• Gastroesophageal Reflux Disease
• (GERD)• GER signifies the retrograde movement of gastric contents across the LES into the esophagus & is usually physiological in young infant.
• GERD symptoms or complications resulting from exposure of esophagus, oropharynx, or airway to gastric refluxate (acid, food, bile);
• i.e. pathological GER
Measurement of lower esophageal pH shows that in normal individuals there is acidity from reflux of stomach contents for ˂ 4% of 24-hr period.
Transient LES relaxation (TLESR) is the primary mechanism allowing reflux to occur.
It is common in 1st yr of life. By 12 ms of age, nearly all symptomatic reflux will have resolved spontaneously, presumably due to a combination of:
maturation of LES, assumption of an upright posture & more solids in the diet.
• Clinical Manifestations :• Infantile reflux manifests more often with regurgitation (especially postprandially), signs of esophagitis (irritability, arching, choking, gagging, feeding aversion) FTT
• Older children can have regurg during preschool yrs; complaints of abdominal & chest pain supervene in later childhood & adolescence.
• Occasional children present with neck contortions (arching, turning of head), designated Sandifer syndrome.
• The respiratory presentations:
• infants : obstructive apnea, stridor or lower airway disease in which reflux complicates primary airway disease such as laryngomalacia or BPD.
• older children commonly related to asthma or laryngitis or sinusitis.
• Infant reflux becomes evident in the 1st few ms of life, peaks at ∼4 mo, resolves in up to 88% by 12 mo & nearly all by 24 mo.
• Symptoms in older children tend to be chronic, waxing & waning, but completely resolving in no ˃ half, which resembles adult patterns.
• Diagnosis:
• For most of the typical GERD , thorough Hx & PE suffice initially to reach Dx .• Contrast (usually barium) radiographic study of eso. & upper GIT is performed in pt with vomiting & dysphagia to evaluate for achalasia, esophageal strictures & stenosis, H.H, & gastric outlet or intestinal obstruction.
