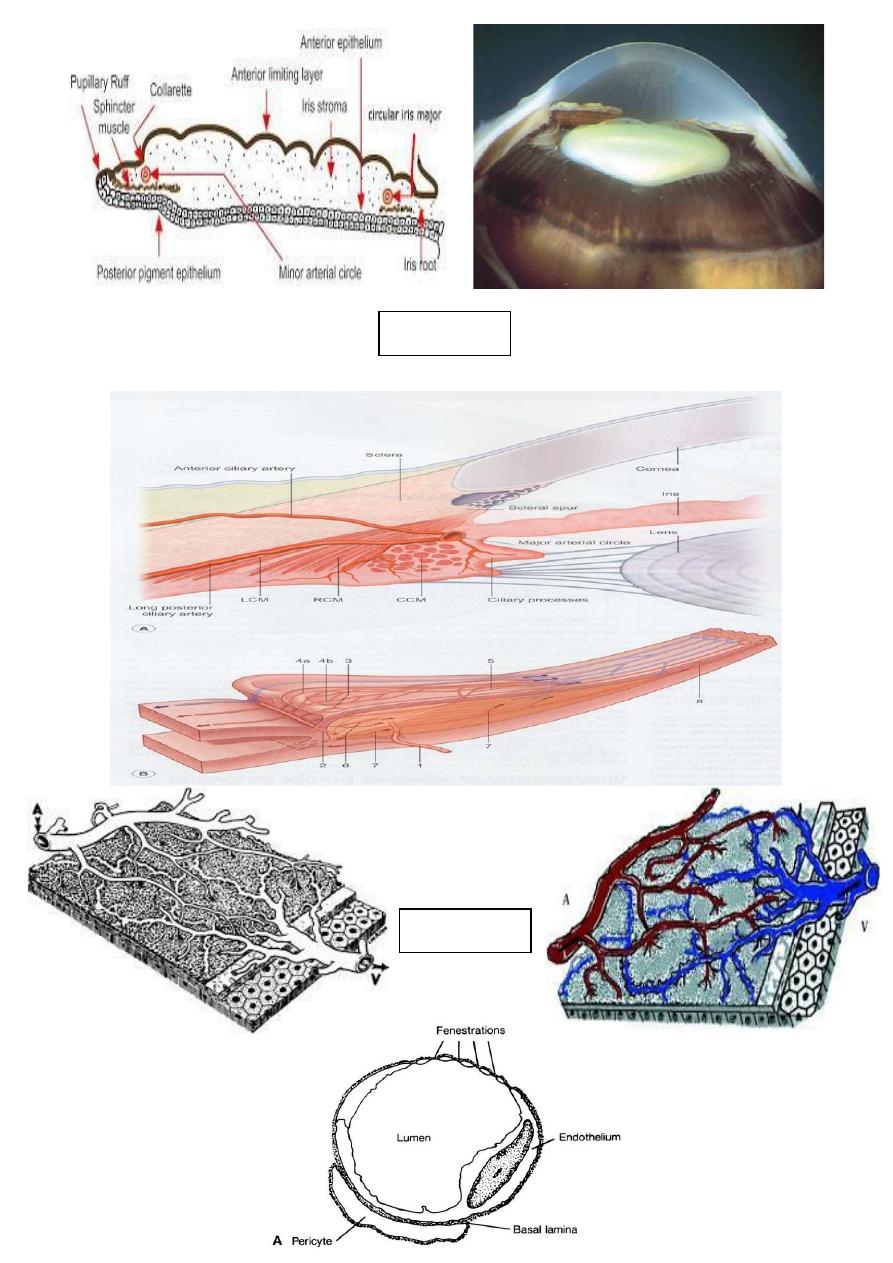
Iris
Choroid
Blood supply of uveal tissue:
3
Uveitis:
• The uvea is the intermediate vascular layer of the eye which
comprise the iris, ciliary body and choroid.
• Uveitis: inflammation of uveal tract.
• The term uveitis refers to a group of inflammatory disorders
affecting the uvea, the middle layer of the eye. Endogenous or
associated with a systemic disease, noninfectious uveitis
accounts for approximately 75% of total cases comprising of a
heterogeneous group of inflammatory conditions. The incidence
of uveitis in the general population is between 17 and 52 cases
per 100,000 habitant per year with prevalence of 0.1%. People
aged 20-50 years are commonly affected. Uveitis are
responsible for about 10% of legal blindness in developed
nations, and are more than 35% of patients with uveitis
represent significant visual loss in at least one eye. These data
reveal the magnitude of the epidemiologic, diagnostic, and
therapeutic problem posed by the uveitis, as well as healthcare
cost generated. So, both for diagnosis and, especially, for the
proper treatment, close cooperation between ophthalmologist,
rheumatologist and general practitioners are required in order to
correctly classify the pattern of uveitis and associated co-
morbidities to establish the most appropriate therapeutic
scheme.
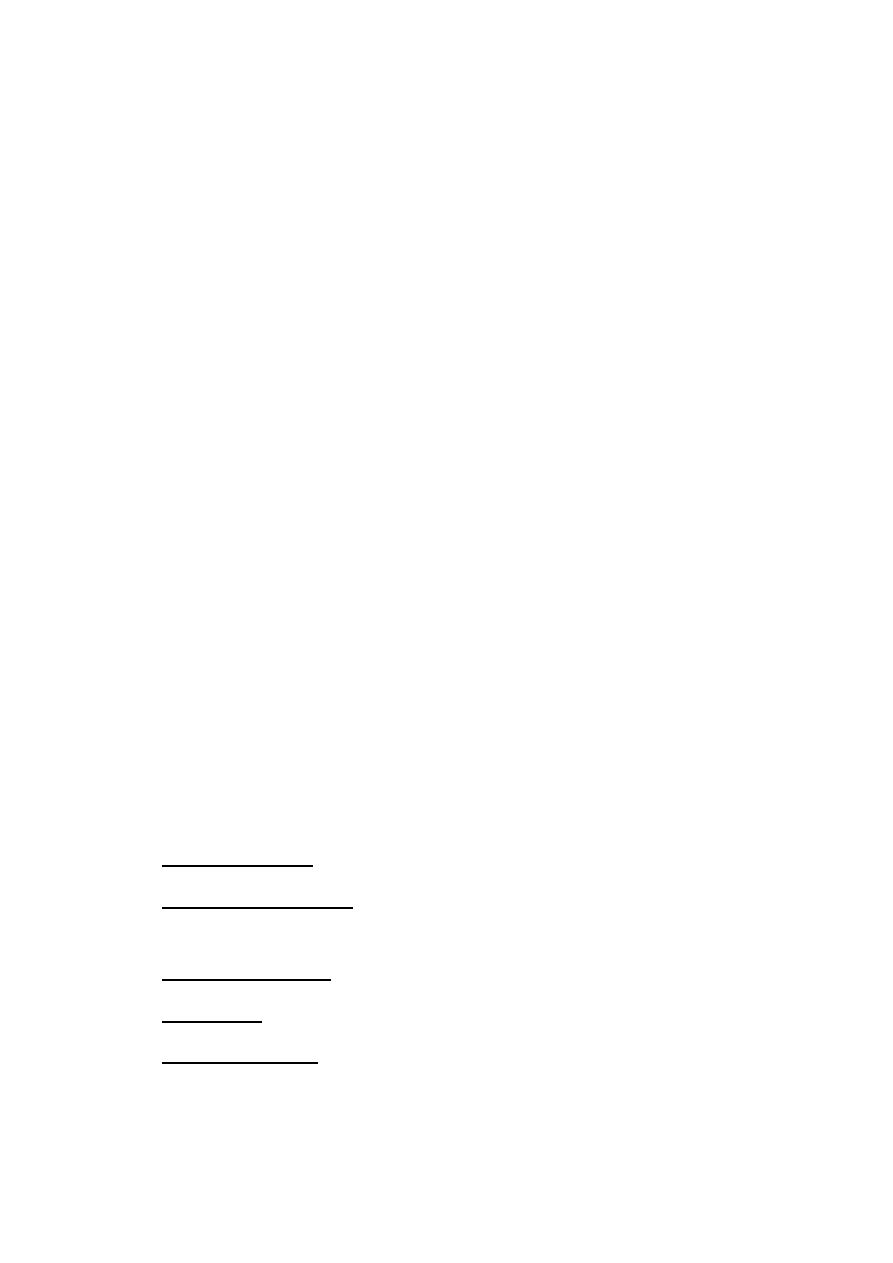
• Anterior uveitis: subdivided into iritis and iridocyclitis.
• Intermediate uveitis: inflammation predominantly involving the
vitreous.
• Posterior uveitis: involve funds posterior to the vitreous base.
• Panuveitis: entire uveal tract inflammation.
• Panophthalmitis: involve entire globe with orbital extention.
• Uveitis may be acute,incidoius, limited or persistant. The coarse
may be acute, recurrent or chronic if it is more than 3 months.
4
Approach to patient with uveitis:
1 History.
2 Investigations.
3 Treatment.
History:
• Age of presentation is very important, e.g. uveitis associated
with juvenile idiopathic arthritis (JIA) is typically affects
children.
• HLA B27 associated uveitis and Behcet syndrome usually
affect young adults.
