Laryngeal Trauma
Dr. Nada Khalil Yaseen
Introduction
Incidence: 1:30,000 emergency patients
Airway
Voice
Outcome determined by initial
management
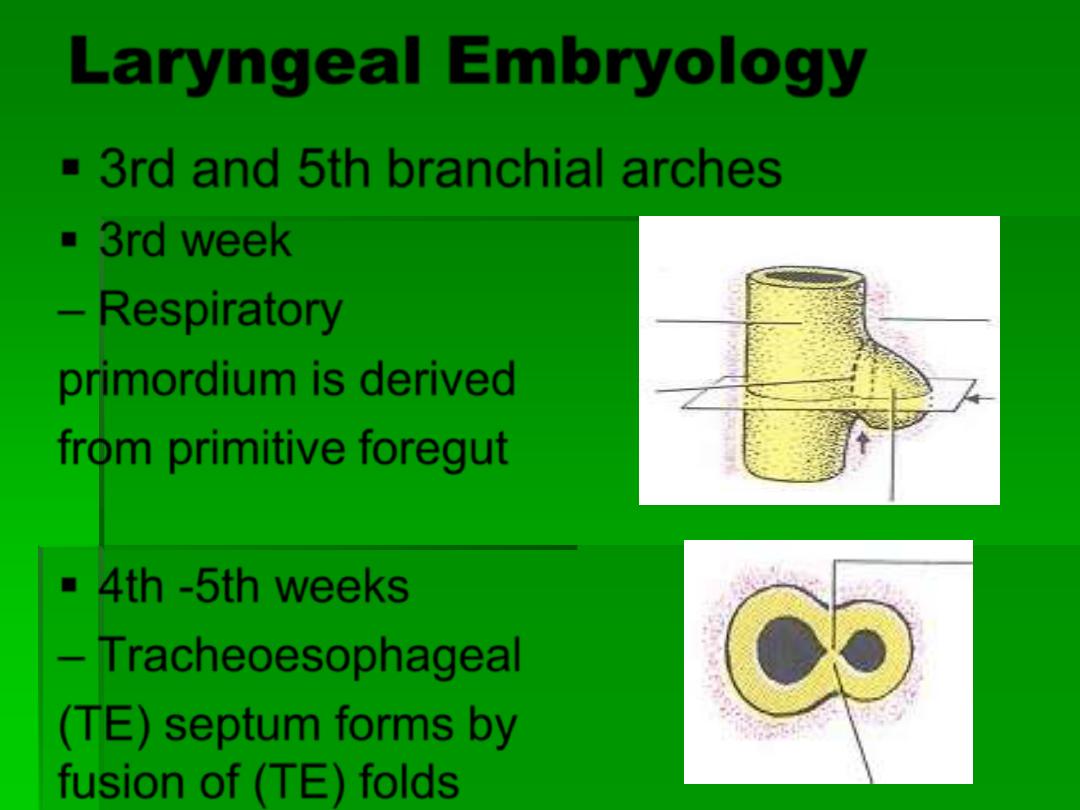
Laryngeal Embryology
3rd and 5th branchial arches
3rd week
– Respiratory
primordium is derived
from primitive foregut
4th -5th weeks
– Tracheoesophageal
(TE) septum forms by
fusion of (TE) folds
Anatomy and Physiology
of Larynx
Well protected (mandible, sternum, neck
flex)
Support: Hyoid, thyroid, cricoid
