Fungal infection 2
Dr Anfal Layth Al harbawiArab board of dermatology
Tinea manuum
Dermatophyte infections on the dorsal aspect of the hand have a clinical presentation similar to tinea corporis. However, dermatophyte infection of the palm and interdigital spaces,
The typical causative organisms are T. rubrum, T. mentagrophytes, and E. floccosum.
. Tinea manuum is usually non-inflammatory and often unilateral (“two feet and one hand syndrome”) (as Moccasin-type tinea pedis is often present in patients with tinea manuum)
there is hyperkeratosis of the palms and digits, includingwithin creases, that fails to respond to emollients
Tinea barbae
Tinea barbae is a dermatophytosis that involves the bearded areas of the face and neck in men.Because the disease is often acquired from animals, the causative organisms are typically zoophilic dermatophytes,
namely microsporum canis
With the increased use of disposable razors and disinfectants, the incidence of tinea dramatically reduced.
the clinical presentation tends to be severe, with intense inflammation and multiple follicular pustules.
Abscesses, sinus tracts, bacterial superinfection, and kerion-like boggy plaques can develop.
Patients may have constitutional symptoms such as malaise as well as lymphadenopathyand even scarring alopecia
Tinea pedis
is a dermatophyte infection of the soles and interdigital web spaces of the feet.This condition is more common in adults than children and is found around the world, affecting both sexes.
The lack of sebaceous glands and the moist environment created by occlusive shoes are important factors in the development of tinea pedis
In fact, tinea pedis is uncommon in populations that do not wear shoes.
However, the fungus may be acquired from going barefoot (locker rooms, gyms, public facilities).
The dermatophytes that are typically responsible for tinea pedis areT. rubrum, T. interdigitale
CLINICAL TYPES OF T. PEDIS
TypeCausative organism
• Clinical features
Moccasin
Trichophyton rubrumDiffuse hyperkeratosis, erythema scaling and
fissures on one or both plantar surfaces
Interdigital
T. interdigitale
Most common type; erythema, scaling, fissures and maceration in the web spaces; the two lateral web spaces are most commonly affected;
“dermatophytosis complex” (fungal infection
followed by bacterial invasion†) can develop;
pruritus common; may extend to dorsum and soleof foot
Inflammatory
(vesicular)T. mentagrophytes
Vesicles and bullae on the medial foot
Ulcerative
T. rubrumT. interdigitale
Typically an exacerbation of interdigital tinea pedis; ulcers and erosions in the web spaces;
commonly secondarily infected with bacteria; seen
in immunocompromised and diabetic patients
Tinea unguium (dermatophytic onychomycosis)
Onychomycosis is a term used to encompass all fungal infections of the nail and includes those due to dermatophytes as well as nondermatophytes.It is divided into three patterns based upon the point of fungal entry into the nail unit:
TYPES
CLINICAL FEATURESdistal/lateral subungual,
ith invasion via the hyponychium (mostcommon;
superficial white,
with direct penetration into (and usually confinement to) the dorsal surface of the nail plate (often due to T. interdigitale;
proximal subungual
with invasion under the proximal nail fold(frequently in immunocompromised hosts as with HIV infection)Mixed type
with ≥2 of the above patterns in the same nailOnychomycosis can be challenging to manage due to difficulties in diagnosis, the requirement for long treatment periods, potential side effects of systemic medications, and frequent recurrences.
patients with the condition complain of discomfort and pain associated with trimming the nails, running, and other activities such as dancing.
In addition, serious complications such as cellulitis can result from onychomycosis ,especially in patients who are diabetic or immunocompromised.