• Sepiginous choroditis affect 5
th
-7
th
decade of life.
• Past ocular history e.g. previous ocular trauma would point to
sympathetic ophthalmia.
• Past medical history: exposure to infectious agent e.g.
Tuberculosis and syphilis.
• History of raring pits: in toxoplasmosis.
• Toxoplasmosis may affect any age group.
• Hygiene and dietary habits: e.g. toxoplasmosis (uncooked meat).
5
Investigations:
• Generally not necessary in single attack if:
Mild unilateral acute anterior uveitis without suggestion of
possible underlying cause.
Specific Uveitis entities e.g. sympathetic ophthalmia.
When systemic diagnosis compatible with Uveitis
Indications for investigation:
1. Recurrent granulomatous anterior uveitis.
2. Bilateral case.
3. Systemic manifestations without specific diagnosis.
4. Confirmation of suspected ocular picture.
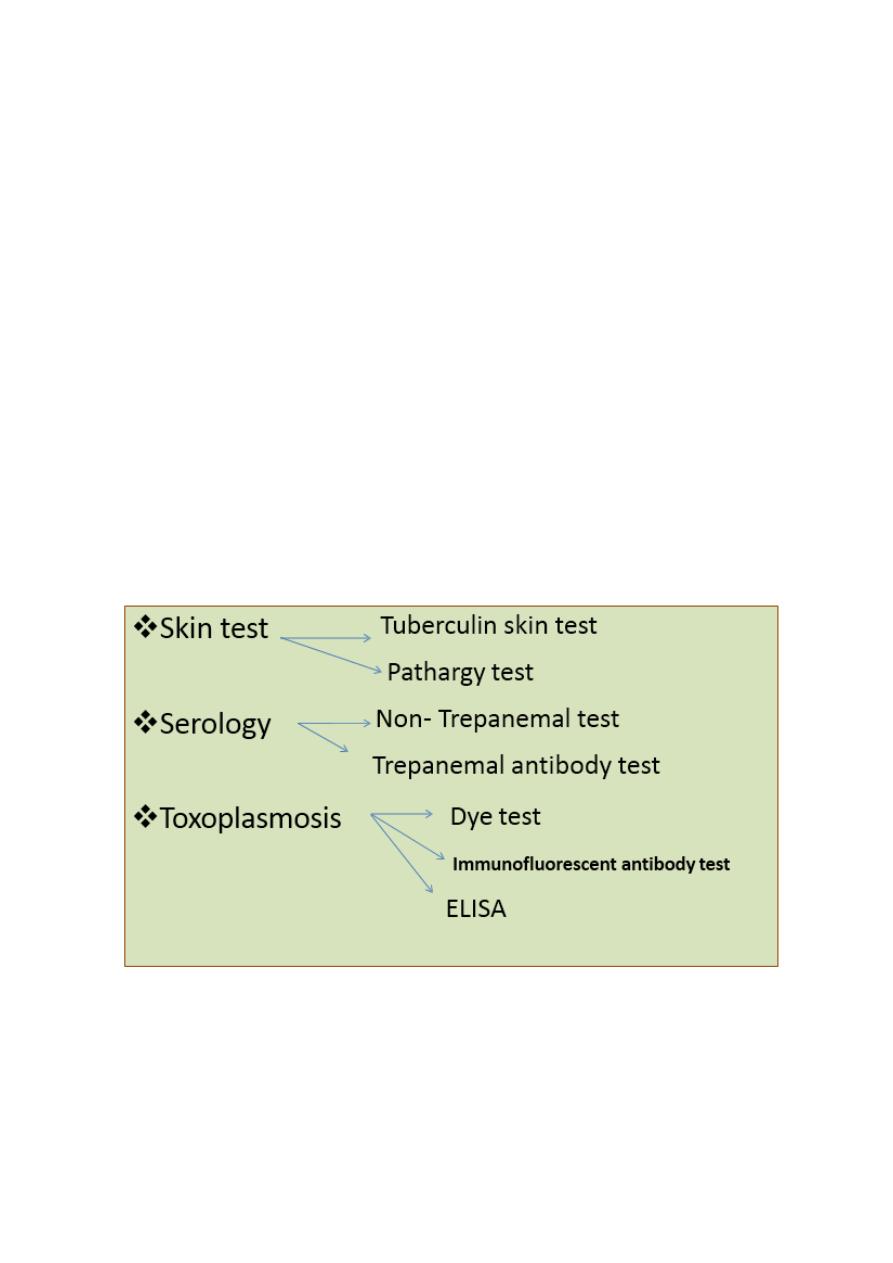
Investigations:
6
Pathargy test
Tuberculin skin test
Dye test
Immunofluorescent
antibody test
ELISA
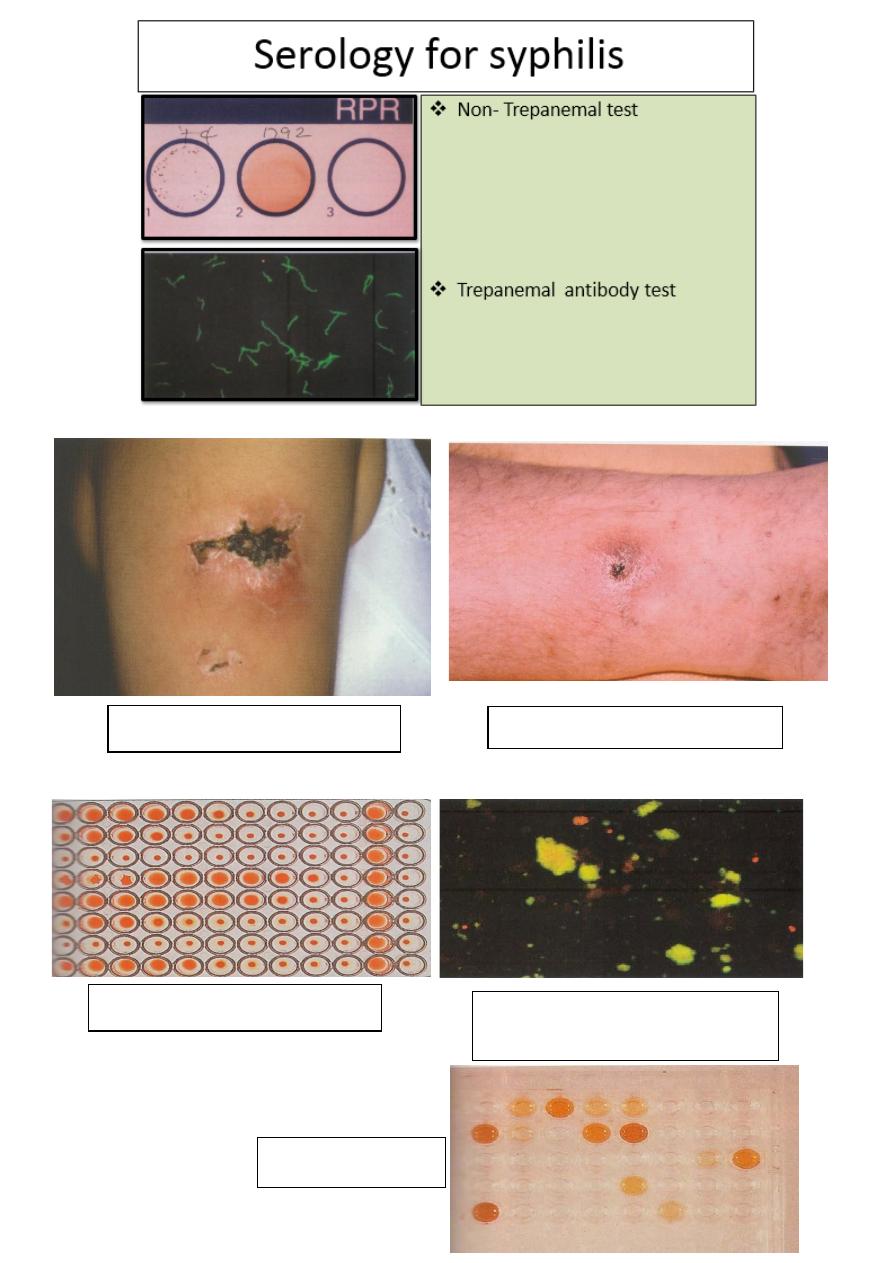
Investigations:
Skin tests
Serology:
for toxoplasmosis

7
HLA tissue typing
Imaging:
o
Flurescein Angiography
o
Indocyanin Green
o
Ultrasonography
Biopsy:
o
conjunctival and lacrimal gland for Sarcoidosis.
o
Aqueous sample with PCR for viral retinitis.