• It has poor sensitivity & specificity due to inability to differentiate physiologic GER from GERD.
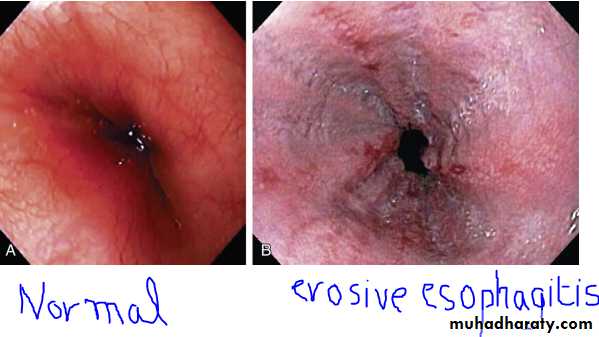
• Endoscopy allows Dx of erosive esophagitis & complications such as strictures or Barrett esophagus;
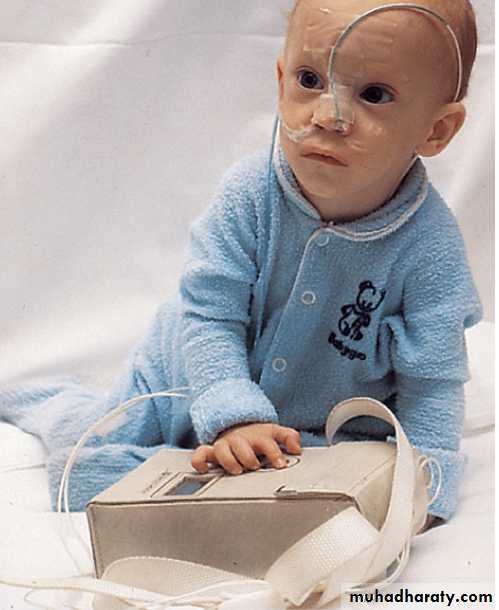
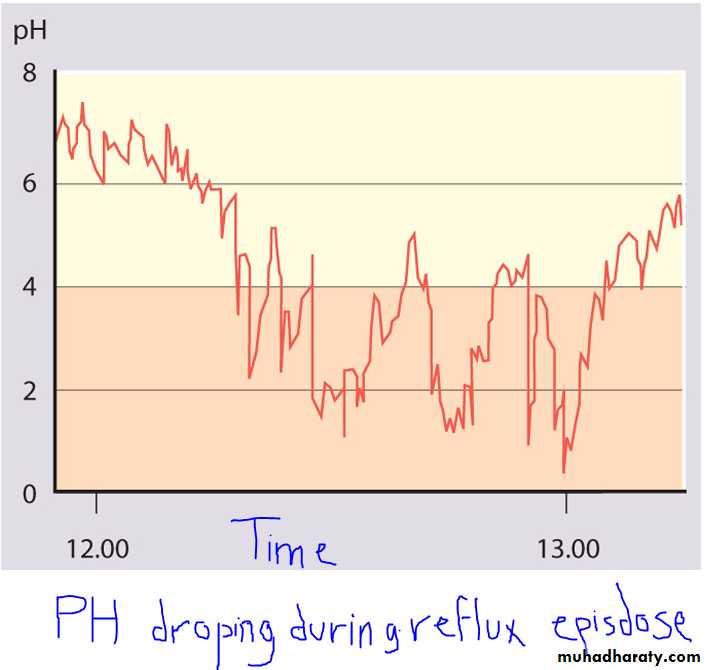
• Extended esophageal pH monitoring of the distal esophagus:
• no longer considered necessary for GERD Dx, provides a quantitative & sensitive documentation of acidic reflux episodes.• The most important indications for eso pH monitoring are for :
• assessing efficacy of acid suppression during Rx, evaluating apneic episodes evaluating atypical GERD presentations such as chronic cough, stridor & asthma.
PH study in GERD
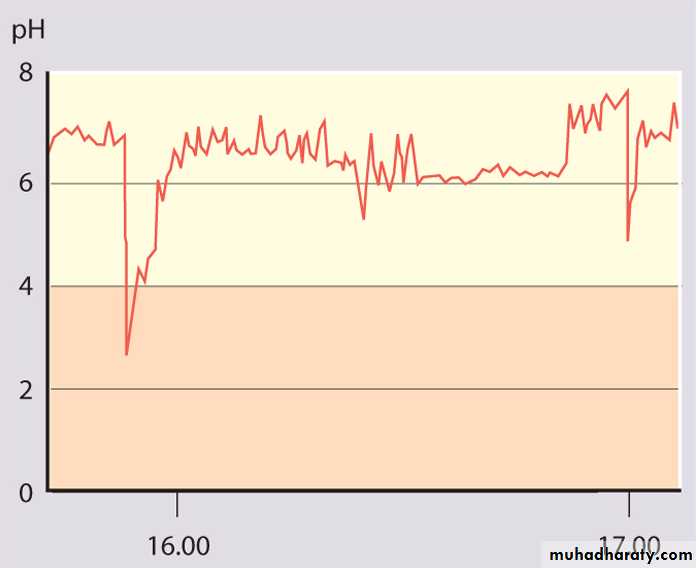
Part of a normal oesophageal pH study.
The lower oesophageal pH is above 4 for most of the time.• Management:
• Dietary measures for infants include normalization of any abnormal feeding techniques, volumes & frequencies.• Thickening of feeds or use of commercially prethickened formulas ↑ % of infants with no regurgitation, ↓ the frequency of daily regurgitation & emesis & ↑ infant's wt .
• The addition of a Tbsp of rice cereal/ oz of formula results in a greater caloric density (30 kcal/oz) & reduced crying time, although it might not modify the number of nonregurgitant reflux episodes.
A short trial of a hypoallergenic diet may be used to exclude milk or soy protein allergy before pharmacotherapy.
Older children should be counseled to avoid acidic or reflux-inducing foods (tomatoes, chocolate, spicy foods , mint) & beverages (juices, carbonated & caffeinated drinks, alcohol), avoiding lying down after meals
Weight reduction for obese & elimination of smoke exposure
• Positioning measures important for infants, who cannot control their positions independently.• Seated position worsens infant reflux should be avoided.
