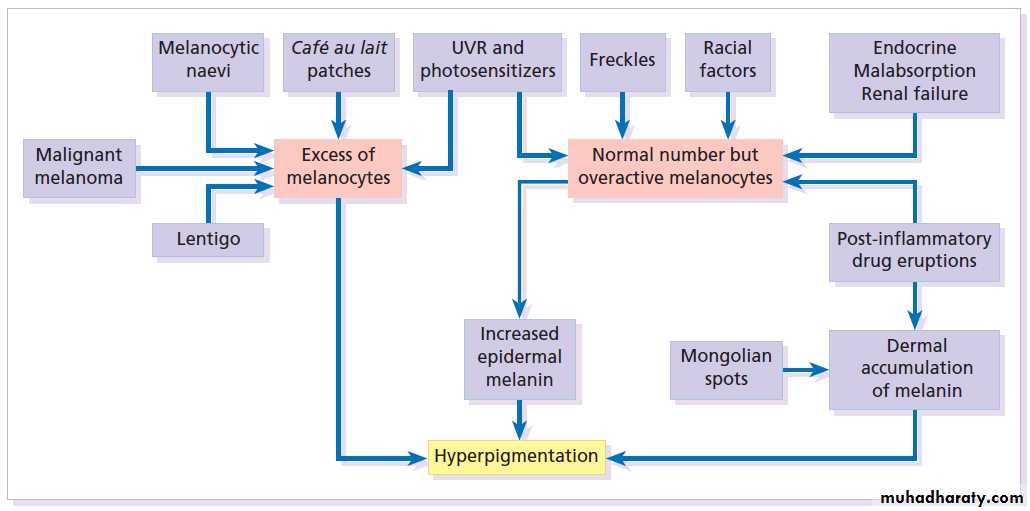
Pigmentary disorders
Dr. Qassim Al-chalabiM.B.Ch.B F.A.B.H.S
(Dermatology & Venereology)
Normal skin color
• Melanin is synthesized by epidermal melanocytes, the most important pigment in determining skin color.• Variations in the amount & distribution of melanin in the skin are the basis of the 3 racial colors: black, brown & white, which are genetically determined “constitutive melanin pigmentation”.
• Can be by UV exposure “inducible melanin pigmentation”.
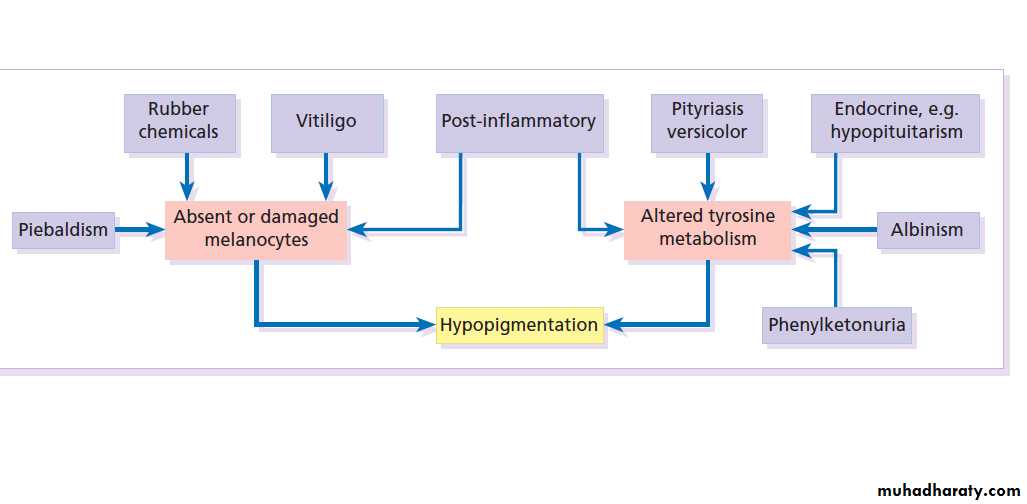
Causes of hypo and depigmentation
Vitiligoداء البهاق
• Prevelence
• A common disorder affecting about 1-2% of population.
• 50% of the patients develop vitiligo before the age of 20 & the incidence decreases with increasing age.• +ve family history in at least 30% of cases.
• Etiologic theories
• Autoimmune hypothesis.
• Melanocyte self-destructive hypothesis.
• Neural theory.