o
Vitreous biopsy for endophthalmitis & intraocular
Lymphoma
Retinal and choroidal biopsy
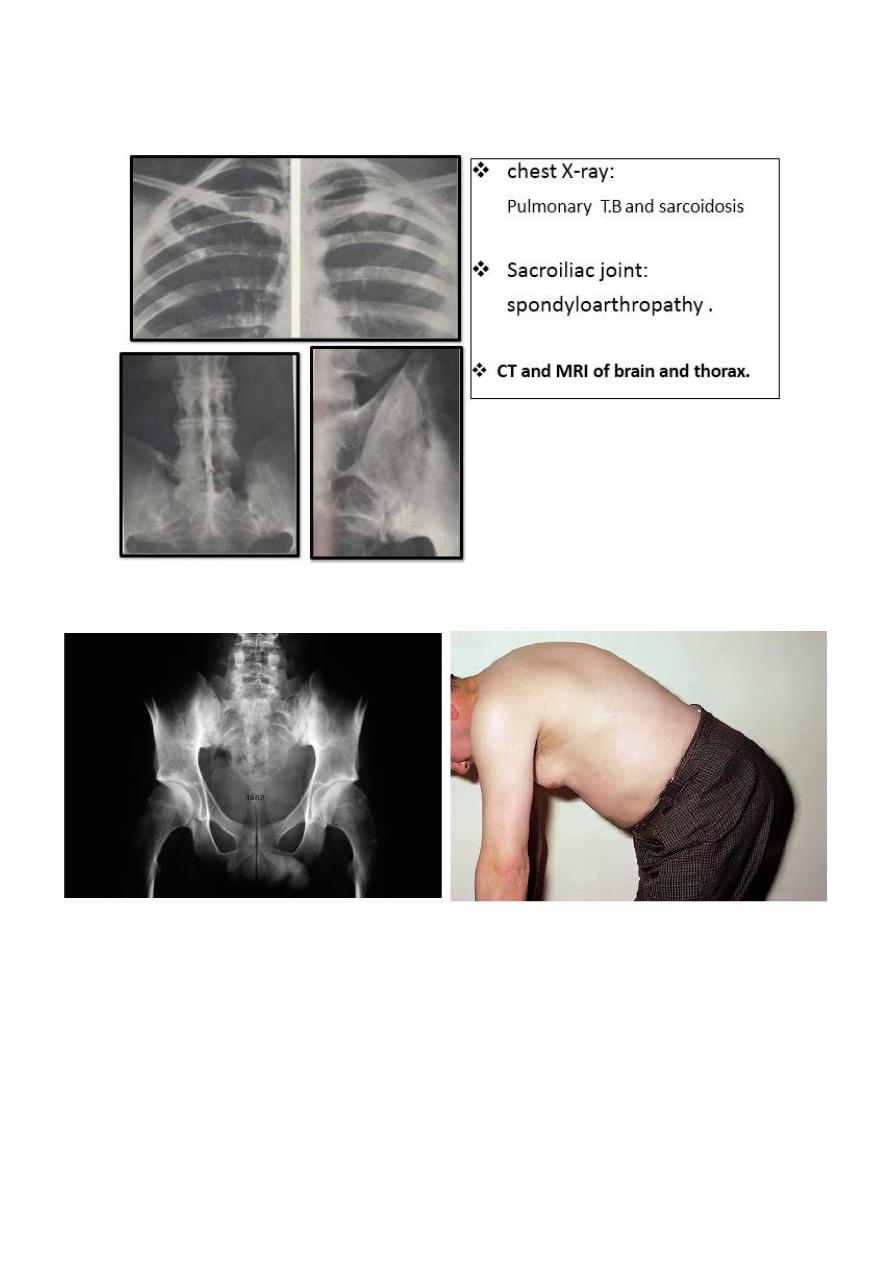
Radiology: chest X-ray, T.B and sarcoidosis
Sacroiliac joint, spondyloarthropathy CT and MRI of brain
and thorax.
Antinuclear antibody (ANA)for JIA.
8
Radiology:
Limitation of lumbo-sacral spine movement:
Acute Anterior uveitis:
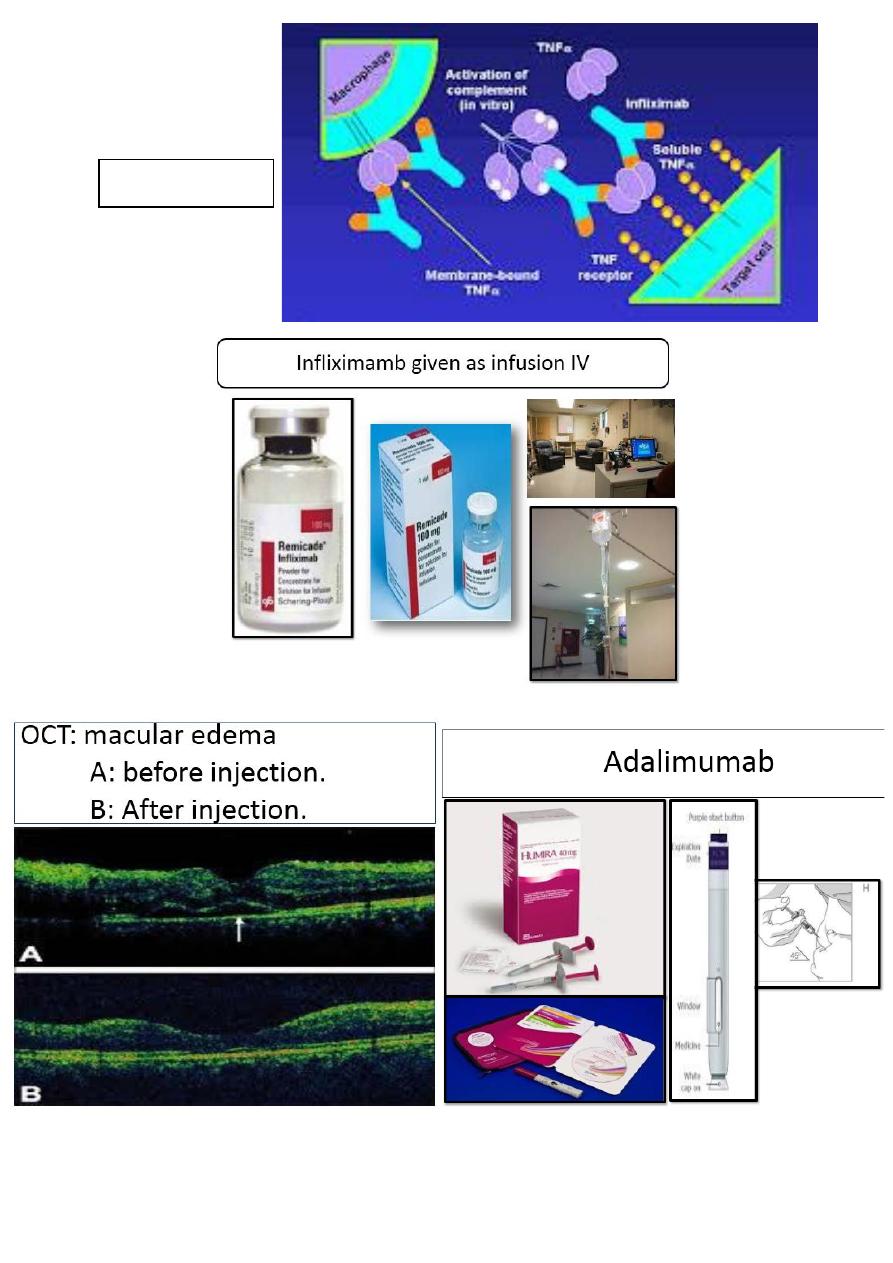
• Anterior uveitis is the most common form of uveitis. Acute
anterior uveitis (AAU) is the most common form of anterior
uveitis, accounting for three-quarters of cases.
• It’s easily recognized due to severity of symptoms, which force
the patient to seek medical attention.
9
Clinical features:
Symptoms:
• Presentation is typically with sudden onset of unilateral pain,
photophobia and redness, which may be associated with
lacrimation.
• Acute anterior uveitis (AAU) is the most frequent form and
usually requires only topical treatment with steroids and
mydriatic. However, it is a cause of disability when flares are
frequent or when tends to become chronic.
• Sulphasalazine and methotrexate have demonstrated a reduction
in the number of flares and better control of inflammatory
activity in cases of chronicity.
