Histopathology of Periodontal Disease
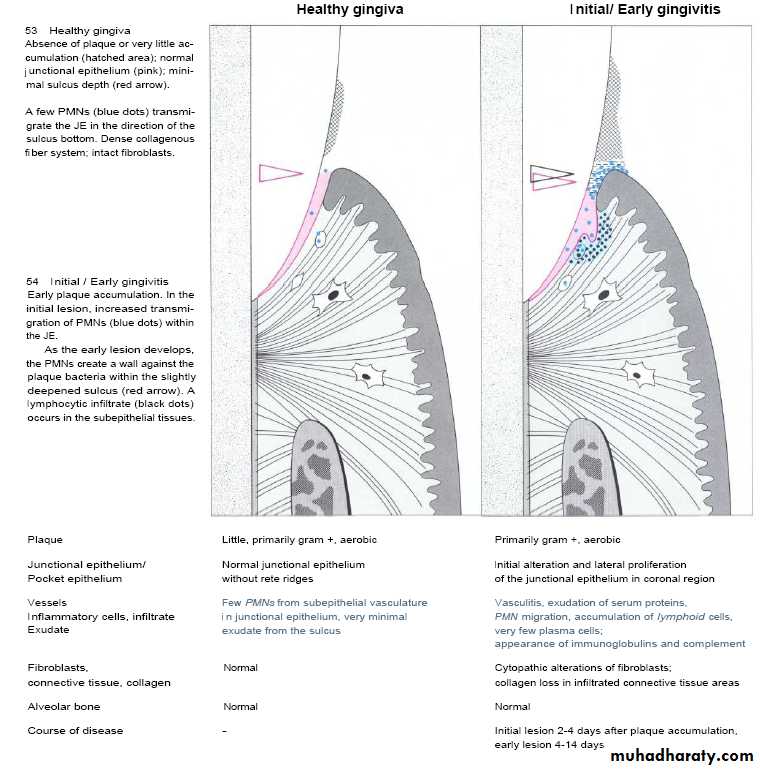
Histopathology of periodontal diseaseNormal Gingiva;
It appears pink color ,firm in consistency, scalloped outline.
Interdental papilla firm & fill gingival embrassure.
No bleeding on probing and knife edge gingival margin.
Few inflammatory cells can be seen in marginal portion.
Histopathology of periodontal disease
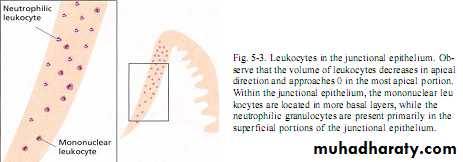
Below junctional epithlium ; microvascular plexus with inflammatory cells.Fluid & plasma protein leak , pass in connective tissue & junctional epithlium into gingival sulcus to form gingival fluid.
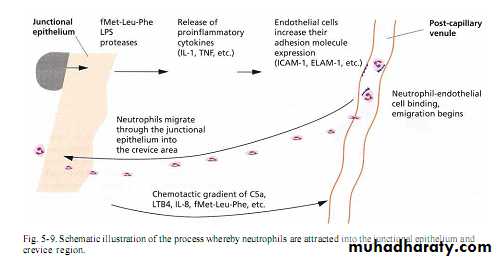
Neutrophiles & Macrophages seen in junctional epithlium that continuously migrate to gingival sulcus which mediated by chemotactic factor from plaque.
”its amount increase with increase gingival Inflammation”
Normal & clinically healthy gingival continuously invaded by microorganisms & deal with this microorganisms by:-
1- outward of gingival fluid flow.
2- killing of microorganisms by neutrophils¯ophage.
3- shedding of microorganisms .
4- destruction by antibodies &/or complements.
5- restriction of massive microbial growth by normal flora.
6- intact epithelial barrier
Gingival inflammation
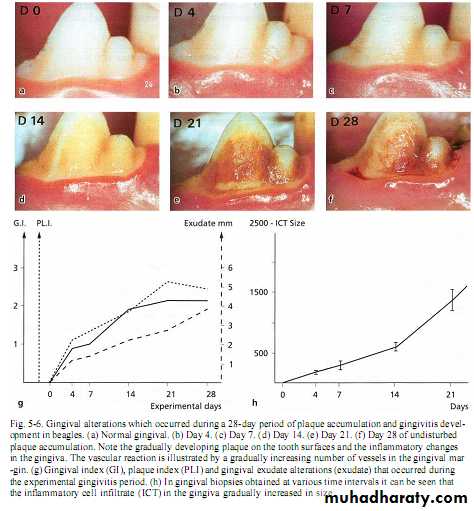
Inflammation develops within second day of undisturbed plaque accumulation .Clinically; slight color & texture changes of marginal gingiva then after 10 -20 days, overt gingivitis with marked redness ,swelling & bleeding on probing (reversible).