Innervation: RLN, SLN
Supraglottis: soft tissue
Glottis: relies on external support, crico-
arytenoid mobility and neuromuscular input
Subglottis: cricoid, narrowest in infants
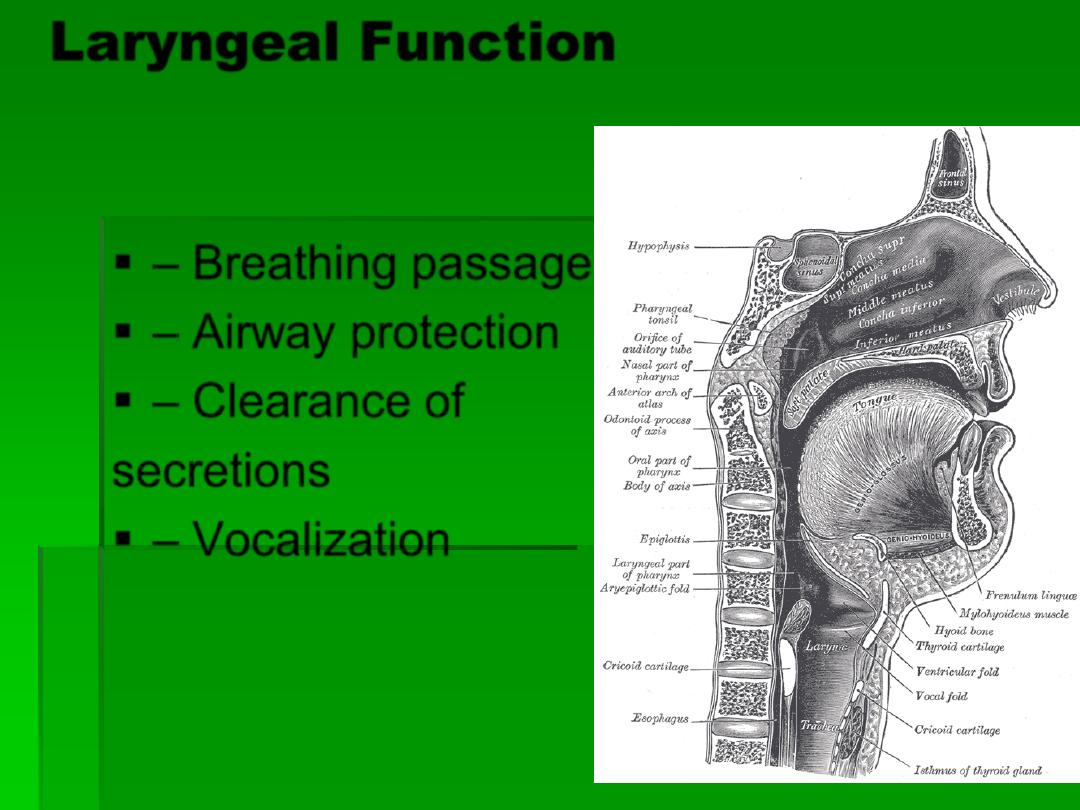
Laryngeal Function
–
Breathing passage
– Airway protection
– Clearance of
secretions
– Vocalization

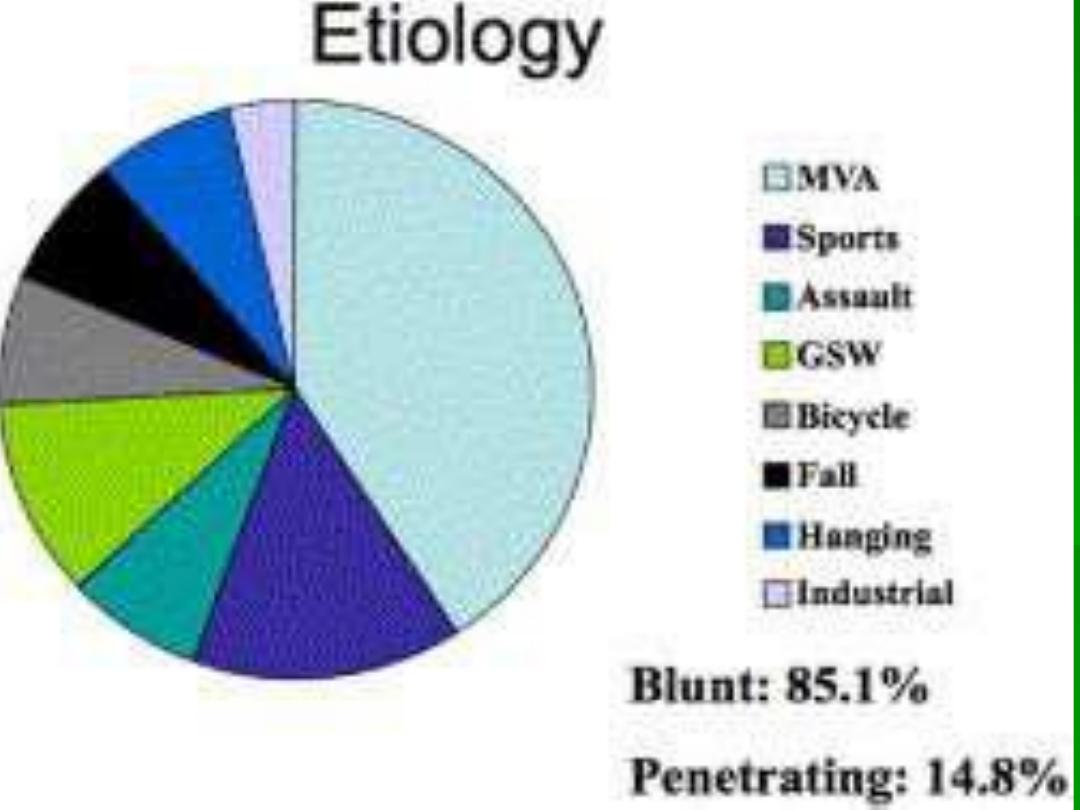
Mechanism of Injury
Blunt
–
motor vehicle accident , strangulation,
clothesline, sports related
Significant internal damage, minimal
external signs
