Objectives
• To know the clinical features and management of newborn baby with transient tachypnea of newborn baby and meconium aspiration syndrome• To recognize the clinical features of congenital diaphragmatic hernia and tracheoesophageal fistula
• To know the features of other complications of preterm baby like intraventricular hemorrhage, apnea, and necrotizing enterocolitis
Transient Tachypnea of Newborn [TTN ]TTN is self limited condition characterized by tachypnea,mild retraction, and occasional grunting,usually with out signs of severe respiratory distress. Cyanosis when present, usually requires no more than 40% O2.Patients usually recover rapidly within 3 days. The lungs are generally clear without rales or rhonchi .
TTN is noted in large premature infants& term infants born by cesserian section with out prior labour.
Infants of diabetic mothers and infants with poor respiratory drive as a result of placental passage of analgesic drugs are at risk.
TTN may be caused by retained lung fluid or slow resorption of lung fluid.
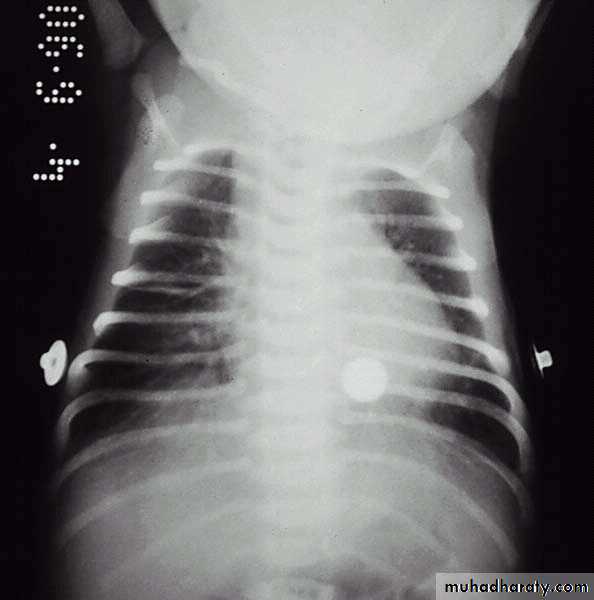
Chest x-ray:Prominent central vascular marking, fluid in lung fissure, overaereation, occasionaly small pleural effusion.
Distinguishing the disease from RDS and other respiratory disorders (e.g., pneumonia) may be difficult, and transient tachypnea is frequently a diagnosis of exclusion;
the distinctive features of transient tachypnea are rapid recovery of the infant and the absence of radiographic findings for RDS (hypoaeration, diffuse reticulogranular pattern, air bronchograms) and other lung disorders.
TTN. Radiograph reveals a number of streaky perihilar densities and a visible fluid density in the right major fissure.
Meconium Aspiration SyndromeMeconium is the first intestinal discharge from newborns which is a viscous, dark green substance composed of intestinal epithelial cells, lanugo, mucus, and intestinal secretions, such as bile. Meconium stained amniotic fluid is seen in 15% of predominantly term, growth retarded,& post term deliveries. Although the passage of meconium into amniotic fluid is common in infants born in the breech presentation, meconium-stained fluid should be considered a sign of fetal distress& suggest in utero asphyxia, hypoxia, acidosis. Meconium inactivates surfactant . Meconium aspiration syndrome develops in 5% infants with meconium stained amniotic fluid.
Meconium. A typical, sticky, greenish-black meconium stool
consists of accumulated intestinal cells, bile, andproteinaceous material formed during intestinal development
Meconium may be aspirated before, during, or just after birth leading to high incidence of pneumonia& pneumothoraces. Clinical features: Meconium aspiration pneumonia characterized by tachypnea, hypoxia, hypercapnia,& small airway obstruction that produce air trapping,& extra-alveolar leaks. Complete small airway obstruction produces atelectasis within 24-48 hr, chemical pneumonitis develops in addition mechanical effect of airway obstruction.