Clinical picture
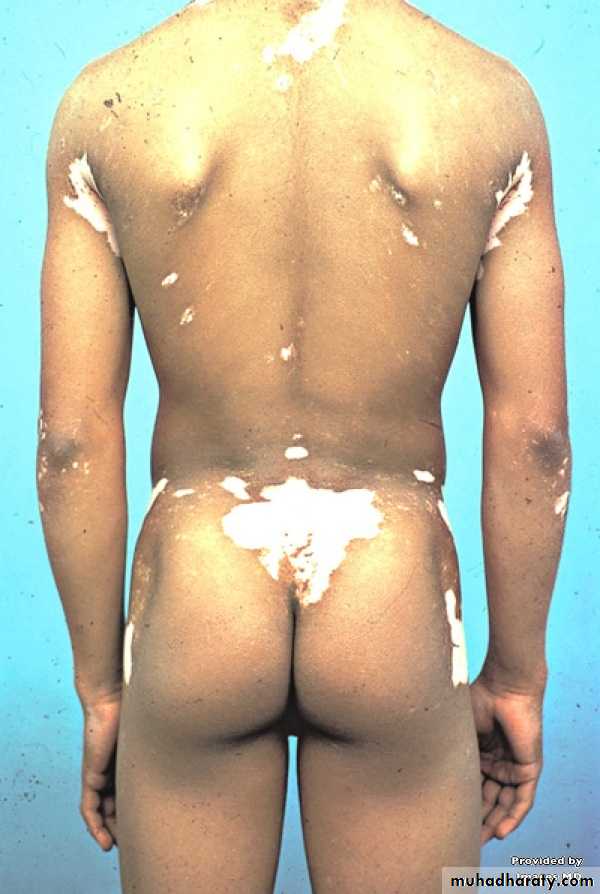
Generalized type The sharply defined, usually symmetrical, white patches are especially common on the backs of the hands, wrists, fronts of knees, neck and around body orifices. The hair of the scalp and beard may depigmented too.The course is unpredictable: lesions may remain static or spread, sometimes following minor trauma (Köbner phenomenon).
Distribution
• Focal.• Segmental (2nd common)
• Generalized: (most common)
• Acrofacial.(resistant to treatment)
• Universal vitiligo.
Associations
• Insulin-dependent diabetes
• Pernicious anemia
• Hashimoto’s thyroiditis
• Grave’s disease
• Addison’s disease
• Alopecia areata
Treatment
Sunscreen and cosmetic cover-up.Topical corticosteroids
PUVA
Ultraviolet phototherapy(NB UVB)
Laser (308 mn excimer)
Topical tacrolimus(TCI)
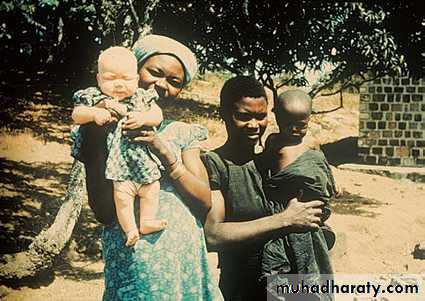
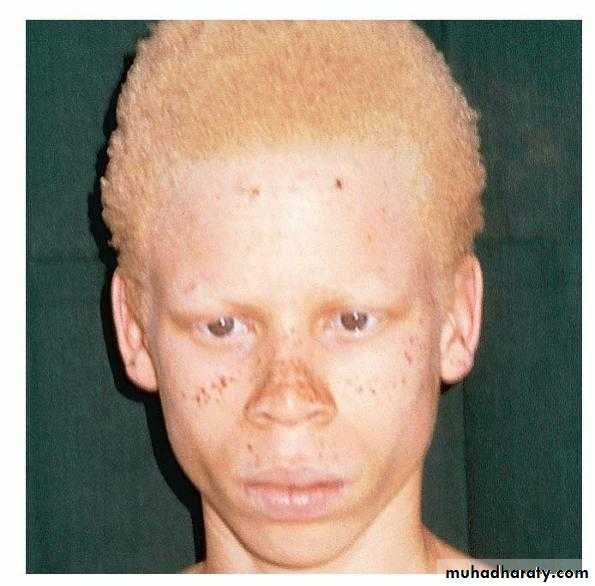
Oculocutaneous albinism
It is a genetic(AR) disorder characterized by absence of melanin in the skin and/ or eyes.The prevalence of albinism of all types ranges from 0.01% to 5% in some communities.
oculocutaneous albinism divided into two main types: tyrosinase negative and tyrosinase positive.
Clinical feature
The whole epidermis is white and pigment is also lacking in the hair, iris and retina.
Albinos have poor sight, photophobia and a rotatory nystagmus.
Tyrosinase-positive albinos may also develop freckles. Sunburn is common on unprotected skin. As melanocytes are present, albinos have non-pigmented melanocytic naevi and may develop amelanotic malignant melanomas.