Penetrating
Gun shot wound: damage related to
velocity
Knife: easy to underestimate damage

• Penetrating trauma
–
GSW- related to the
type of weapon
Directly penetration or
indirectly by the blast
effect
Blunt Trauma: Mechanisms
of Injury
Compression over
spine
Static lateral force
Laryngo-Tracheal
separation

Blunt injuries
– Most commonly
from
MVA
– Forward thrust
• Neck extension
•
impacting steering
wheel
• Removes the
mandibular barrier

Laryngeal skeleton is
compressed between a
foreign object (i.e.,
steering wheel or
dashboard) and the
anterior aspect of the
cervical spine
Decrease incidence- seat
belt harness and air bags
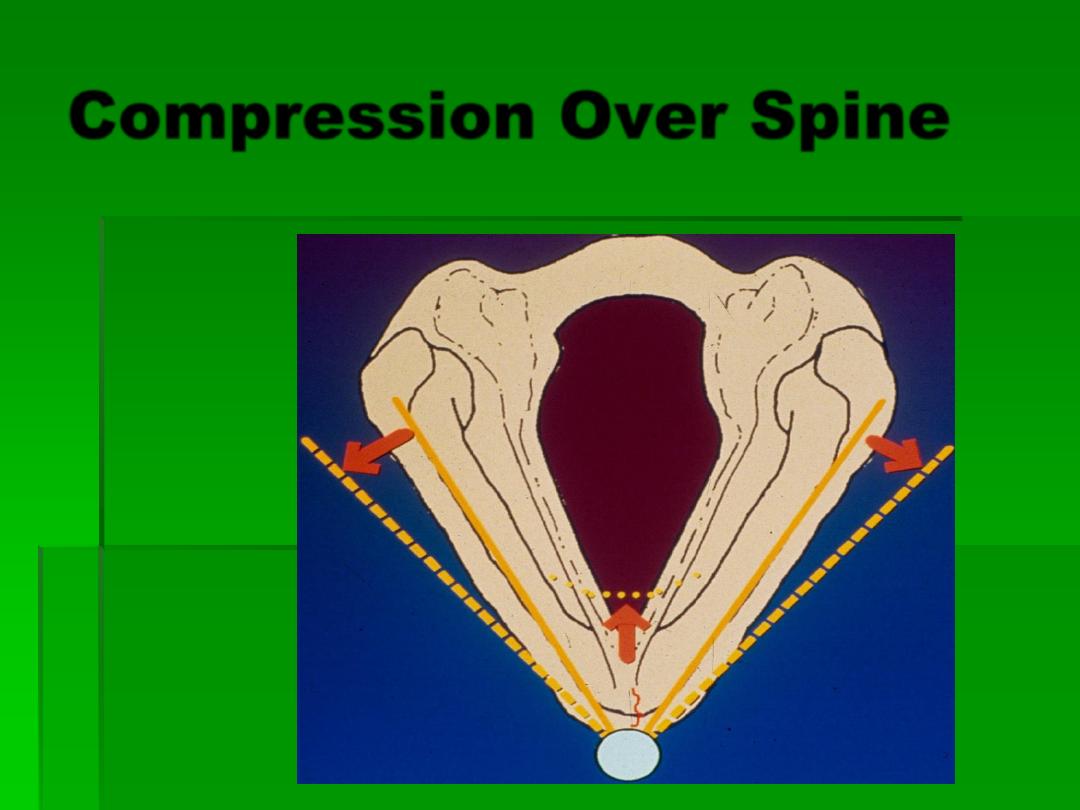
Compression Over Spine
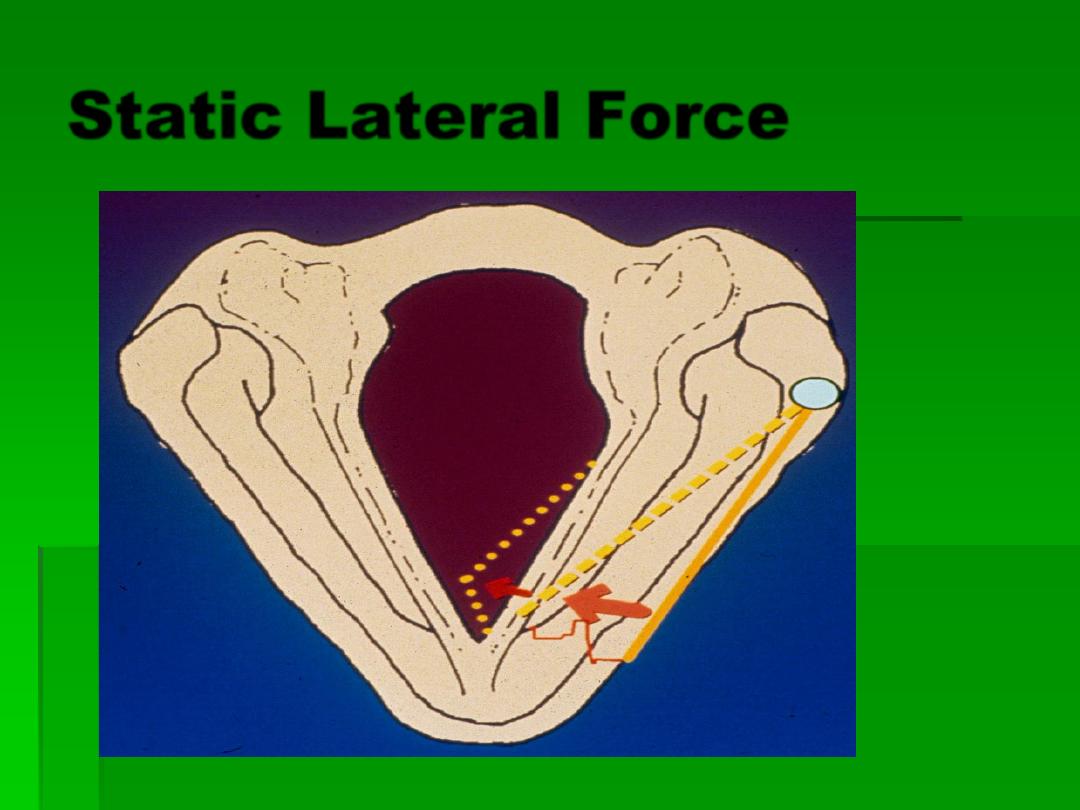
Static Lateral Force
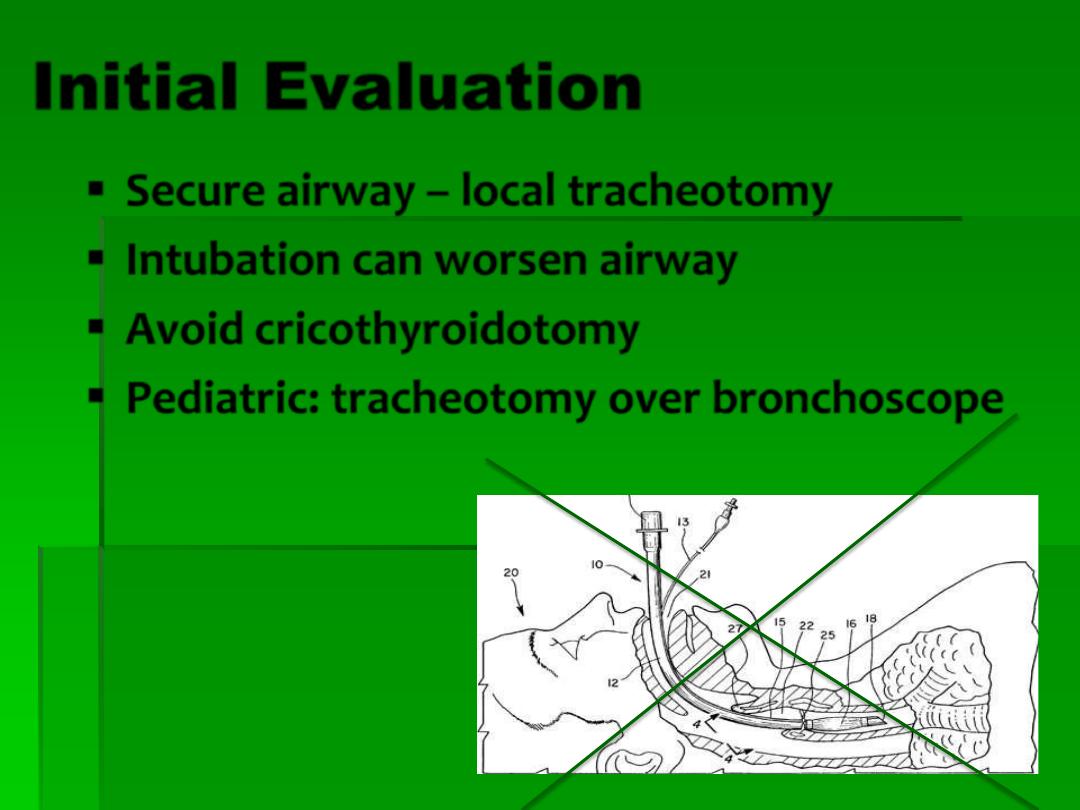
Initial Evaluation
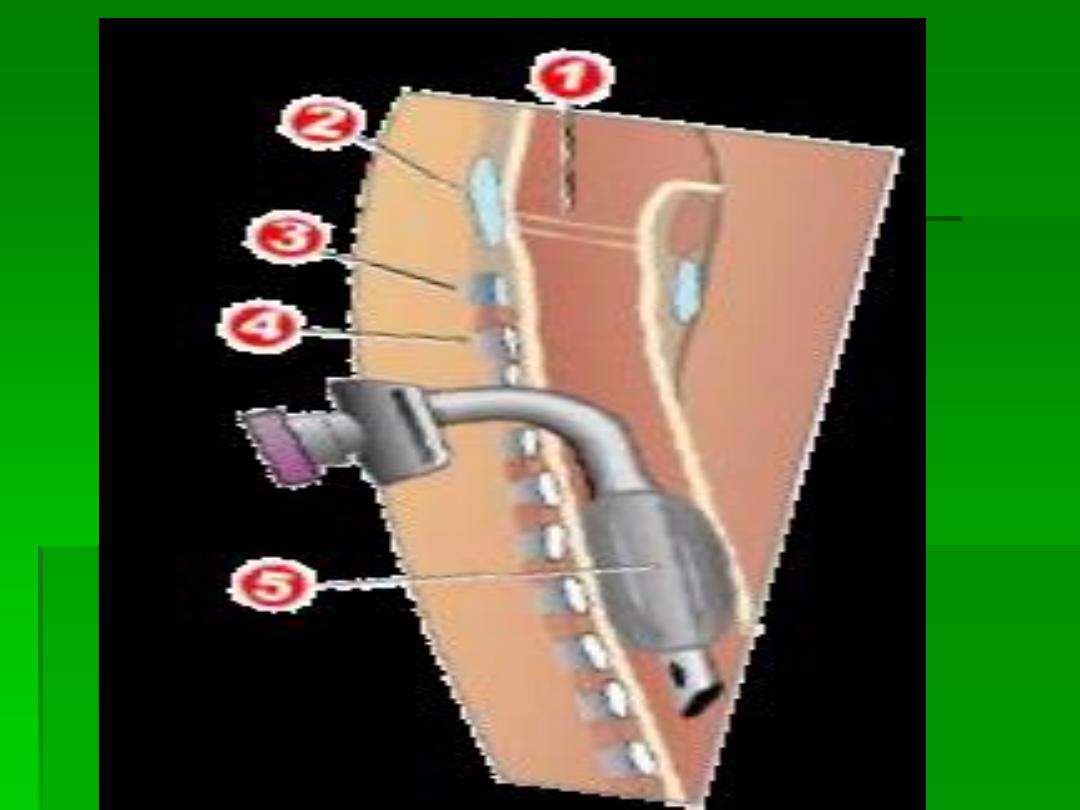
Secure airway – local tracheotomy
Intubation can worsen airway
Avoid cricothyroidotomy
Pediatric: tracheotomy over bronchoscope