• Other patterns of uveitis with involvement of intermediate and
posterior segments have a worse prognosis
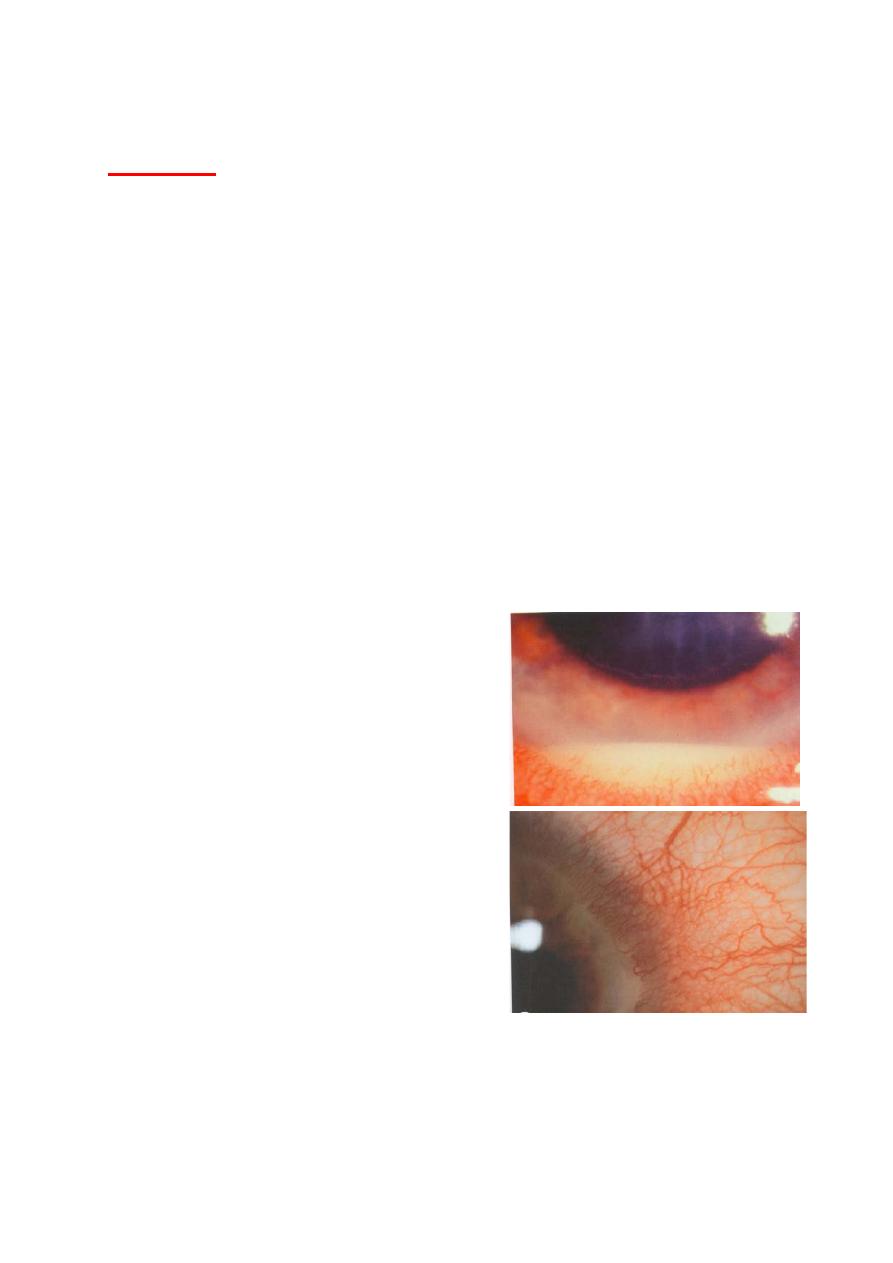
Signs of uveitis:
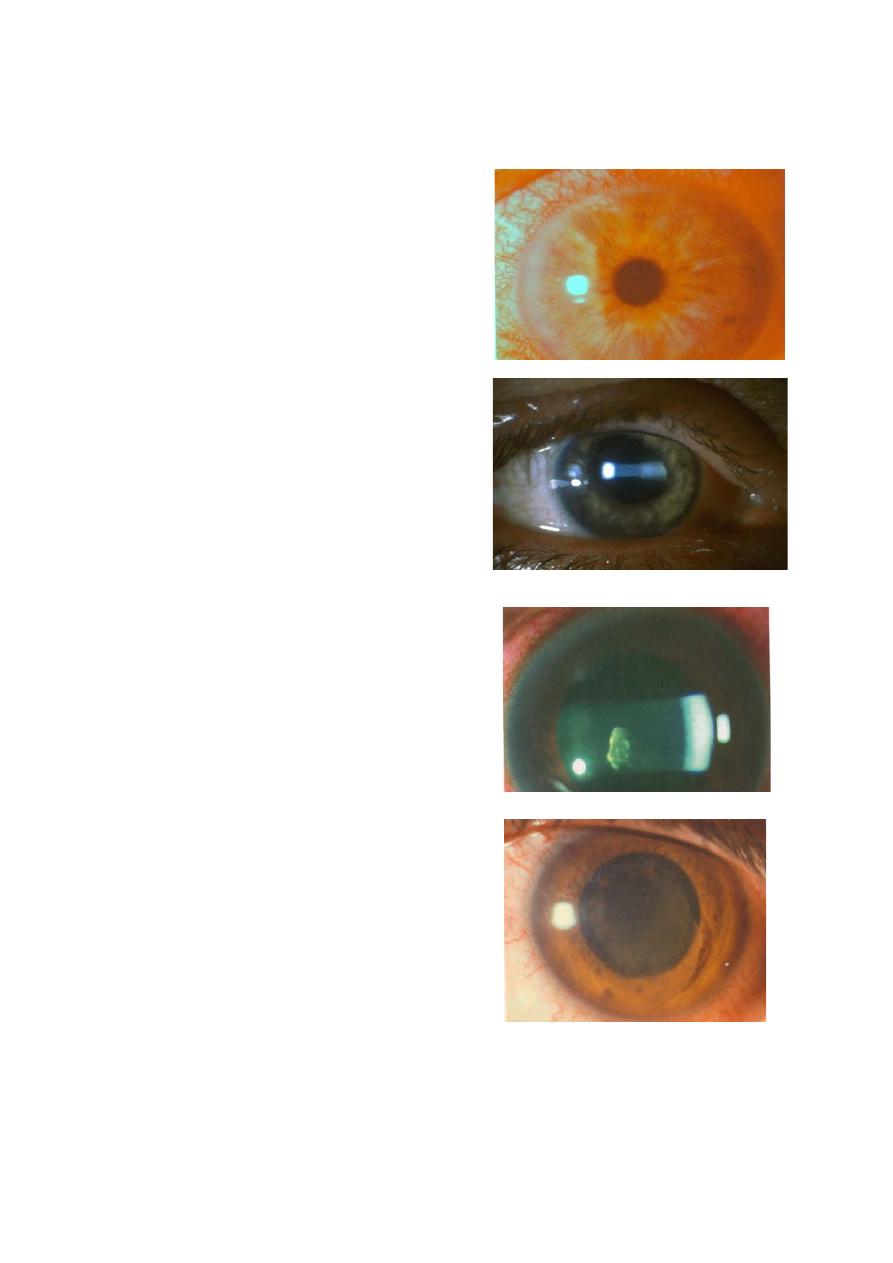
• Visual acuity: is usually good at
presentation, except in very severe
cases with hypopyon.
• Ciliary (circumcorneal) injection
has a violaceous hue.
Infectious causes and masquerade
syndromes should always be
excluded before considering an
immune-mediated mechanism, since
therapeutic scheme is completely
different. Some infectious causes,
such as toxoplasmosis, herpes,
syphilis and tuberculosis could produce uveitis and, frequently,
clinical signs indistinguishable from those produced by immune-
mediated uveitis. Some malignancies, especially CNS lymphoma,
10
can also simulate uveitis, postoperative and drug-induced uveitis
must be discarded.
• Miosis due to sphincter spasm
may predispose to formation of
posterior synechiae unless the
pupil is dilated.
• Aqueous cells indicates disease
activity and their number
reflects disease severity.
• Anterior vitreous cells indicate
iridocyclitis.
• Aqueous flare reflects the
presence of protein due to break
down of blood aqueous barrier.
11
Posterior synechiae
Keratic precipitate
• Endothelial dusting may be
myriads of cells is present
early and gives rise to a
“dirty” appearance and true
keratic precipitates usually
appears only after a few days
and are usually non-
granulomatous.
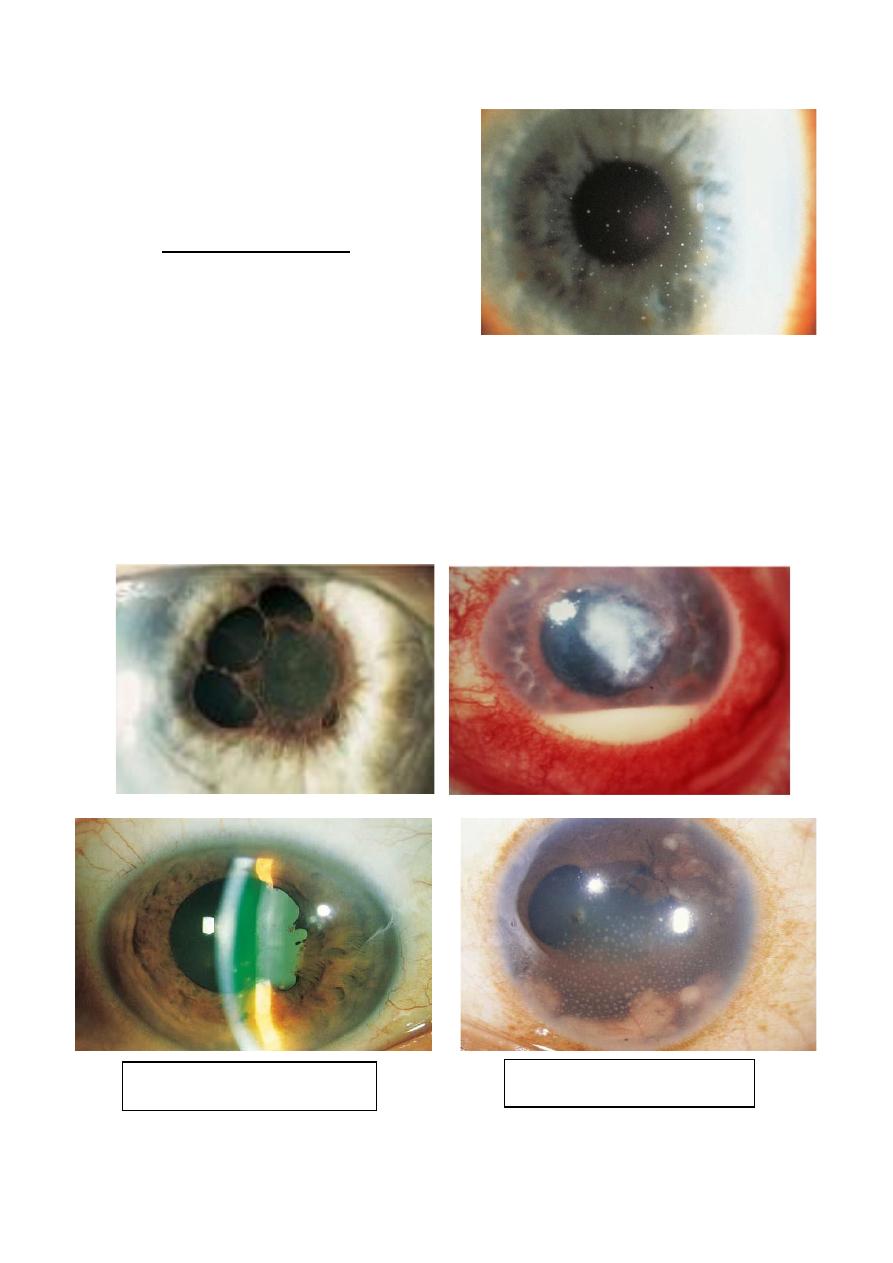
• Hypopyon is a feature of intense inflammation in which the
cells settle in the inferior part of anterior chamber and form a
horizontal level.