Microscopically;Inflammatory cells with reduction of fibroblast & collage fibers with increase volume of intercellular matrix ,degraded collagen, exudative materials & degenerated cells .
The presence of microorganisms in gingival sulcus synthesize products like collagenase,hyaluronidase,protease, chondroitin sulfatase or endotoxin.
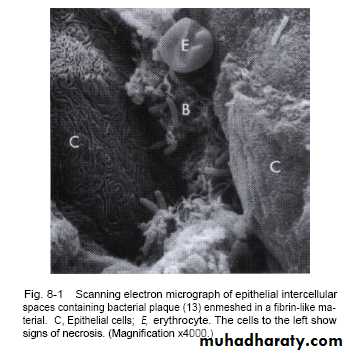
Widening of intercellular space in junctional epithilum permit injurious agents to gain access to connective tissue.
Disease progression
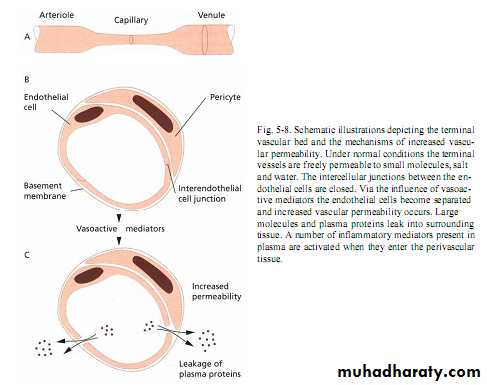
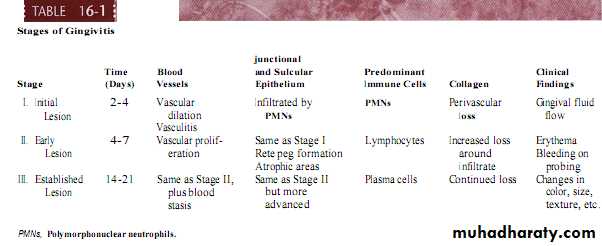
Initial gingival lesionWithin 24h,changes of microvascular plexus that involve;
Dilation of arteriols,capillaries & venuls.Hydrostatic pressure elevated with formation of intercellular gaps of capillaries or venular endothelial cells lead to increase in permeability of veins to fluid & protein.
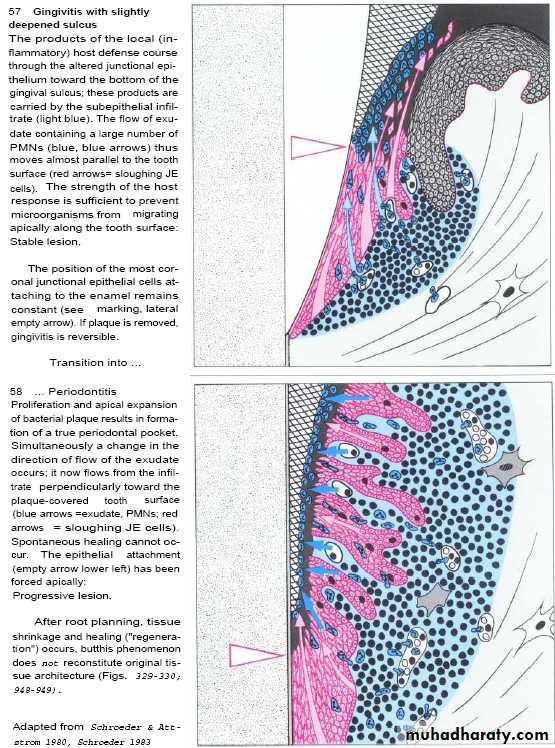
• Flushing of the sulcus to washout the accumulated bacteria.
• Kill the bacteria by antibodies & complement.
• Neutralize the toxin of the bacteria.
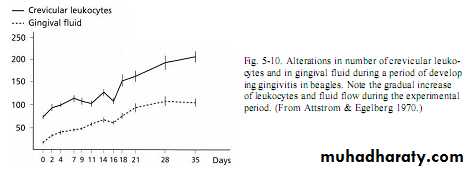
Neutrophil,macrophage & lymphocyte move to the site, first adhere to vessels walls (margination) then leave capillaries by migration through wall then to gingival sulcus to form what is called crevicular leukocytes.