• When the infant is awake & observed, prone position & upright carried position can be used to minimize reflux.
• The efficacy of positioning for older children is unclear, but some evidence suggests a benefit to left side position & head elevation during sleep.
• Pharmacotherapy to ameliorate gastric acidity
• Antacids: most commonly used antireflux & available .• relieve symptoms by acid neutralization.
• SE : diarrhea (Mg antacids) & constipation (Al antacids) .
• Histamine-2 receptor antagonists (H2RAs: cimetidine, famotidine, nizatidine, & ranitidine)
• widely used, there is a definite benefit in Rx of mild-to-moderate reflux esophagitis.
• PPIs (omeprazole, lansoprazole………)
• provide the most potent antireflux effect• rabe-&panto- are not FDA-approved in children.
• Prokinetic agents:
• metoclopramide (dopamine-2 and 5-HT3 antagonist), bethanechol (cholinergic agonist), and erythromycin (motilin receptor agonist).
• Most of these ↑ LES pressure; some improve gastric emptying or esophageal clearance.
• Baclofen is a centrally acting (GABA agonist) that has been shown to ↓ reflux by ↓ TLESRs in healthy adults & in a small number of neurologically impaired children with GERD.
• Surgery, usually fundoplication
• is effective therapy for intractable GERD in children, particularly those with refractory esophagitis or strictures & those at risk for significant morbidity from chronic pulmonary disease.
• Complications of GERD:
• Reflux is often problematic:
• in children with CP or other neuro developmental disorders
• in preterm infants who develop BPD
• following surgery for esophageal atresia or diaphragmatic hernia.
• 1.Esophageal:
• Esophagitis• Prolonged & severe esophagitis strictures
• Long-standing esophagitis predisposes to Barrett esophagus, a precursor of esophageal adenocarcinoma.
2.Nutritional:
Esophagitis & regurgitation may be severe enough to induce FTT bec of caloric deficits.
• 3. Extraesophageal:
• Respiratory (“Atypical”): chronic cough, stridor & hoarseness, aspiration pneumonia & chronic pulmonary fibrosis• Often, GERD & primary respiratory disorder, such as asthma, interact & a vicious cycle between them worsens both diseases.
• Hypertrophic Pyloric Stenosis
• It is hypertrophy of the pylorus causing gastric outlet obstruction. It is more common in boys (4 : 1), particularly first-borns, there may be a family Hx, especially on the maternal side.
• The incidence is ↑ in infants with B & O bd groups. It is occasionally associated with other congenital defects, including TEF.
• Etiology
• unknown .
• PS is usually not present at birth .
• An association has been found with the use of erythromycin in neonates with highest risk if the medication is given within the 1st 2 wk of life.
• deficiency of nitric oxide, a mediator of smooth-muscle relaxation, may be associated with the development of PS because NO synthase is selectively depleted in pt with PS.
• Clinical Manifestations:
• Nonbilious vomiting is the initial symptom of PS. The vomiting may or may not be projectile initially but is usually progressive, occurring immediately after a feeding.• The vomiting usually starts after 3 wk of age ( irrespective of GA), but symptoms can develop as early as the 1st wk of life and as late as the 5th mo.
• About 20% have intermittent emesis from birth that then progresses to the classic picture.
• After vomiting, the infant is hungry & wants to feed again.
• Persistent vomiting results in the continuous loss of gastric HCl. Dehydration causes ↑ in aldosterone production, leading to ↑ renal excretion of K+ hypochloremic, hypokalemic metabolic alkalosis.
• The depletion of Cl- in bd leads to an exchange of H+& K+ for Na in the distal tubule, resulting in a paradoxical aciduria.
• Hypoglycemia may be present & may cause seizures.
Pathophysiology:
• Hyperbilirubinemia is the most common clinical association of PS, also known as icteropyloric syndrome. Unconjugated hyperbilirubinemia is more common than conjugated & usually resolves with surgical correction.
• It may be associated with ↓ level of glucuronyl transferase as seen in ∼5% of affected infants.