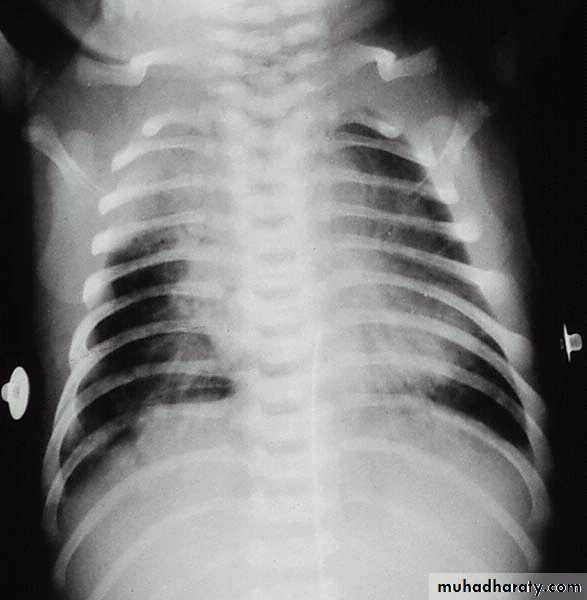
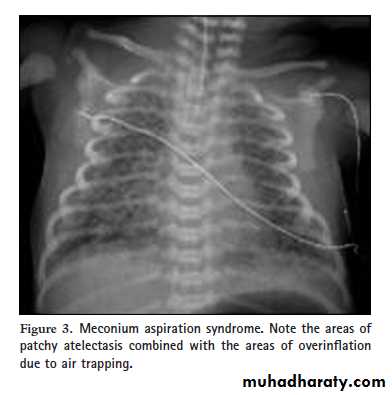
Chest x-ray:- Patchy infiltrates, overdistention , flattening of diaphragm, increase anteroposterior diameter& high incidence of pneumomediastinum& pneumothorax.
Meconium aspiration. The radiograph reveals irregularly distributed areas of hyperaeration and consolidation.
Prevention The risk of meconium aspiration may be decreased by rapid identification of fetal distress and initiating prompt delivery in the presence of fetal acidosis, late decelerations, or poor beat-to-beat variability.
Treatment
Routine intubation to aspirate the lungs of vigorous and depressed infants born through meconium-stained fluid is not recommended.Treatment of meconium aspiration pneumonia includes supportive care and standard management for respiratory distress.
Administration of exogenous surfactant to infants with MAS requiring mechanical ventilation decreases the need for ECMO support
Treatment with antibiotics should also be strongly considered because intrauterine infection might be a precipitating factor in the initial passage of meconium and that in vitro studies suggest that the presence of meconium might facilitate the growth of bacteria in the lung.
Both conventional and high-frequency ventilation can be used to achieve normal gaseous exchange and prevent complications such as air trapping and air leaks, which are common in such infants.
Inhaled nitric oxide (iNO) therapy should be considered in infants with concomitant PPHN who are not responding to