Diagnosis
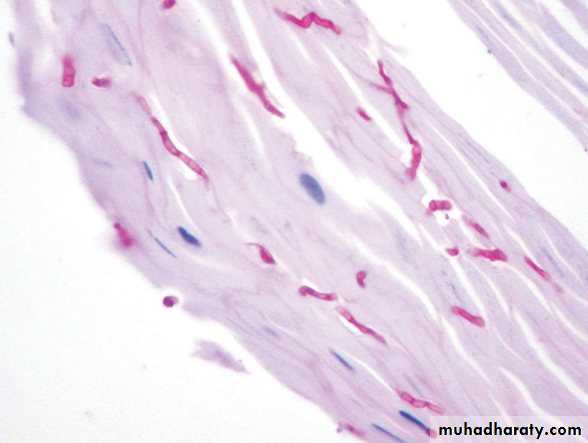
Tinea pedis, manuum, faciei, cruris, and corporis are usually diagnosed via KOH examination
If biopsies are performed of cutaneous dermatophyte infections, hyphae are seen within the stratum corneum;
Wood s light
treatment
Topical antifungals are the first-line treatment for many patients with uncomplicated, localized cutaneous dermatophyte infections such as tinea corporis, tinea cruris, and tinea pedisSystemic antifungal therapy, is typically
required to cure tinea manuum, capitis, and unguium.
In general, oral treatment is also needed for infections involving extensive areas of skin,
in hairy sites other than the scalp (e.g. tinea barbae),
or associated with excessive inflammatory reactions
Tinea incognito
The inflammatory response may be totally suppressed by steroids (systemic or topical) raised margin, inflammation & scaling are reduced. Bruise-like brownish discoloration is seen. If steroid is stopped for few days, scrapings will yield +ve resultswood s light
UV radiation is passed through a nickel oxide filter, producing light at a wave length of about 365nm. It will help with the examination of some skin conditionsPityriasis Versicolor……..yellow.
Erythrasma ………coral red.
Disorders of pigmentation ……epidermal melanin pigmentation is markedly enhanced, while the dermal melanin pigmentation doesn’t become accentuated. Hypomelanosis……. appears whiter.
Dermatophytids
In cases of inflammatory tinea capitis, tinea pedis.widespread “id” eruptions may appear concomitantly on the trunk and extremities.
These are vesicular, lichenoid, papulosquamous, or pustular.
They represent a systemic reaction to fungal antigens.
Although they are commonly refractory to topical corticosteroids,
they typically clear rapidly after treatment of the fungal infection.
Candidiasis
candidiasis has a wide spectrum of clinical presentations.Early descriptions of oral candidiasis (thrush) were made by Hippocrates.
Candida albicans is a classic opportunistic pathoge
One or more predisposing factors such as obesity, moisture and maceration, immobility, diabetes, pregnancy, the use of broad-spectrum antibiotics, or perhaps the use of the contraceptive pill, will often be found to be playing some part.
Cutaneous Candida infections present with markedly erythematous, sometimes erosive, patches that are often accompanied by satellite papules
The most common sites of involvement are intertriginous zones (e.g. submammary, beneath pannus, inguinal creases, intergluteal fold) and the scrotum, as well as the diaper area in infants.
Candida can also infect periungual areas (e.g. in the setting of chronic paronychia), nails
and the web space between the third and fourth fingers (erosio interdigitalis blastomycetica, especially in individuals whose hands are frequently exposed to water
Perleche (angular cheilitis)
is characterized by maceration and transverse fissuring of the oral commissurs. The earliest lesions are ill-defined, grayish-white, thickened areas with slight erythema of the mucous membrane at the oral commissure.Diaper candidiasis
The diagnosis of candidiasis may be suspected by the finding of involvement of the folds and occurrence of many small erythematous desquamating "satellite" or "daughter" lesions scattered along the edges of the larger.Topical anticandidal agents are effective.
Recurrent diaper Candida may be associated with oral and gut colonization and may respond to the addition of oral nystatin suspension
paronychia
Acute paronychia is usually bacterial, but in chronic paronychia Candida may be the sole pathogen, or be found with other opportunists such as Proteus or Pseudomonas sp.The proximal and sometimes the lateral nail folds of one or more fingers become red .
The cuticles are lost and small amounts of pus can be expressed. The adjacent nail plate becomes ridged an discoloured.
Predisposing factors include wet work, poor peripheral circulation and vulval candidiasis