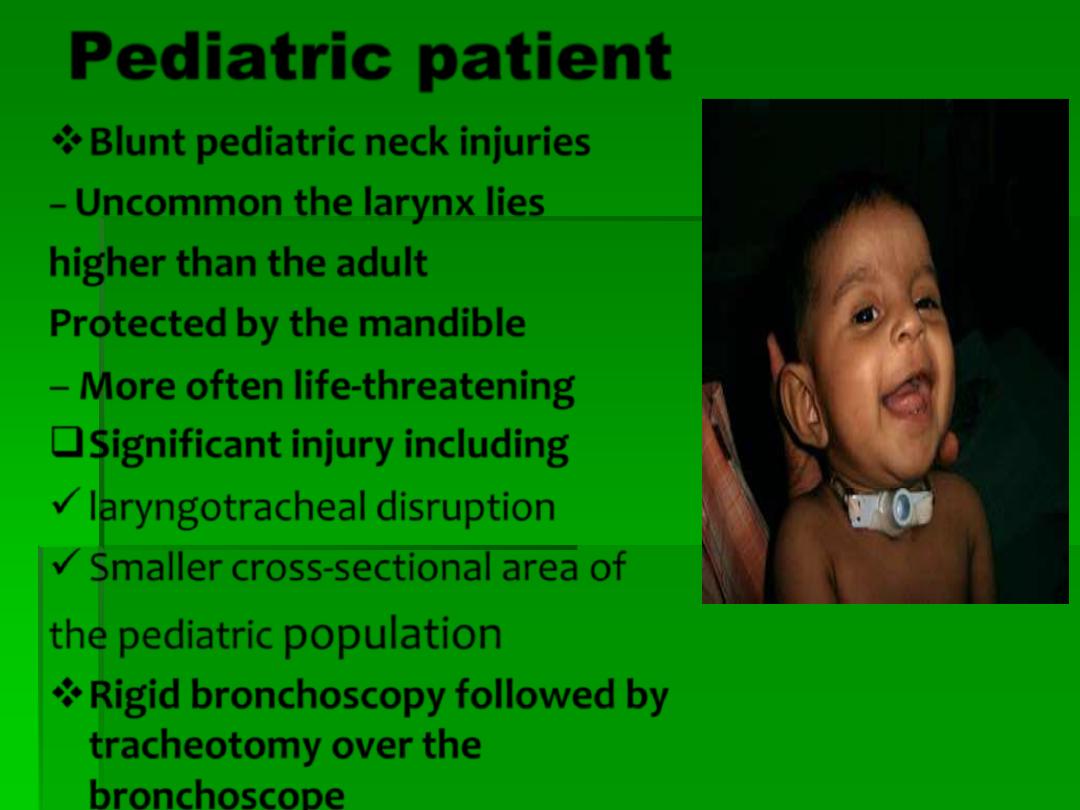
Pediatric patient
Blunt pediatric neck injuries
–
Uncommon the larynx lies
higher than the adult
Protected by the mandible
–
More often life-threatening
Significant injury including
laryngotracheal disruption
Smaller cross-sectional area of
the pediatric
population
Rigid bronchoscopy followed by
tracheotomy over the
bronchoscope
History
Change in voice
– most reliable
Dysphagia
Odynophagia
Difficulty breathing - more severe
injury
Anterior neck pain
Inability to tolerate supine position
–
probable airway compromise
imminent
Physical exam
Stridor
Hoarseness
Subcutaneous emphysema
Hemoptysis
Laryngeal tenderness, ecchymosis, edema
Loss of thyroid cartilage prominence
Associated injuries - vascular, cervical spine,
esophageal
Flexible Fiberoptic
Laryngoscopy
Perform in emergency room
Findings dictate next step
CT scan
Tracheotomy
Endoscopic
Surgical Exploration
Other studies
Radiographic Imaging
C-spine
CT if airway stable and mild abnormality
on flexible exam.