conventional treatment.
Extracorporeal membrane oxygenation (ECMO) is considered as a rescue treatment when predicted mortality is running
high.
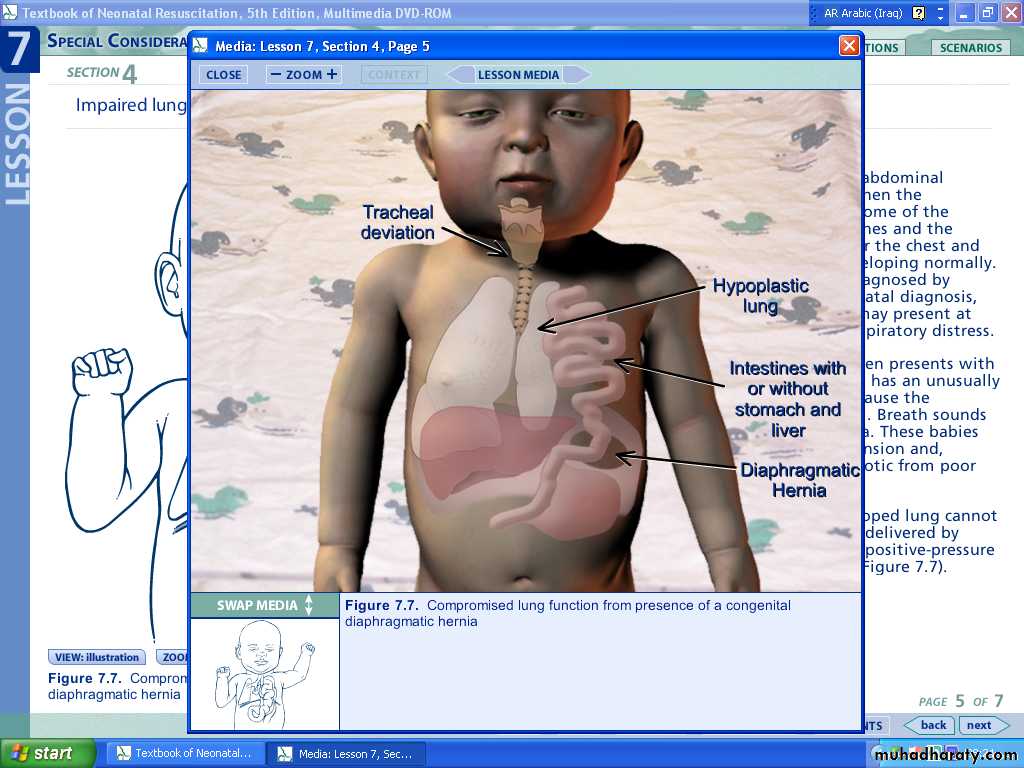
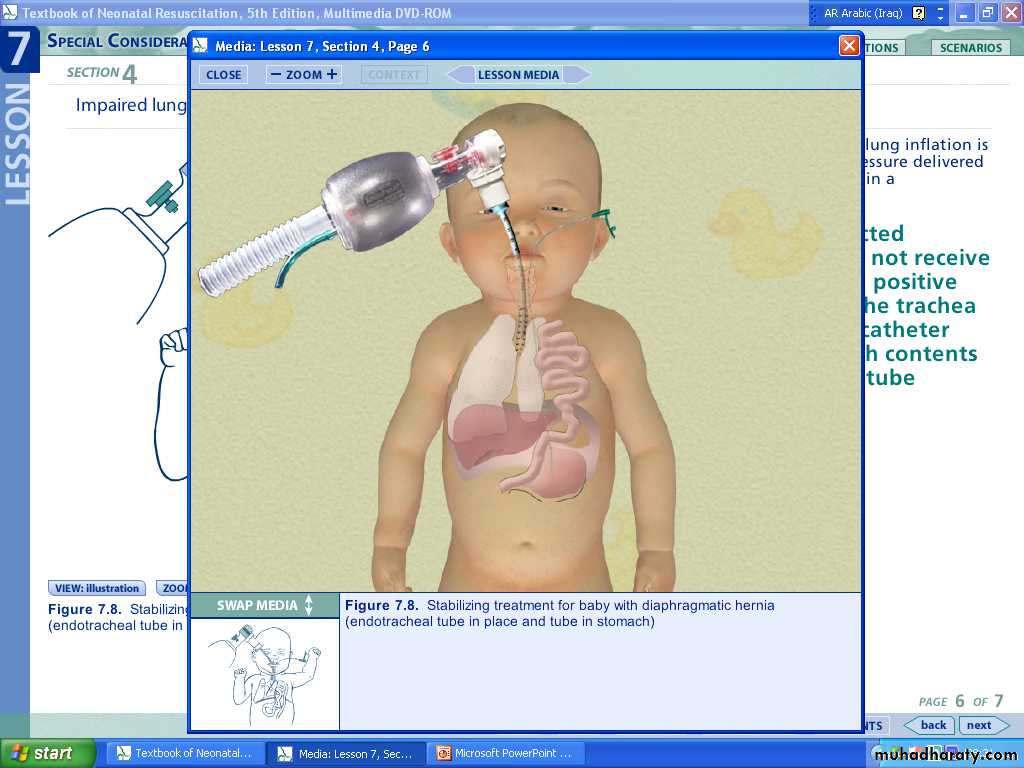
Congenital Diaphragmatic HerniaEtiology:Herniation occurs most often in posterolateral segment of diaphragm more often in left side due to failure of pleuroperitoneal canal to close[foramen of Bochdalek].Less frequently the herniation in the retro sternal area[foramen of Morgagni].The vast majority, 90%–95%, are of the Bochdalek type.As many as 30%–40% of babies with CDH have additionalcongenital anomalies, most commonly of the heart, central nervous system, and genitourinary system.
Pathology:
Protrusion of abdominal viscera [stomach,intestine,spleen …] through diaphragmatic hernia in to thoracic cavity displace the lungs and heart to opposite side.
The lung on affected side is compressed and hypoplastic,this lead to increase pulmonary vascular resistance and pulmonary hypertension.
Clinical Manifestations:Severe respiratory distress,including dysopnea and cyanosis is frequently present at birth or later.The abdomen is usually small and scaphoid.The infant is cyanotic and have respiratory retraction.Breath sounds may be absent on the affected side,and occasionally sounds of intestinal peristalitic movement can be heard over the chest.Diagnosis: by x-ray.Antenatal diagnosis may be made by ultrasound.