• Dilated iris vessels .
• Posterior synechiae may develop quite quickly and must be
broken down before they become permanent.
12
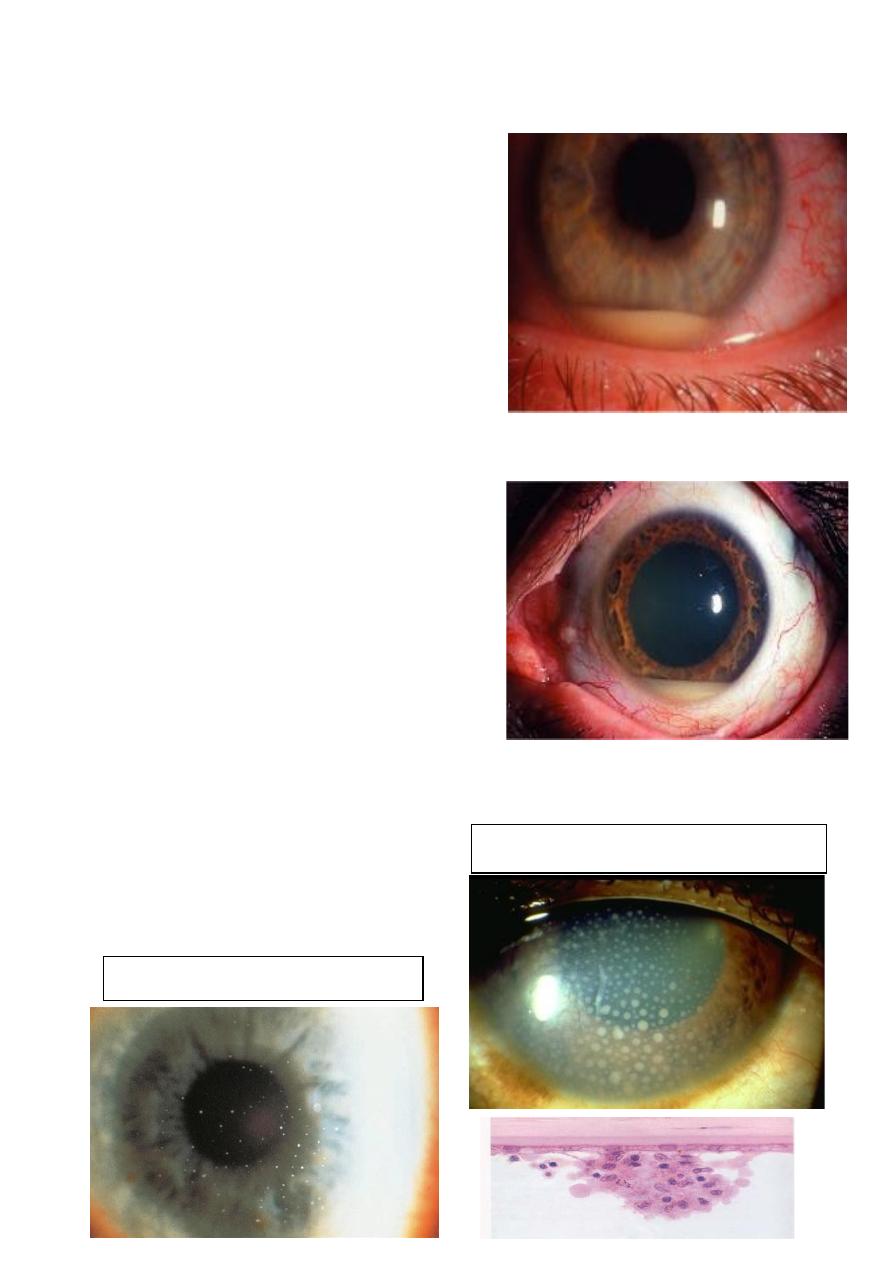
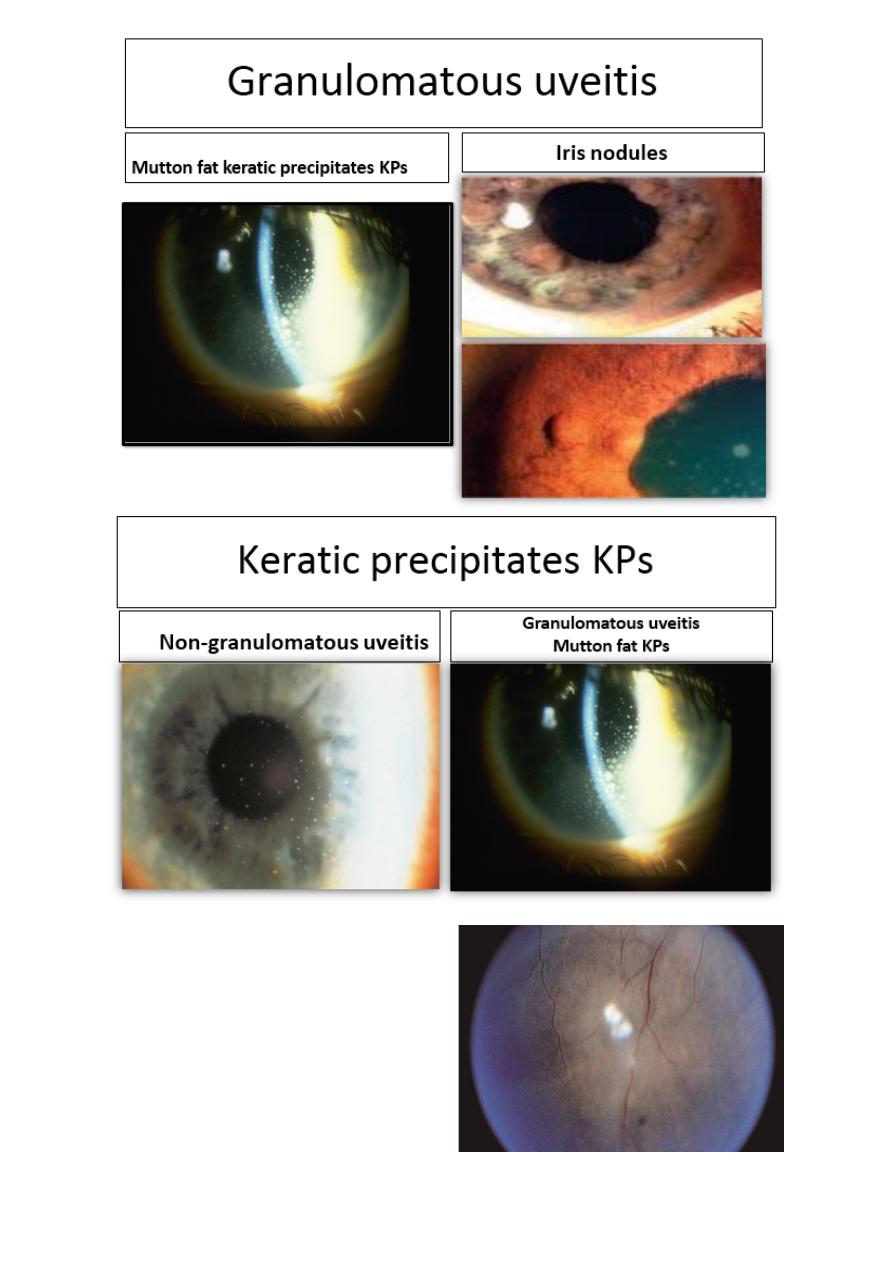
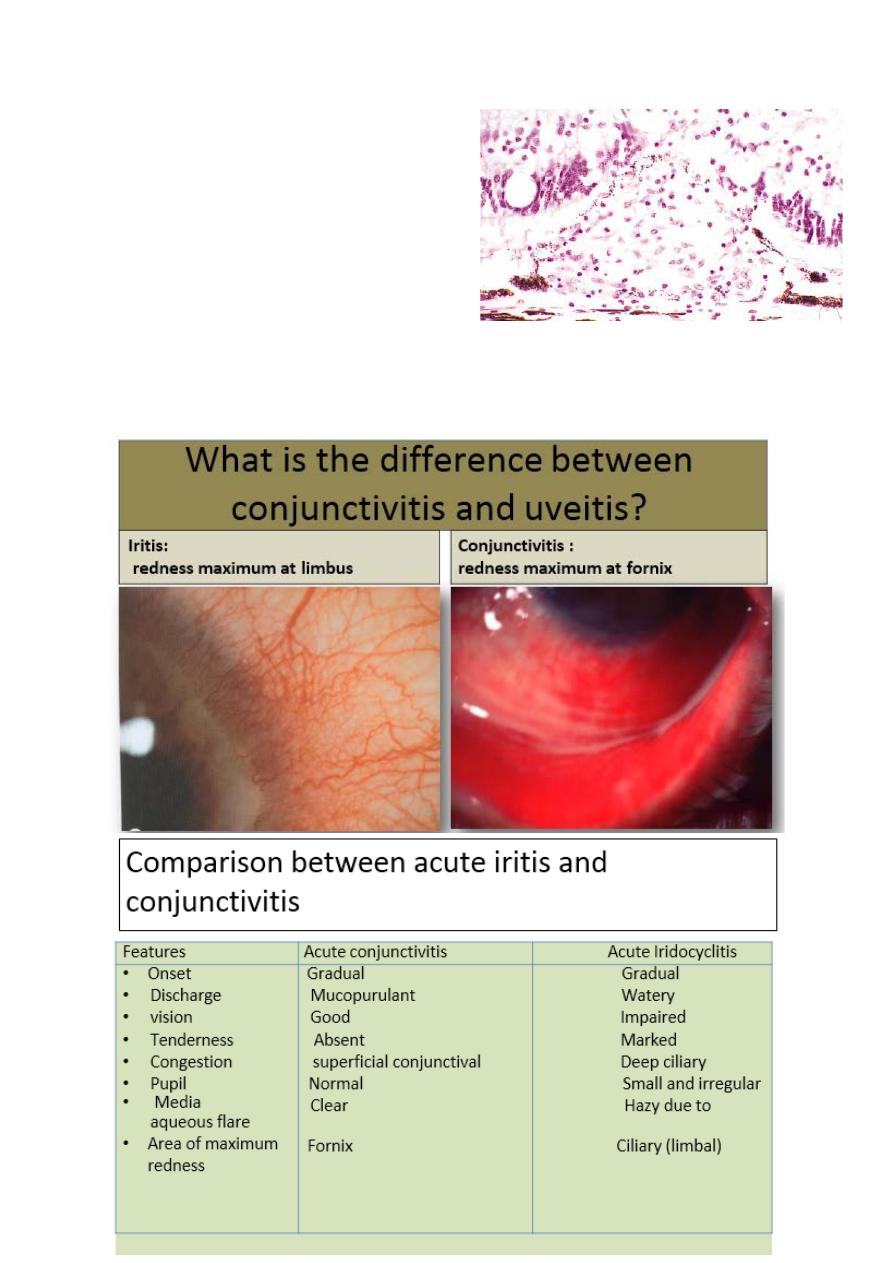
Non-granulomatous uveitis
Granulomatous uveitis Mutton fat KPs
• Low IOP is the rule as a result of
reduced secretion of aqueous by
ciliary epithelium.
Occasionally ,the IOP may be
elevated (hypertensive uveitis) in
herpetic uveitis and toxoplasma
retinitis.
• In AAU associated with HLA-
B27,the hypopyon has a high
fibrin content which makes it
dense, immobile and slow to adsorb.
• In patients with BehÇet
syndrome, the hypopyon has
minimal fibrin content and there
fore shifts according to patient
head position and may disappear
quickly.
• Hypopyon associated with blood
occurs in herpetic infection and in
eyes with associated rubeosis
iridis.
Keratic precipitates KPs:
13
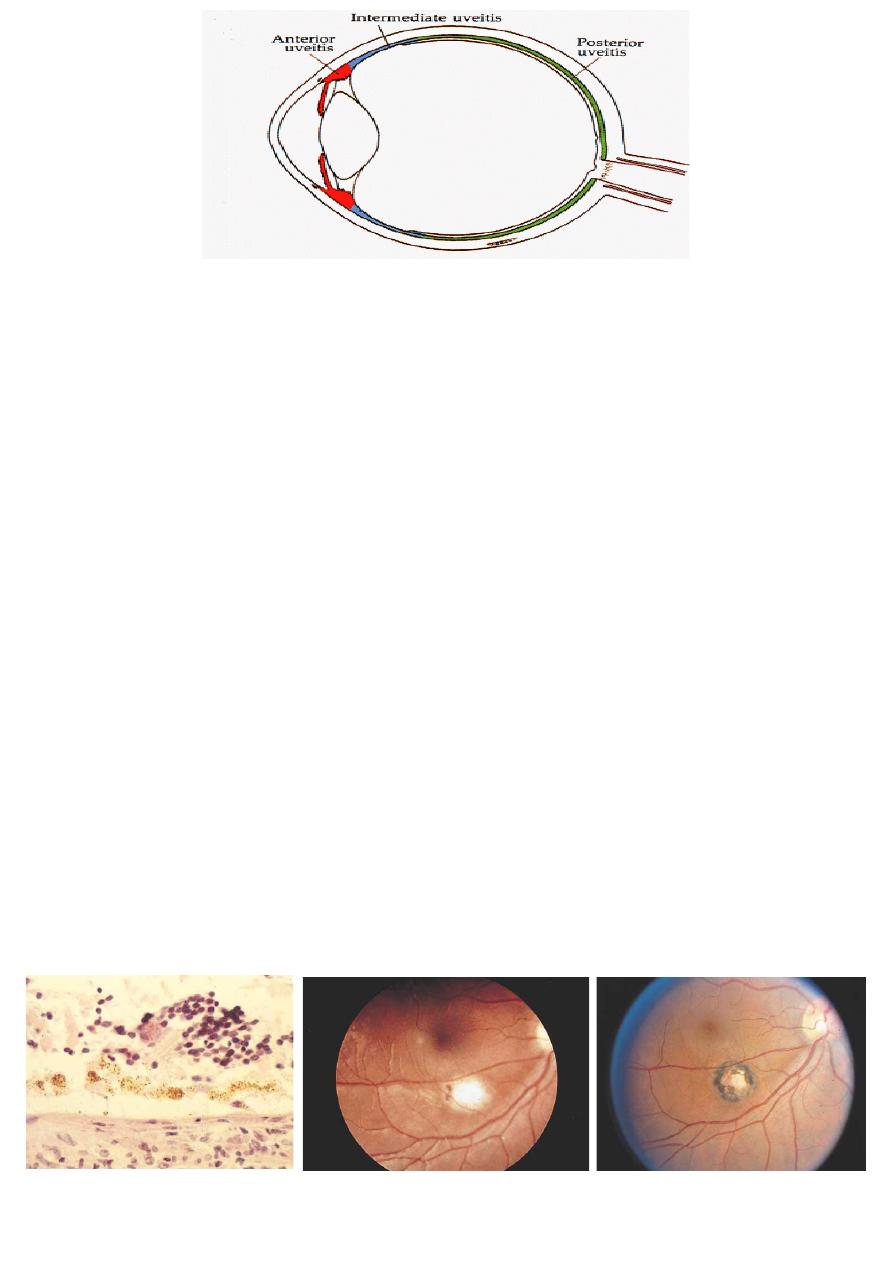
epithelioid cells in the inflammatory nodules
Granulomatous inflammation:
• Definition:
Chronic granulomatous inflammation
is a proliferative inflammation
characterized by a cellular infiltrate of
epithelioid cells (and sometimes
inflammatory giant cells,
lymphocytes, plasma cells,
polymorphonuclear leukocytes
(PMNs), and eosinophils.
Granulomatous uveitis:
Causes:
1 Chronic sarcoidosis.
2 Sympathetic ophthalmia.
3 Voket-Koyanaki Harada
syndrome.
4 Infection: T.B, syphilis,
toxoplasmosis.
5 phacoantigenic uveitis.
6 Multiple sclerosis.
14
Sarcoidosis:
• Sarcoidosis. White cellular
masses (“balls”) are seen in
the vitreous compartment on
the surface of the inferior
15
• neural retina, along with early
“candle wax drippings.”
• Candle wax drippings are
caused by perivascular retinal
granulomatous infiltration.
• White balls are caused b
y
accumulations of granulomatous inflammation in the vitreous.
• large Dalen–Fuchs nodule is
seen in this case of sarcoidosis.

16
Masquerade Syndromes:
• Defined as those conditions that includes, as part of their
clinical findings, the presence of intraocular cells but not due to
immune- mediated uveitis entities.