Good for intermediate cases with scope
limited by edema
Angiography and contrast esophagrams
considered
CT Scan
Indications
:
Significant mechanism of
injury
Rule out occult
fracture/dislocation
Confirmation of
suspected fracture
Determine extent of
fracture(s
)
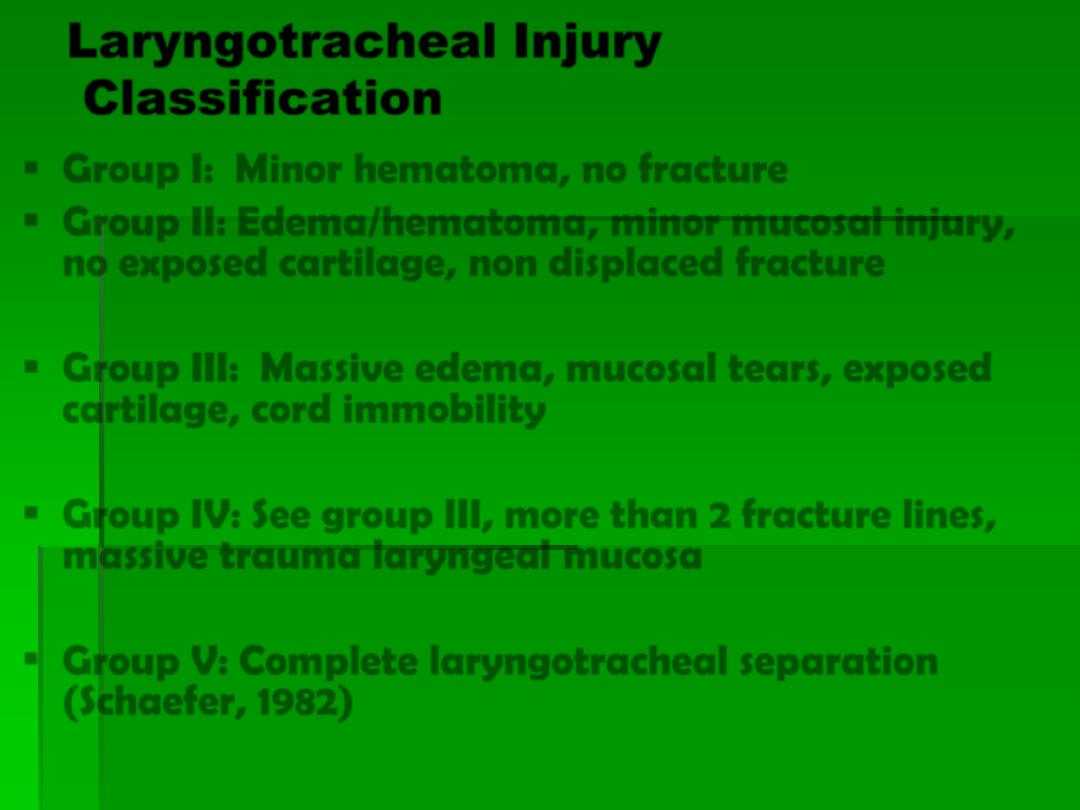
Laryngotracheal Injury
Classification
Group I: Minor hematoma, no fracture
Group II: Edema/hematoma, minor mucosal injury,
no exposed cartilage, non displaced fracture
Group III: Massive edema, mucosal tears, exposed
cartilage, cord immobility
Group IV: See group III, more than 2 fracture lines,
massive trauma laryngeal mucosa
Group V: Complete laryngotracheal separation
(Schaefer, 1982)
Laryngeal Trauma
Asymptomatic or minimal symptoms
F/L
CT scan
Mild Edema
Small hematoma
Non-displaced linear fracture
Intact mucosa
Small lacerations
Displaced fracture
(by CT or exam)
Loss of mucosa or extensive
laceration
Bleeding
Exposed cartilage
Bed rest
Cool mist
Antibiotics
Steroids
Anti-reflux
Tracheotomy
Panendoscopy
Explore
Laryngeal Trauma
Respiratory distress, open wounds, bleeding
Tracheotomy
Panendoscopy
Explore
Medical Management
Group I injuries
– Minimum of 24 hours
of close observation
– Head of bed elevation
– Voice rest
– Humidified air
– Anti-reflux medication
– Serial flexible fiberoptic exams
Antibiotics for laryngeal mucosa
disruption
Steroid
Controversial
Early systemic steroids therapy are often given