Till this time, the gingivitis is Subclinical .
Disease progression
Early gingival lesion-Occur during forth to seventh days of undisturbed plaque accumulation.
-blood vessels remain dilated.
-More pronounced infiltration of inflammatory cells(mainly lymphocytes 75%) .
• - Proliferation & retepegs formation of junctional epithelium.
• - Its happened through period of 2 weeks.
• - Fibroblast degeneration by action of lymphocytes & decrease capacity of collagen production(70% loss of collagen fibers) mainly in circular & dentogingival fibers.
• - Clinically, there are sign of erythema with bleeding on proping.
Disease progression
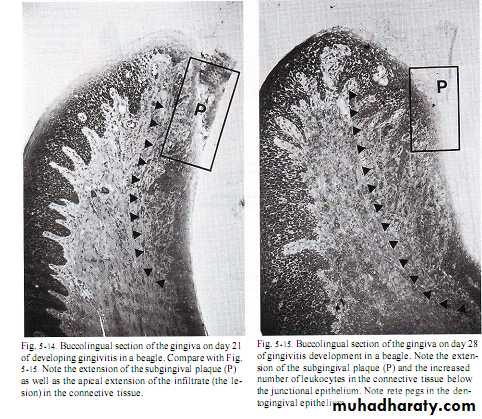
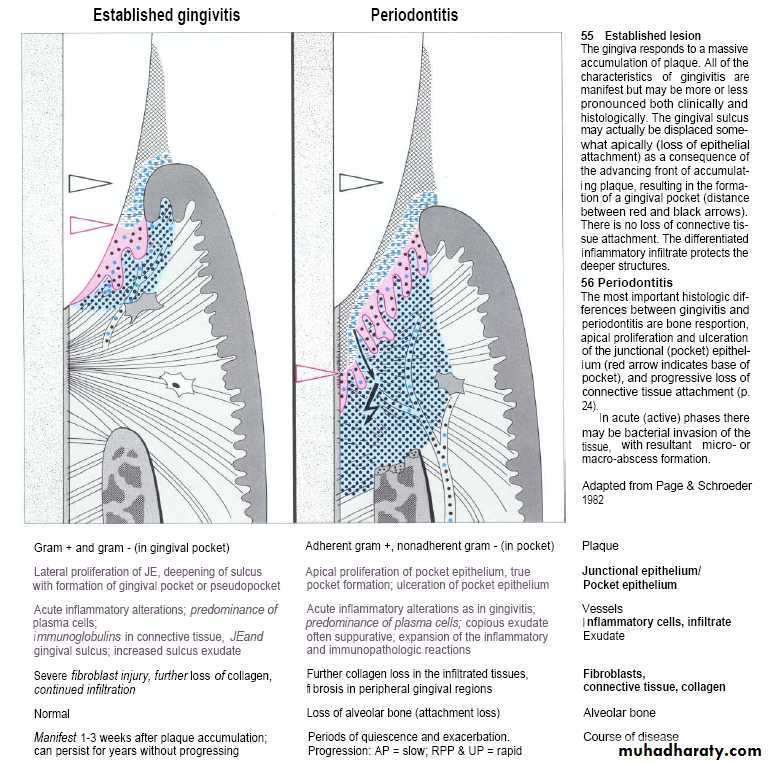
Established gingival lesionAmount of gingival fluid &increase in no.of migrating lymphocytes.
After 1months,celluar & permeability response appear( reach to steady or balance state).
Neither rapid extension of inflammation nor microorganisms elimination.
Large no.of plasma cells in coronal connective tissue & around vessels(primary characteristic feature).
Collagene lost due to collagenase produce by microorganisms & polymorphnuclear leukocytes.
Proliforation of junctional epithlium maintained with the formation of pocket epithelium which are thin & ulcerated with wide intercellular space.
Disease progression
Established gingival lesionBlood vessels become congested, venous return impaired & blood flow becomes sluggish.
Localized gingival anoxemia which superimposes the bluish color on reddened gingiva.
Extravasations of RBC into connective tissue & breakdown of hemoglobin can deepen the color of chronically inflamed gingiva.
Lesion can describe as moderately to severely inflamed gingiva.
Disease progression
Advanced gingival periodontal lesionGrow of plaque along crown & cementum.
Deepening of pocket with continuo proliferation of junctional epithelium. & infiltration of plasma & other cells
Further destruction of collagen fibers.
Alveolar bone destruction “indicate transition from gingivitis to periodontitis”