• Other coexistent clinical diagnoses have been described, including:
• eosinophilic gastroenteritis,H.H, peptic ulcer, congenital nephrotic syndrome, CHD & congenital hypothyroidism.
• Diagnosis:
• palpating the pyloric mass( firm, movable, ∼2 cm in length, olive shaped, hard, best palpated from the Lt side.
• The mass is easiest palpated after an episode of vomiting.
• After feeding, there may be a visible gastric peristaltic wave that progresses across the abdomen.
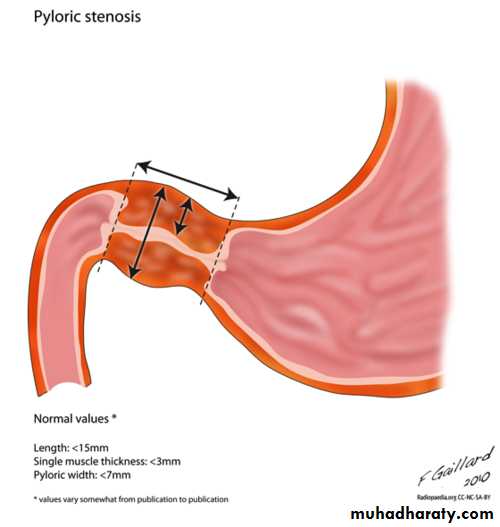
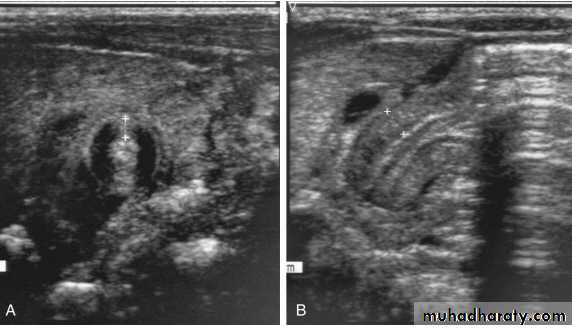
• U/S : confirms Dx in the majority of cases. Criteria include pyloric thickness 3-4 mm, an overall pyloric length 15-19 mm, and pyloric diameter of 10-14 mm. It has a sensitivity of ∼95%.
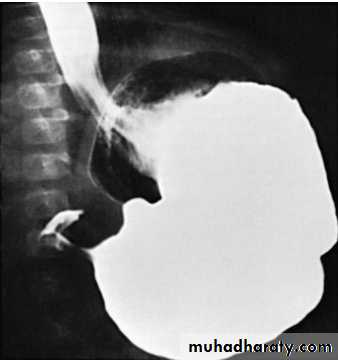
• Contrast studies demonstrate an elongated pyloric channel (string sign), a bulge of the pyloric muscle into the antrum (shoulder sign), and parallel streaks of barium seen in the narrowed channel, producing a “double tract sign”
Visible gastric peristalsis in an infant with pyloric stenosis
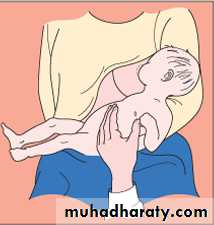
Diagram showing a test feed being performed to diagnose pyloric stenosis
A, Transverse sonogram demonstrating a pyloric muscle wall thickness of >4 mm (distance between crosses). B, Horizontal image demonstrating a pyloric channel length >14 mm (wall thickness outlined between crosses) in an infant with pyloric stenosis.
Barium in the stomach of an infant with projectil
The attenuated pyloric canal is typical of CHPS.• DDx:
• GERD, adrenogenital syndrome, Inborn errors of metabolism………• Rx:
• Preoperative Management
• The anatomic correction of PS is not a surgical emergency because, although PS is a form of intestinal obstruction, gangrene & intestinal perforation do not occur with this condition. Infants should not undergo surgery until the fluid and electrolyte deficits have been corrected.
Surgical Management
Once the volume and electrolyte status is corrected, the infant is ready for surgery (Ramstedt pyloromyotomy)Pyloric stenosis at operation showing pale, thick pyloric muscle and pyloromyotomy incision