FUNGAL INFECTION
Dr.Anfal Layth Al HarbawiArab board of dermatology
objectives
To know the general point about fungus and fungal infectionTo know the types of fungal infections
To identify every disease and their presentation and their characterized manifestation
To differentiate between disease types
How to diagnose the fungal infection
And treatment
Key feature
Aerobic organisms that contain a true nucleus “Eukaryotic”. The cytoplasm is enclosed by a rigid cell wall composed of cellulose & chitin. Their cell membranes contain ergosterol.
Fungi reproduce by both sexually and asexually by different kinds of spores.
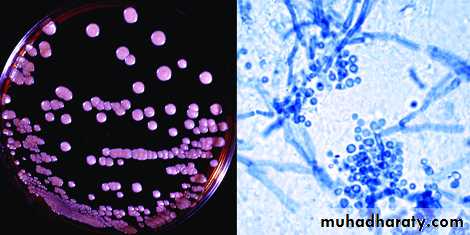
pathogens: Yeasts:Unicellular oval to round cells, reproduce by budding or fission and form moist colonies.Like Candida spp. Malassezia spp
Molds: Filamentous fungi, characterized by tubular branching cells called hyphae, which form fuzzy, velvety or smooth colonies like Dermatophytes and Select nondermatophyte molds
common cutaneous fungal infections, and theyare subdivided into three major groups: (1) “superficial”; (2) “subcutaneous”; and (3) “deep” or systemic
SUPERFICIAL MYCOSES
Superficial mycoses are due to fungi that only invade fully keratinized tissues, i.e. stratum corneum, hair, and nails.They can be further subdivided into those that induce minimal, if any, inflammatory response, e.g. tinea (pityriasis) versicolor, and those that lead to more substantial cutaneous inflammation, e.g. dermatophytoses
Non-inflammatory superficial mycosesTinea versicolor: pityriasis versicolor, tinea flava
It is superficial mycoses caused by Malassezia species M.furfur (came to be recognized as the causative microbe). More recently, found that M. globosa (as a major causative organism).Note
Malassezia spp. normally live on human skin in amounts too minute to be detectable on potassium hydroxide (KOH) examination of stratum Corneum. Tinea versicolor occurs when the round yeast form transforms to the mycelial form.
Factors that can promote this conversion include
high ambient temperatures and humidity,oily skin(Because this yeast is lipophilic, use of bath oils and skin lubricants may also encourage its growth)
Excessive sweating,
immunodeficiency,
poor nutrition,
pregnancy, and
Corticosteroid use.
.
Clinical features
Patients usually present with multiple oval-to-round macules, patches or thin plaques with mild, fine scale.Seborrheic regions, in particular the upper trunk and shoulders, are the favored sites. Less frequently, lesions are seen on the face (especially in children), scalp, antecubital fossae, submammary region, and groin.
The most common colors are brown (hyperpigmented)and whitish-tan (Hypopigmentation which may be secondary to either reduced tanning or inhibition of melanin production by dicarboxylic acids )
In general, tinea versicolor is asymptomatic and the major concern is its appearance.