This is a radiograph of a 1-day-old infant with a moderate-sized
congenital diaphragmatic hernia. Note the air- and fluid-filled bowel loopsin the left chest, the moderate shift of the mediastinum into the right chest,
Treatment:
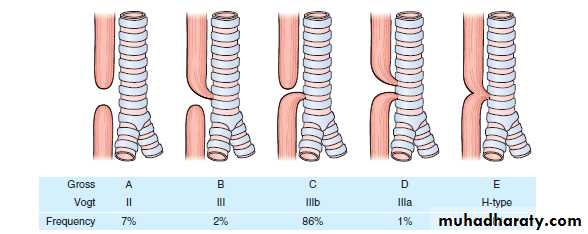
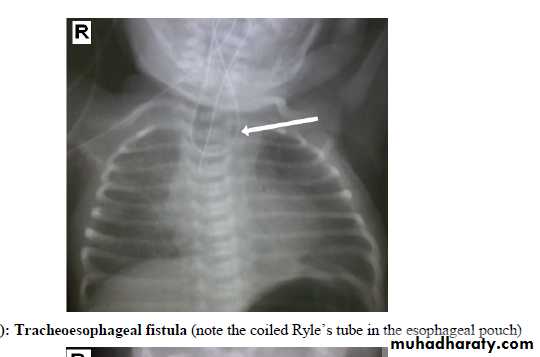
Resuscitation of newborn is mandatory prior to surgery1-position head and thorax higher than abdomen to facilitate downward displacment of abdominal organs.2-nasogastric intubation with intermittent suction decrease air and fluid in herniated viscera.Esophageal Atresia&Tracheoesophageal FistulaIn 85% of cases fistula between trachea and distal esophagus accompanies atresia. Less commonly, EA or TEF may occur alone.One third of affected infants are born premature.
Clinical manifestations:
Atresia of esophagus should be suspected:1-In cases of maternal polyhydromnias.2-If catheter used at birth for resuscitation cannot be inserted in to the stomach.3-If infant has excessive oral secreations.4-If choking, cyanosis,or coughing occurs with an attempt of feeding.In infant with fistula with out atresia [H type] the usual sign is recurrent aspiration pneumonia.At least 30% of infant with EA have associated congenital anomalies like VATER anomalad.Diagnosis:Inability to pass catheter in to the stomach confirms the suspicion,and x-ray shows coiled catheter in to upper esophageal pouch.Treatment: by surgery.
Isolated esophageal atresia (EA). . Note the absence of bowel gas in this patient with EA
,
Periventricular Hemorrhage [PVH]& Intraventricular Hemorrhage[IVH]Are common among VLBW ,and the risk decrease with increasing gestational age.50% of infants under 1500gm have evidence of intracranial hemorrhage.
Pathogenesis: unknownInitial site of bleeding may be the weak blood vessels in the periventricular germinal matrix. These vessels in this area have poor structural support.Main risk factor is passive changes in cerebral flow with variation of blood pressure.Factor effect blood pressure or interfere with venous return from head increase risk of IVH includes: asphyxia, pneumothorax, mechanical ventilation, hypercapnia, hypoxemia, prolonged labor, breach delivery, PDA, heart failure, I.V.therapy with albumin& hypertonic solution such as sodium bicarbonate.
Clinical manifestations:Most PVH&IVH occur in the first 3 days of life, it is unusual after 5th day of life.Seizure, apnea, bradycardia, lethargy,coma,hypotension, metabolic acidosis, anemia not corrected by blood transfusion,bulging anterior fontanel,& cutanous mottling.Small hemorrhage are asymptomatic, large hemorrhage may progress to shock &death.Later complications includes posthemorrhagic hydrocephalus, periventricular leukomalacia, which may be precursor to cerebral palsy..
Diagnosis:By CT scan or ultrasound through anterior fontanel Treatment: of acute hemorrhageStandard supportive care including ventilation for apnea, and blood transfusion for shock.Post hemorrhagic hydrocephalus may be managed by serial lumbar puncture, external ventriculostomy tube or permanent ventricular peritoneal shunt.
ApneaApnea is defined as the cessation of pulmonary air flow for a specific time interval, usually longer than 10-20 seconds. Bradycardia often accompanies prolonged apnea.Types:1-Central apnea: refers to complete cessation of airflow and respiratory efforts with no chest wall movement.2-Obstructive apnea: no airflow is exhibited but the chest wall movements continue.3-Mixed apnea: a combination of these two events and is most frequent type.
Pathogenesis:-Idiopathic apnea: a disease of premature infants appears in the absence of any other identifiable disease,it occurs during the first week of life and resolve by 36 weeks of post-conceptional age. It is usually due to process of regulating respiration.Premature infants respond paradoxically to hypoxia by apnea rather than by increasing respiration as mature infant.
