
Complications of fractures
Local complications
Late
Less urgent
urgent
Delayed union
Fracture blister
Visceral injury
Malunion
Plaster sore
Vascular injury
Non-union
Pressure sore
Nerve injury
Avascular necrosis
Nerve entrapment
Compartment syndrome
Muscle contracture
Myositis ossificans
Hemarthrosis
Joint instability
Ligament injury
Infection
Osteoarthritis
Tendon lesion
Gas gangrene
Joint stiffness
Algodystrophy
Bone:
Infection: usually occur in open #, but could affect
closed # following open reduction &internal fixation.
Clinically: the wound become inflamed, discharging
seropurulent fluid. Culture will reveal the organism.
Ŗ→ meticulous debridement & AB.
Stabilize the # with external fixation.
Skin:
Fracture blister: due to elevation
of superficial layers of skin by
edema especially in ankle #.
Prevention: firm bandaging.
Ŗ→ cover with sterile dressing.
Plaster sore: due to pressure of Pop cast on bony
prominence causing skin ischemia with burning
sensation which is an alarm to open a window in the cast
to relief the pressure otherwise, skin necrosis will occur.
Prevention: good padding over bony points & gentle
casting. Ŗ→ cut a window for dressing.

Muscle:
With any fracture, there will be tear in muscle fibers near the #.
These would adhere to each others, to the healing bone and to
joint capsule. Later, after healing (fibrosis), the joint become stiff.
Prevention & Ŗ→ early muscle exercise.
Joint:
Haemarthrosis:
the joint become swollen, tense & painful.
Ŗ→ the blood should be aspirated under strict aseptic
condition & joint splinted
untill the pain subsided,
then start early active
. exercise.
Vessels:
Vascular(arterial) injury:
The usual sites are fractured knee, elbow,
humerus &femur. The artery may be cut,
torn, compressed, thrombosed due to
intimal injury or only in spasm.
CF: the limb become: pale (or blue),
cold, numb (paraesthesia in fingers or toes)
with absent or weak pulse &in severe cases,