Diagnosis
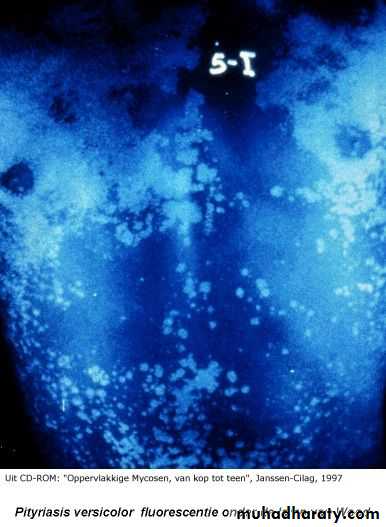
clinicallyWood’s light examination revealing bright yellow fluorescence
and then direct microscopy of scales can confirm the diagnosis of tinea versicolor(both hyphal and yeast forms are seen; although likened to “spaghetti and meatballs”
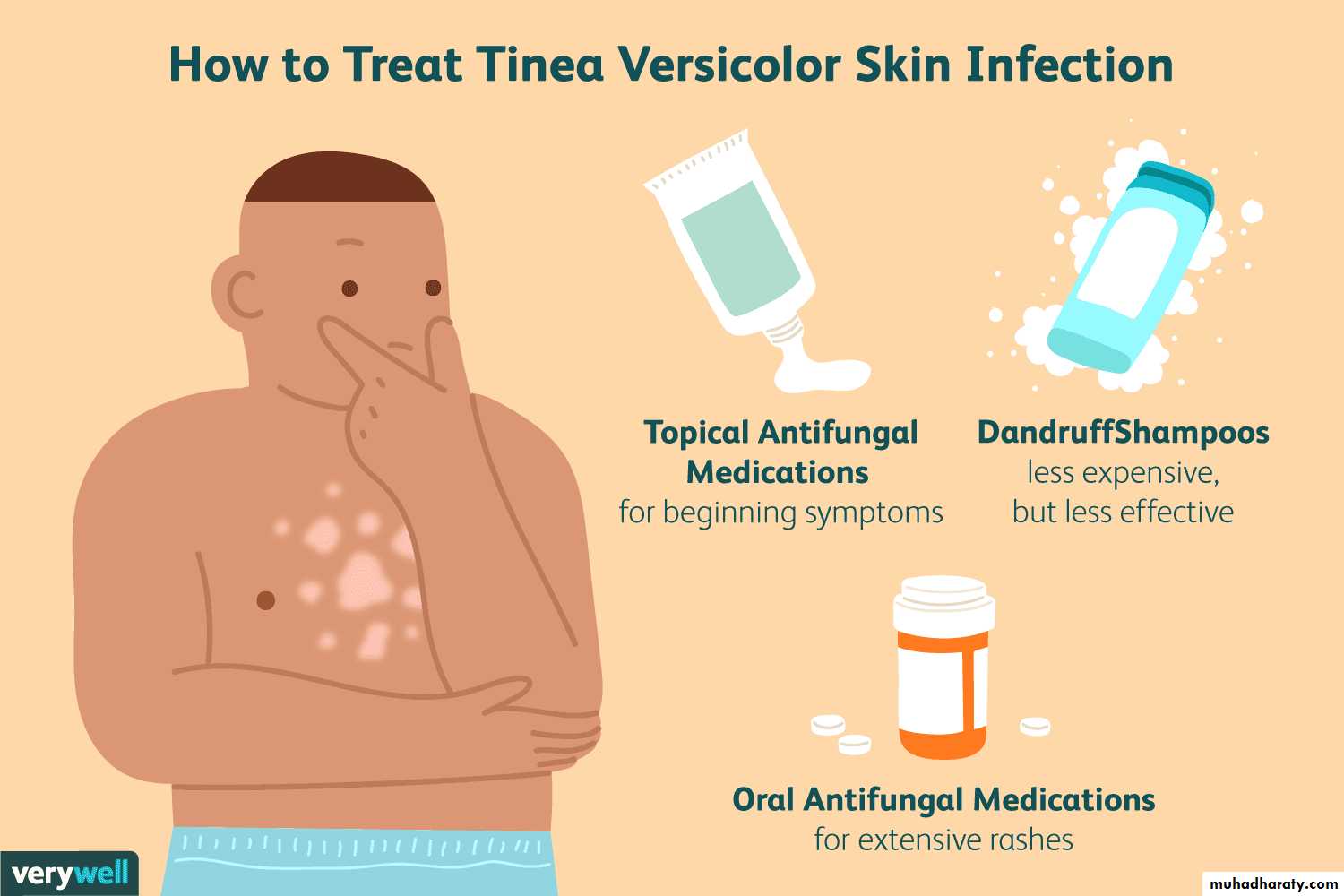
treatment
Tinea versicolor usually responds to topical antifungal ( ketacanazole ) or selenium sulfide shampoo( put it few minutes the rinse it daily for 7-10 days )oral treatment with fluconazole or itraconazole can be considered when there is more extensive involvement.
Residual pigmentary changes often require weeks to months to resolve
inflammatory superficial mycosesDermatophytoses
are fungal infections caused by three genera of fungi that have the unique ability to invade and multiply within keratinized tissue (hair, skin, and nails).The three genera are Microsporum, Trichophyton, and Epidermophyton.