to reduce laryngeal edema
Indications for Repair
(surgical treatment)
Comminuted fractures
Displaced fractures
All fractures involving
the median and
paramedian thyroid
ala
Cricoid fracture
LT separation
Large mucosal
lacerations
Laceration of AC and
free edge VC
Disruption CA joint
VC immobility
Exposed cartilage
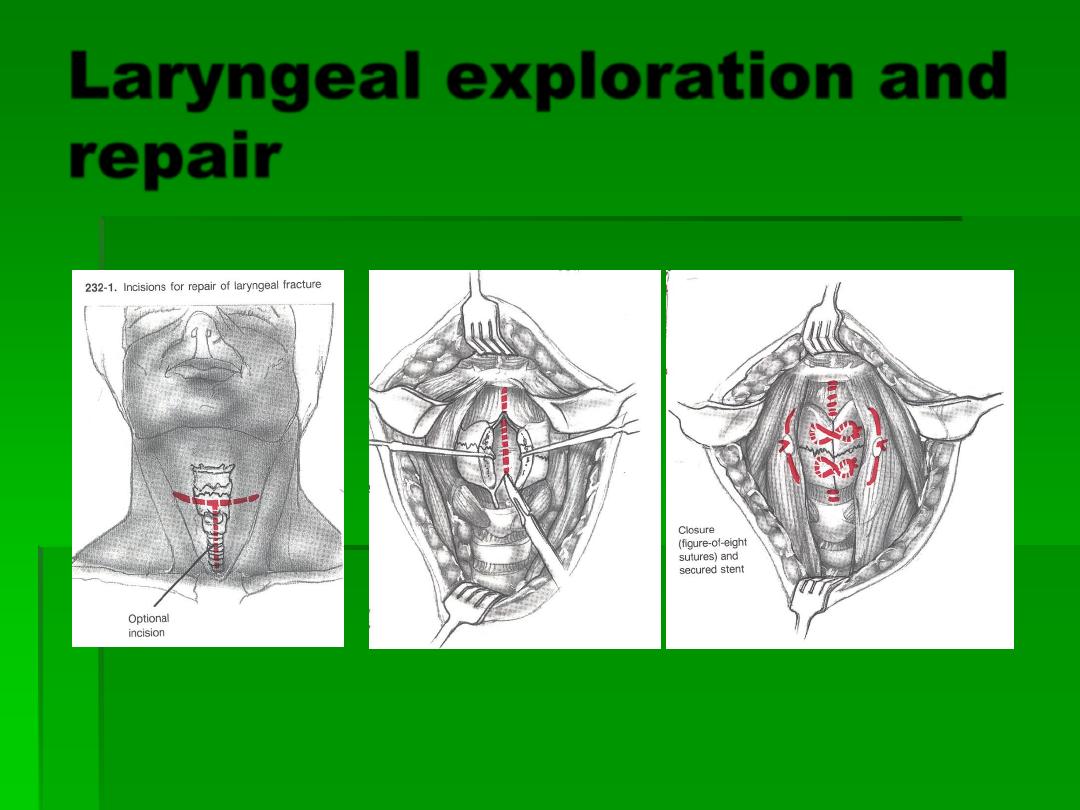
Laryngeal exploration and
repair
Goals of Laryngeal
exploration
Cover all cartilage to prevent granulation
tissue and fibrosis
Primary closure ideal,can undermine
mucosa or use advancement flaps from
epiglottis or pyriforms
Palpate arytenoids and reposition if
necessary
Resuspend anterior commisure.
Treatment Goals
Preservation of airway
Prevention of aspiration
Restoration of normal voice
Outcomes
Airway
Poor
– trach dependent
Fair
– mild aspiration or exercise
intolerance
Good
– preinjury status
Outcomes
Voice
Poor: aphonia or whisper
Fair: changed or hoarse
Good
– normal voice
Outcomes
Swallowing
Normal
Abnormal
Subjective patient report
Outcomes
Medical better than surgical
Voice results worse with use of stents
(airway the same), less time in better
Vocal cord paralysis – poorer outcome
Improved results with repair <48 hours
Conclusions
Rare injury
Assess airway first and follow systematic
management
Timely evaluation with high index of suspicion for
classic signs and symptoms
Don’t forget about associated vascular or
esophageal injuries
Treatment based on site/extent of injury