peripheral gangrene.
Ŗ→ remove all the dressing & the pop
cast, reduce the displaced # & wait for
1/2 an hour, if there is no improvement,
then explore the vessel and deal with it:
suture a tear, remove a thrombus or
replace a segment with vein graft.
Certainly, the # should be stabilized
before start repairing the vessel.
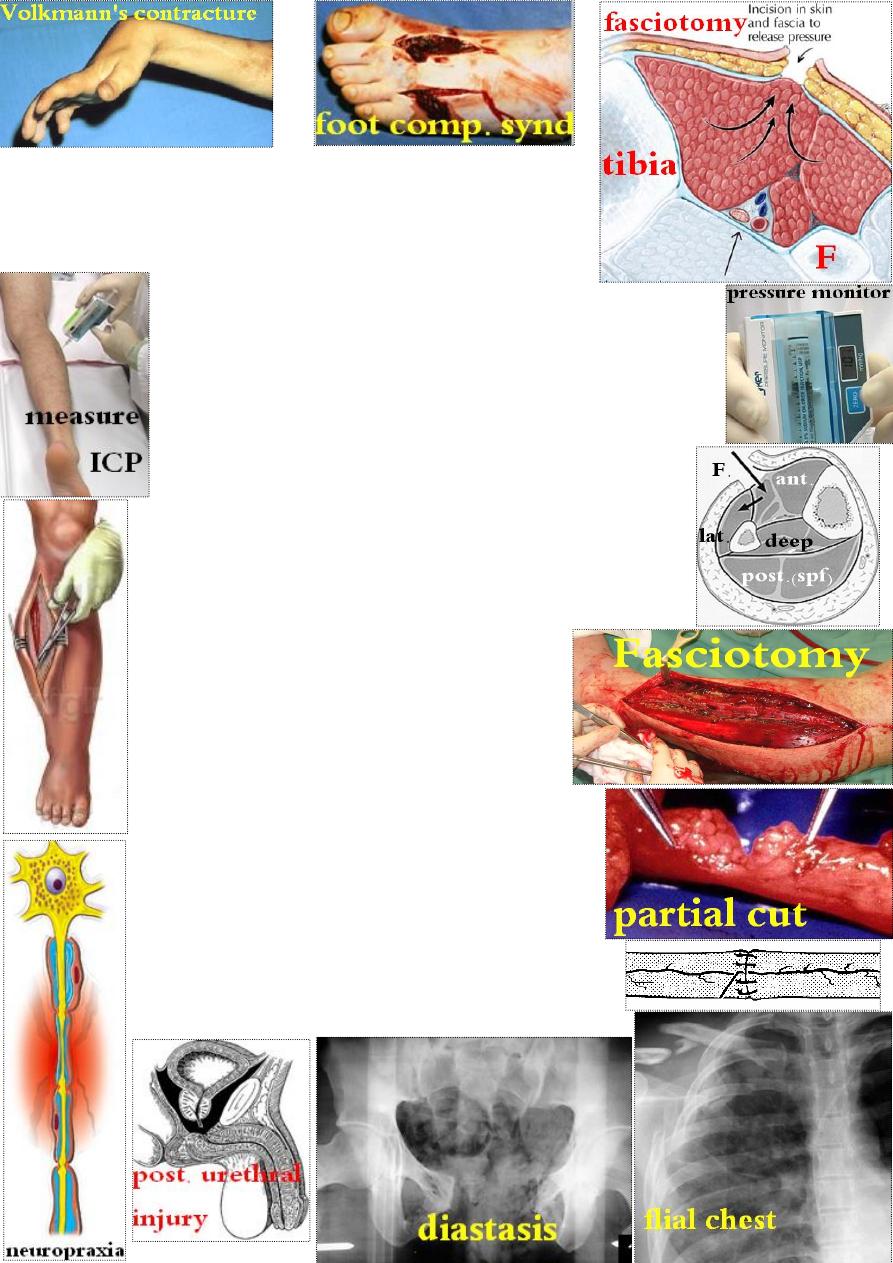
Compartment syndrome: the usual sites are
forearm and leg. The common cause is #, but
can occur following operation or infection.
Pathogenesis: bleeding or edema will ↑ the pressure
in one of the closed osteofascial compartment →
↓ capillary blood flow → muscle ischemia →
more edema → ↑ intracompartmental pressure & so on.
Results:
Muscle &nerve necrosis occur after 4-8 hrs of complete ischemia.
The muscle will be replaced by fibrous tissues causing contracture
(Volkmann's ischemic contracture) of the flexor forearm
muscles with fingers flexion. The nerves may regenerate later.
CF: early: you should suspect the condition if the limb is:
unduly painful, swollen, tense & passive fingers movement
causes pain. So measure intracompartment pressure(ICP)
which is normally 0-10 mmHg.
In late cases, there will be the 5Ps:
pain, paraesthesia, pallor, paralysis &pulselessness.
Ŗ: in mild cases: remove all dressing &splints
& wait for 1 hour, if not improved or ICP
> 30- 40 mmHg., then do fasciotomy. The wound
of fasciotomy is left open for late closure.
Ŗ→ of Volk. contracture: release of the contracted
muscles at their origin or tendon transfer.
Nerves:
In closed injury, the nerve is usually compressed &
the lesion is neuropraxia which recovers within few
days or weeks. If not, do explore &deal with the lesion.
In open injury: the nerve is usually cut (neurotmesis)
which require early repair or after 3 weeks.
Visceral injury:
like pelvic # may be associated with bladder
or urethral injury, or ribs # causing lung injury.