We divided the disease
A. In naming clinical infections due to dermatophytes, “tinea” precedes the Latin name for the involved body site, e.g. “tinea pedis” refers to a dermatophyte infection of the foot.
B.Types of dermatophytes based on mode of transmission.
Types of dermatophytes based on mode of transmission.
TYPES OF DERMATOPHYTES BASED ON MODE OF TRANSMISSIONCategory
Mode of transmissionMild to non-inflammatory,
chronic
Anthropophilic
Human to human
Intense inflammation
(pustules and vesicles
possible), acute
Zoophilic
Animal to human
Intense inflammation
(pustules and vesicles) acute
Geophilic
Soil to human or animal
Moderate inflammation
Pathogenesis
Dermatophytes, unlike most other fungi, produce keratinases
(enzymes that break down keratin), which allow invasion of the fungi into the stratum corneum
The severity of clinical disease is also affected by several host factors.
• Sebum has an inhibitory effect on dermatophytes, and the degree of disease activity may be related to the number and activity of sebaceous glands in a particular body region.
• Breaks in the skin barrier or macerated skin encourage dermatophyte invasion,
• and increased susceptibility related to immunologic factors may be inherited.
• Other conditions influencing dermatophyte infections include skin disorders that affect cutaneous barrier function, such as ichthyoses
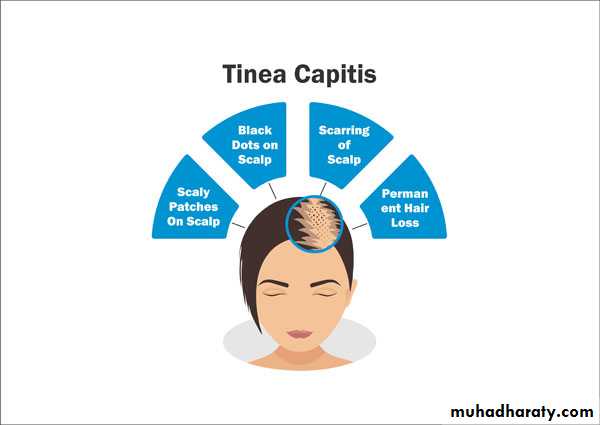
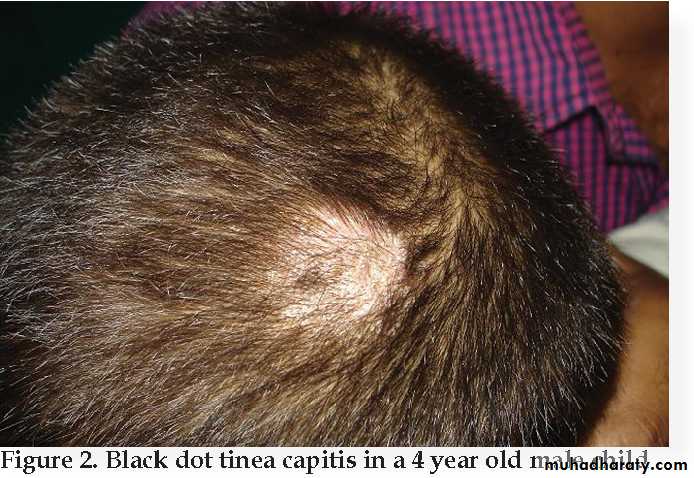
Tinea capitis
Tinea capitis is a common dermatophyte infection of the scalp in children,whereas adult infection occurs infrequently.The causative pathogens are members of only two genera: Trichophyton and Microsporum.
T. tonsurans is currently the most common cause of tinea capitis in the US (accounting for >90% of cases).
Clinical varieties of tinea capitis
• The endothrix patternresults from infection with anthropophilic fungi nonfluorescent
The clinical presentation varies from scaling to “black dots” with patchy alopecia .( black docts occur as affected hair breaks at the surface of scalp)
T. tonsurans and T. violaceum are important causes of endothrix infection.
2. The ectothrix pattern
occurs when arthroconidia are formed from fragmented hyphae outside the hair shaftCuticle destruction ensues.