Masquerade Syndromes:
• A- Non- neoplastic syndromes
• B- Neoplastic syndromes
• non-neoplastic Masquerade syndromes:
1 Retinitis pigmentosa.
2 Ocular ischemic syndrome.
3 Chronic Rhegmatogenous retinal detachment.
4 Intraocular foreign body.
5 Pigment dispersion syndrome.
• Neoplastic masquerade syndromes:
1 Primary CNS Lymphoma.
2 Secondary to systemic lymphoma.
3 Secondary to leukemia, Uveal melanoma, Retinoblastoma,
Juvenile Xanthogranuloma and metastatic tumors.
General Principles and Treatment Strategies:
• Before starting treatment, a number of consideration should be
taken into account:
1 The majority of patient with uveitis can modify significantly the
coarse of their illness if they receive proper early treatment.
2 It is recommended to work in Multi-disciplinary Units to
facilitate handling of the drugs used and early detection of side
effects.
17
3 Infectious cause and masquerades syndromes should always be
excluded before considering an immune- mediated mechanism.
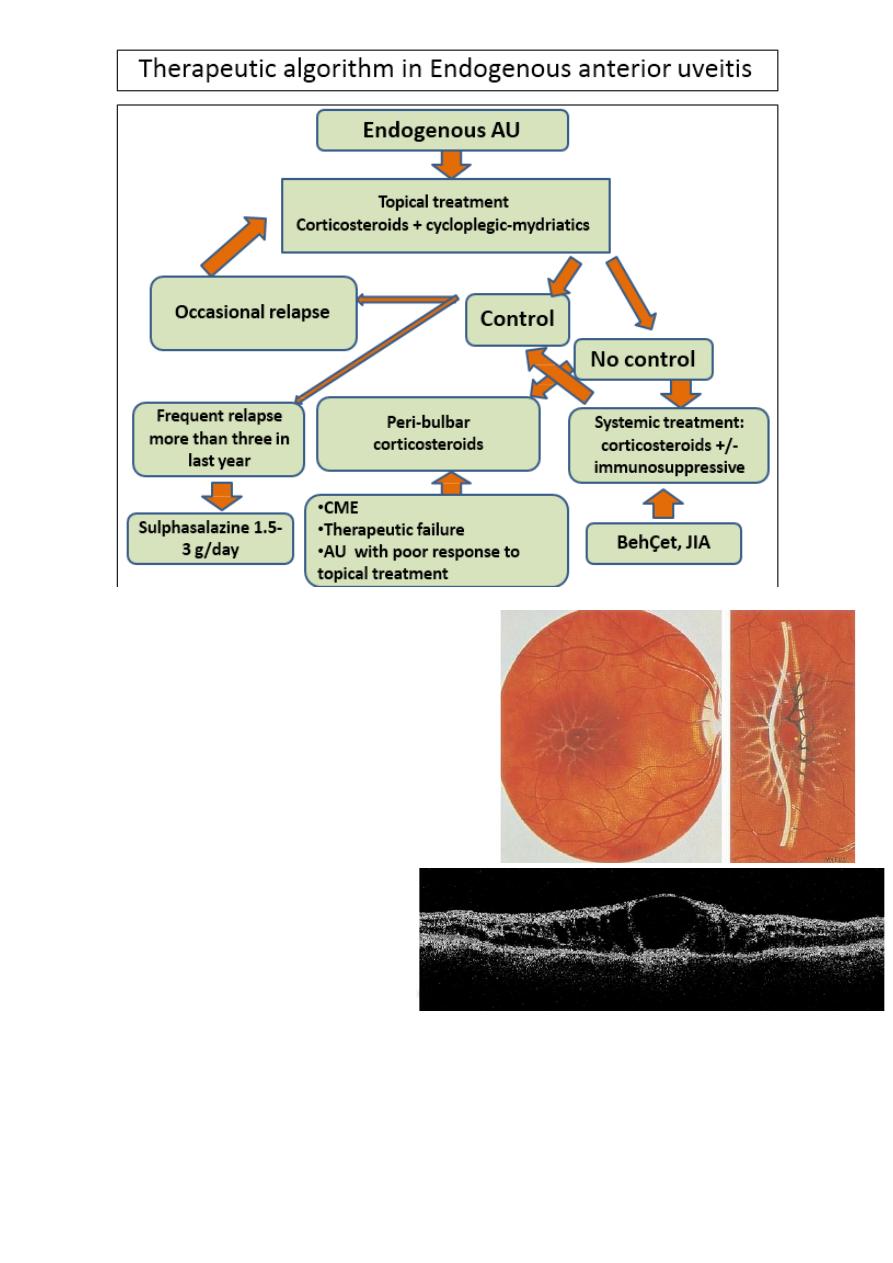
4 Macular edema is the main cause of vision loss in uveitis
patient.
5 Always analyze what is the cause of poor vision in a specific
case. Is it reversible? Are there other causes of poor vision,
Treatment:
• Mydriatics ( short and long acting):
• To promote comfort.
• To break down recently formed synechiae.
• To prevent formation of posterior synechiae.
• Topical steroid;
• Intensive therapy, once inflammation controlled, gradual
therapy.
• Locally injected or systemic corticosteroids and/or
immunosuppressive drugs are usually required in sight –
threatening immune mediated uveitis with involvement of
posterior segment to halt the course of the disease.
Treatment consist in:
1- Phase of induction of remission using high-dose of systemic
corticosteroids administered orally or by means of intravenous
infusion.
2- Phase of maintenance of the long-term control of
inflammatory activity, at this stage, the dose of corticosteroids is
gradually reduced until withdrawal, and if necessary
immunosuppressant′s are added.
Biological therapies, are promising therapeutic options in
refractory patients as a rescue therapy; However, there is clinical
18
Be aware of steroid side
evidence of use of these powerful drugs as first line therapy in
selected cases.
Steroids:
• Systemic steroid.
• Periocular steroids.
• Intraocular steroid.
• Slow release implant.
Due to high efficacy of corticosteroids, it is administered by
different routes, are the drugs of choice in the induction of
remission. However, in many cases corticosteroids are not enough
to sustained control of the inflammation in long term. In other
situations, the control of the inflammatory activity is not
maintained when trying to reduce the dose of corticosteroids, or
side effects of treatment are not tolerable.
In these cases, immunosuppressive treatment for maintenance of
remission is necessary. It is necessary to maintain
immunosuppression for long time, in order to achieve a
stabilization of inflammatory parameters and avoid relapse and
new flares.
Multidisciplinary units (ophthalmologist with internist or
rheumatologist) have been developed to achieve a close follow-up
both at the level of efficacy and early detection of side effects,
allowing better management and control of these therapies.
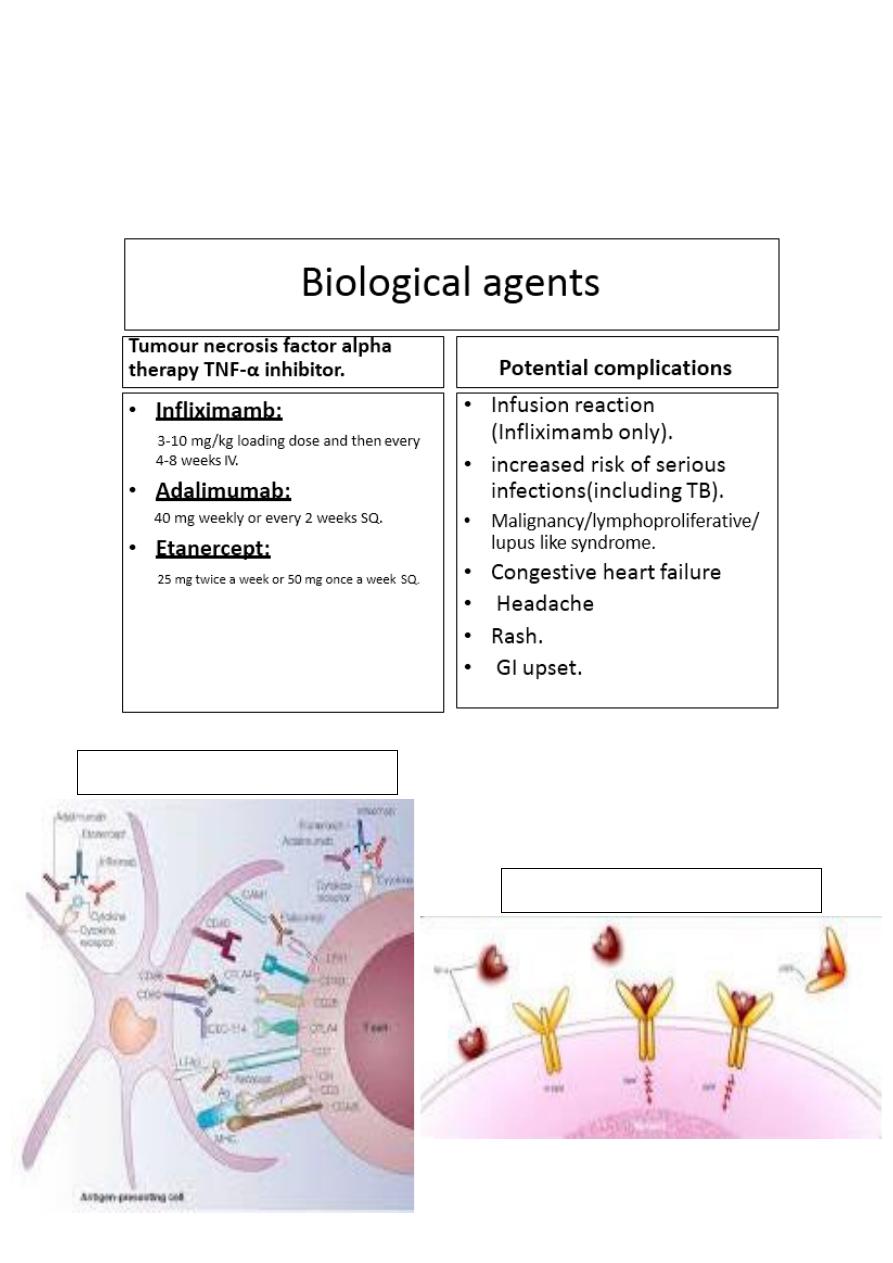
19
Immune modulation
TNF-
α and its receptors
Antimetabolites:
• Steroid spearing therapy and for sight threatening uveitis.