Melasma
It is an acquired, symmetrical well defined hyperpigmentation their edges may be scalloped occurring on sun-exposed skin, especially the face.The condition is much more common in women, affects all races but is most prevalent in dark-skinned individuals with skin types IV–VI .
There are many causes including sunlight, pregnancy ‘the mask of pregnancy, estrogens and oral contraceptives, scented cosmetics, thyroid dysfunction and photosensitizing drugs .
Wood`s light may be useful in the determining the presence of melanin either in the epidermis or dermal.
Treatment
This is unsatisfactory.A sunscreen will make the pigmentation less obvious.
Some improvement achieved with preparations containing 2–5% hydroquinone applied for 6–10 weeks.
Chemical peels have become popular. α-Hydroxy acids, especially glycolic acid.
Melanocytic naevi
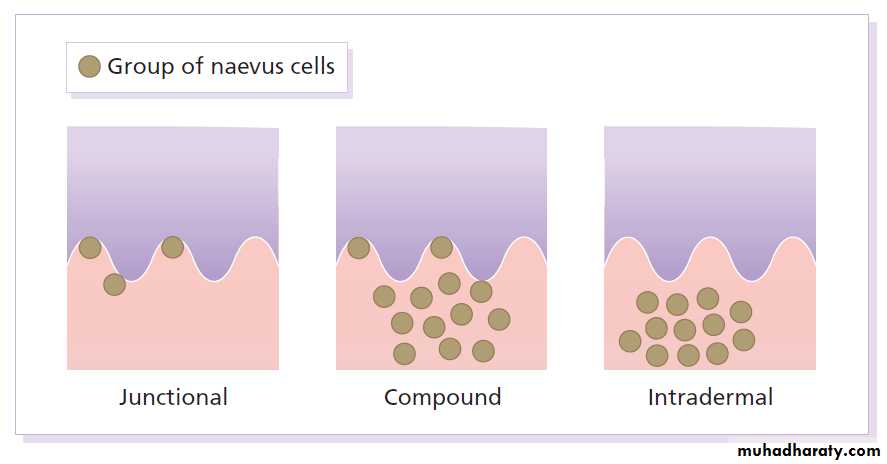
Melanocytic naevi (moles) are localized benign tumors of melanocytes. Their classification is based on the site of the aggregations of the abnormal melanocytes.Cause and evolution
The cause is unknown.A genetic factor is likely in many families, working together with excessive sun exposure during childhood.
With the exception of congenital melanocytic naevi, most appear in early childhood, often with a sharp increase in numbers during adolescence and after severe sunburns.
Further crops may appear during pregnancy, estrogen therapy.
New melanocytic naevi appear less often after the age of 20 years.
Presentation
Congenital melanocytic naevi:These are present at birth or appear in the neonatal period and are seldom less than 1 cm in diameter.
Their colour varies from brown to black or blue– black. With maturity some become protuberant and hairy, with a cerebriform surface.
Such lesions can be disfiguring (e.g. a ‘bathing trunk’ naevus).
Congenital melanocytic naevi carry an increased risk of malignant transformation, depending on their size (up to 10% in those with a diameter greater than 20 cm and less than 0.5% in those with a diameter less than 1.5 cm).
Junctional melanocytic naevi :
These are roughly circular macules. Their colour ranges from mid brown to black and may vary even within a single lesion. Most melanocytic naevi of the palms, soles, mucous membranes and genitals are of this type.
Compound melanocytic naevi :
These are domed pigmented nodules of up to 1 cm in diameter. They arise from junctional naevi. They may be light or dark brown but their colour is more even than that of junctional naevi. Most are smooth, but larger ones may be cerebriform, or even hyperkeratotic and papillomatous; many bear hairs.
Intradermal melanocytic naevi: These look like compound naevi but are less pigmented and often skin-coloured.
Blue naevi So-called because of their striking slate grey–blue colour, blue naevi usually appear in childhood and adolescence, on the limbs, buttocks and lower back. They are usually solitary.
Other rare types:
Spitz naeviDysplastic naevi(increase risk of MM)
Mongolian spots
A- Junctional melanocytic nevus.
B- compound nevus.Complications
Inflammation Pain and swelling are common but are not features of malignant transformation. They are caused by trauma, bacterial folliculitis or a foreign body reaction to hair after shaving or plucking.
Depigmented halo: So-called ‘halo naevi’ are uncommon but benign. There may be vitiligo elsewhere.
Malignant change This is extremely rare except in congenital melanocytic naevi.
Treatment
Excision is needed when:1- A naevus is unsightly;
2- Malignancy is suspected or is a known risk (e.g. in a large congenital melanocytic naevus).
3- A naevus is repeatedly inflamed or traumatized.