Causes of apnoea
Apnoea of prematurity.Lung disease (e.g. RDS, pneumothorax).
Infection.
Airway obstruction (e.g. secretions, micrognathia, choanal atresia).
Hypoxia.
Intracranial haemorrhage.
Metabolic causes (acidosis, hypoglycaemia, hypocalcaemia, hypomagnesaemia).
Drugs (e.g. maternal narcotics,), prostin (PGE1), magnesium sulphate).
Gastro-oesophageal reflux.
Seizures.
NEC.
Patent ductus arteriosus.
Temperature instability.
Polycythaemia with hyperviscosity syndrome.
CNS abnormalities
Useful investigations in determining the underlying cause of apnoea.
Full blood count.
Blood culture.
Chest radiography.
Blood glucose.
Serum electrolytes, including calcium, magnesium and sodium.
Blood gas (arterial, venous or capillary).
Continuous monitoring of oxygen saturation.
Ultrasound examination of the brain.
Treatment of apnea of prematurity:1-Adminstration of oxygen to hypoxic infants.2-Transfusion of anemic infants.3-Cutanous stimulation for infants with mild apnea.4-Persistent apnea with bradycardia can be treated with methylxanthine[ caffeine or theophylline]. Xanthine therapy increases minute ventilation, improves the carbon dioxide sensitivity, decreases hypoxic depression of breathing, enhances diaphragmatic activity, and decreases periodic breathing.5-Nasal CPAP of 3-5 cm H2O is effective method of treating obstructive or mixed apnea.
Neonate on Nasal CPAP through nasal prongs
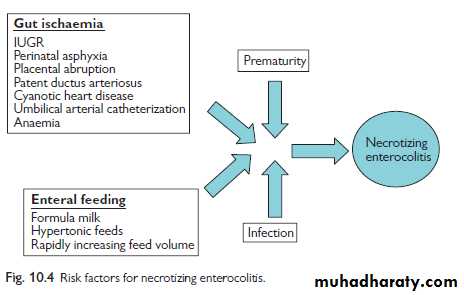
Necrotizing EnterocolitisNEC is a syndrome of intestinal injury
NEC occurs in 1-3 per 1,000 live births Prematurity is the most onsistent and significant factor associated with neonatal NEC.
The disease occurs in 4-13% of infants who weigh less than 1,500 g at birth.
NEC is infrequent in term infants (<10% of affected infants).
Pathogenesis
Prematurity is associated with immaturity of the gastrointestinal tract, including decreased integrity of the intestinal mucosal barrier, depressed mucosal enzymes, suppressed gastrointestinal hormones, suppressed intestinal host defense system, decreased coordination of intestinal motility, and differences in blood flow autoregulation, which is thought to play a significant role in the pathogenesis of NEC.Undigested milk acts as a substrate for gas- and toxin- producing bacteria and the preterm gut is more permeable to micro- organisms and relatively deficient in immunoglobulins.
Breast milk is partly protective. Probiotics have been shown to significantly decrease the incidence of NEC
in preterm infants as well as significantly decreasing all-cause mortality.
Clinical features
The onset of symptom is usually in the first week of life.Early clinical signs of NEC include abdominal distention, feeding intolerance/increased gastric residuals, emesis, rectal bleeding, and occasional diarrhea.
As the disease progresses, patients may develop marked abdominal distention, bilious emesis, ascites, abdominal wall erythema, lethargy, temperature instability, increased episodes of apnea/bradycardia, disseminated intravascular coagulation, and shock.
With abdominal perforation, the abdomen may develop a bluish discoloration.
Diagnosis:-Complete blood count.-Blood culture.-Plain abdominal x-ray: initially shows separation of bowel loops due to ascitis& fluid levels. Periluminal tramlines indicating intramural gas [pneumatosis intestinalis]. Later signs include gas in the portal tree& gas under the diaphragm following perforation.The differential diagnosis of NEC includes sepsis withintestinal ileus or a volvulus. Both conditions can present with systemic signs of sepsis and abdominal distention.
Necrotizing enterocolitis, shows pneumatosis intestinalis
Management:
Initially medical & conservative.Oral feeding should be stopped& nasogastric tube put.
Septic screen is performed.
Intravenous antibiotics[ampicilline,gentamicin,& metronidazole].
I.V feeding through central line for 10 days& bowel rest.
Surgery is indicated if there is perforation or failure to improve on medical therapy.