• Azathioprine,
Methotrexate.
20
Infliximamb
21
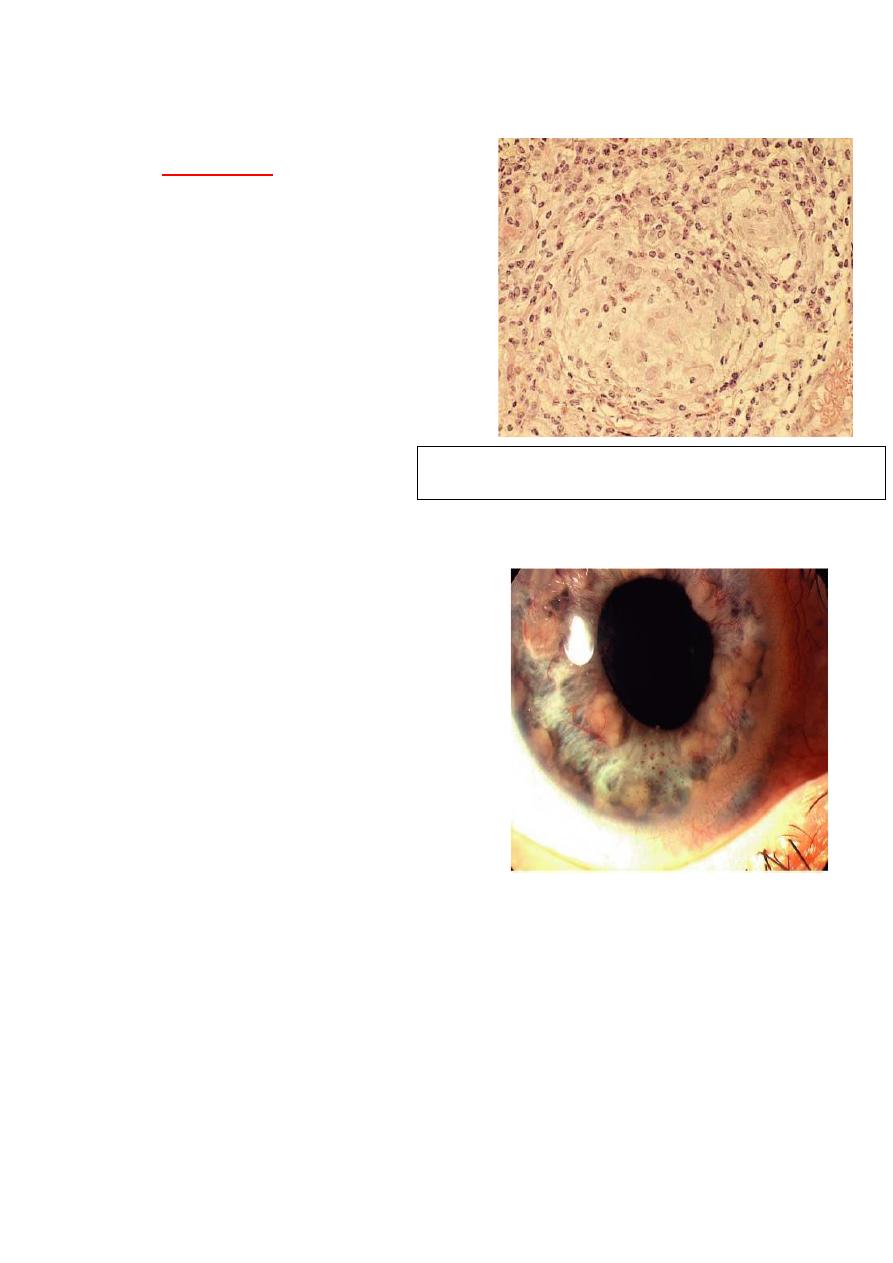
Complications of uveitis Cystoid
macular edema (CME):
• Fluid accumulation in outer
Plexiform and inner nuclear
layers of retina with
formation of cyst like changes.
• Find out what factors, as well as
inflammation, may be
influencing the visual
loss of the patient and
their reversibility.
• There can be co-
morbidities such as
glaucoma, persistent vitreous opacities, cataract or macular
ischemia that have their particular management. It also kept in
mind that some lesions are irreversible (macular or optic
atrophy, advanced glaucoma…) before starting
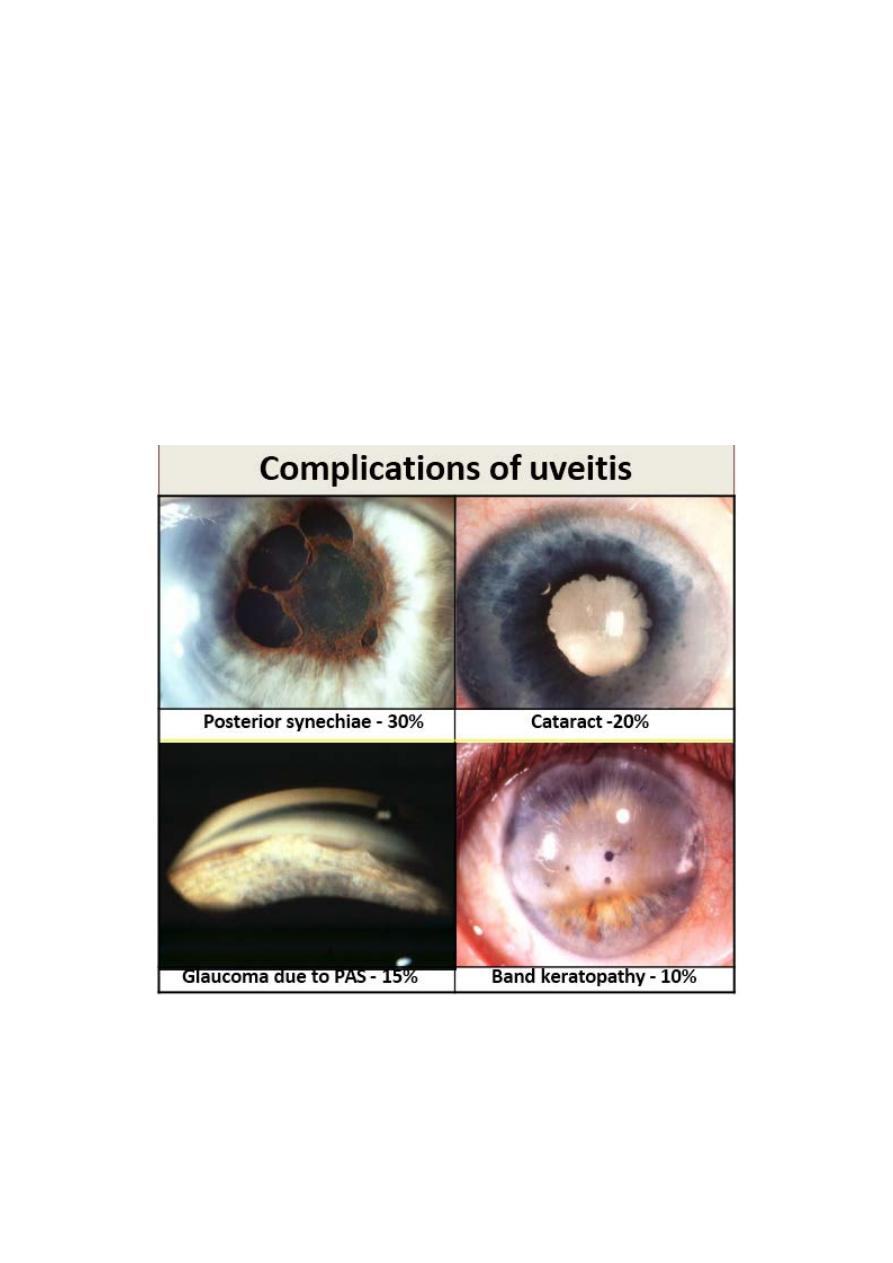
22
immunosuppressive treatment with iatrogenic potential risk in
eyes without the possibility of visual recovery.
• The most frequent causes of loss of visual acuity in those with
uveitis is macular edema (ME). When ME is chronic produces
lesions in the retinal photoreceptors, which can potentially be
irreversible. For this reason, early and appropriate treatment is
essential.
• We must always consider is a general attitude of zero tolerance
to inflammation. Sustained inflammation, even in low grade,
can cause severe structural damage.