Ectothrix infection can be fluorescent (Microsporum) or non-fluorescent (Microsporum and Trichophyton), as determined by Wood’s lamp examination.
Clinical features vary from patchy, scaly alopecia with little inflammation that may mimic alopecia areata (scaly tinea capitis).
3. Favus
Favus is the most severe form of dermatophyte hair infection andis most frequently caused by T. schoenleinii.
Hyphae and air spaces are observed within the hair shaft, and a bluish-white fluorescence by Wood’s light examination is typically seen.
Favus presents as thick, yellow crusts composed of hyphae and skin debris (“scutula”). Scarring alopecia may develop in chronic infections
4. Kerion
A kerion results from advanced disease coupled with an exaggerated host response that leads to boggy, purulent plaques with abscess formation and associated alopeciaNote: If a kerion is misdiagnosed as a bacterial abscess and treated with antibiotics following incision and drainage, the infection will likely worsen, thereby increasing the likelihood of scarring alopecia.
Carrier state
The “carrier state” of T. tonsurans refers to a clinical situation in which there are no obvious signs or symptoms of a scalp infection, yet a positive fungal culture is obtained.Although also seen in children, this typically occurs in adults who have been exposed to infected children.
treat all carriers with oral or topical antifungals.
Treatment
Oral therapy is required, as the drug must penetrate the hair follicle to be effective.Preventative measures are also important in the management of tinea capitis. Because the disease is contagious, all individuals residing with the infected patient should be examined for signs of tinea capitis and appropriately treated.
Appropriate adjunctive treatment: regular (e.g. every other day) use of an antifungal shampoo, such as 2% ketoconazole or 2.5% selenium sulfide, until the patient is free of disease.
Tinea corporis
Tinea corporis is a dermatophyte infection of the skin of the trunk and extremities, excluding the hair, nails, palms, soles, and groin.Any dermatophyte can potentially cause tinea corporis, but T. rubrum is the most common pathogen worldwide, followed by T. mentagrophytes
Transmission
• human-to-human (including autoinoculation, e.g. from tinea capitis or pedis)• animal-to-human (often transmitted by domestic animals),
• soil-to-human spread
Sources include occupational or recreational exposure (e.g. military ,housing, locker rooms, outdoor activities) and contact with contaminated clothing or furnitur
Clinical features
Asymptomatic round or polycyclic circumscribed scaly area with central clearing ( as Infection spreads centrifugally from the point of skin invasion with central clearing of the fungus,) with active margin.Scaly lesion
Variable degree of inflammation may be pustular
Associated symptoms may include pruritus and burning.
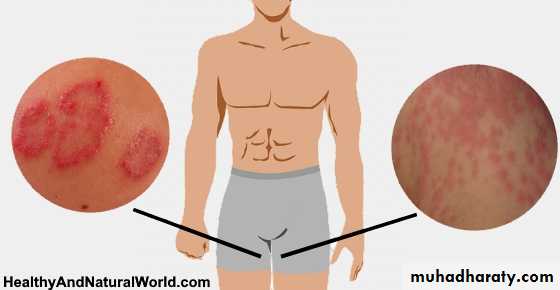
Tinea cruris
Tinea cruris is a dermatophyte infection of the inguinal region, in particular the inner aspects of the upper thighs and crural folds, with occasional extension onto the abdomen and buttocks.Thethree most common causative agents are Epidermophyton floccosum, T. rubrum, and T. mentagrophytes
.
This condition is more often seen in men than in women, since the scrotum provides a warm and moist environment that encourages fungal growth and men are more likely to have tinea pedis and onychomycosis as a source of dermatophytes.
Other predisposing factors include obesity and excessive perspiration, prolonged wearing of wet bathing suits and diabetes
Tinea cruris is frequently associated with tinea pedis because clothing that is brought over the feet is contaminated and then comes in contact with skin in the groin region
Clinical features
The initial sign of infection is usually an area of erythema and pruritus in the fold between the scrotum and the inner thigh.Characteristic lesions are sharply demarcated with a raised, erythematous, scaly advancing border that may contain pustules or even vesicles.
In contrast to candidiasis the scrotum is usually spared.