Late complications:
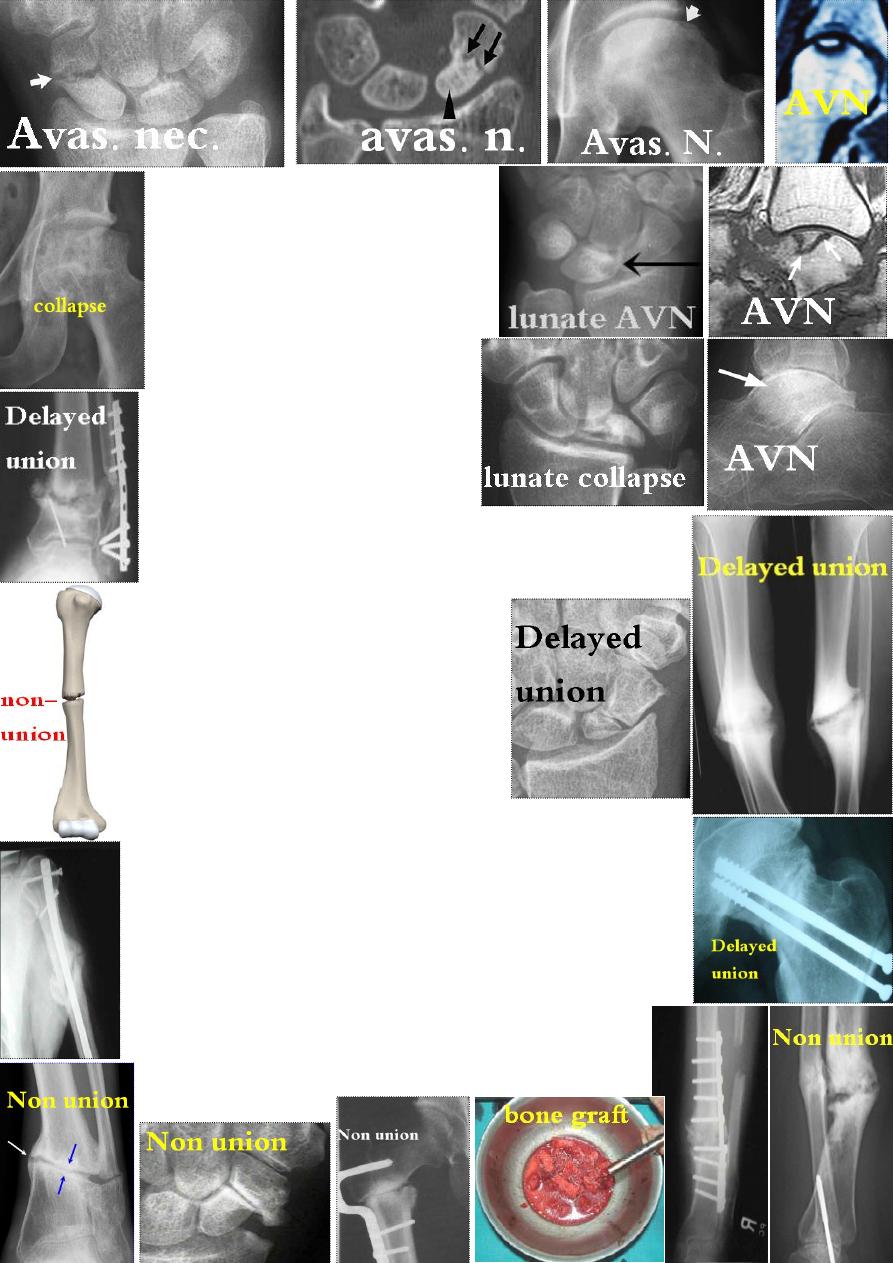
Bone complications:
Avascular necrosis
:
the usual sites are:
1- head of femur (after
neck # or hip ≠).
2-
proximal part of scaphoid ( waist # ).
3- lunate (after dislocation).
4- talus body (following neck # ).
CF: after weeks or months, there will
be nonunion or collapse of the affected
bone causing pain & stiffness.
x-ray: ↑ density of the ischemic bone
due to new bone ingrowth and disuse
osteoporosis of the surrounding bones.
Delayed union: is undue prolongation
of the time required for a given # to unite.
Causes: 1- inadequate blood supply e.g. lower tibia, segmental,
femoral neck, scaphoid &talus fractures. 2-infection,
3-incorrect splintage, 4-intact fellow bone
e.g. fractured tibia with intact fibula.
CF: the # site is still tender, if stress the
bone, it is painful and may angulate.
X-ray shows the # line with little callus.
Ŗ→ Ŗ the cause, like infection; correct the
splintage; excise 2.5cm of the intact fellow
bone e.g. fibula. If all fail → bone grafting.
Non union: if delayed union left untreated, it ends with non union.
Causes: 1- too large a gap e.g. bone loss or excessive traction.
2- soft tissue interposition like muscle, periosteum or cartilage.
3- pathological lesion in bone. 4- intra articular # due to synovial
fluid dissolving # hematoma. 5- same causes of delayed union.
CF: painless MVT at the # site.
X-ray: the # line is smooth & sclerotic.
Types of nonunion: 1- Hypertrophic: huge callus at both ends;
2- Atrophic: with no callus at bone ends.
Ŗ→ Conservative: some require nothing, others require
functional bracing or electrical stimulation.
Operative: rigid fixation (internal or external) & bone
Grafting (if atrophic).
.
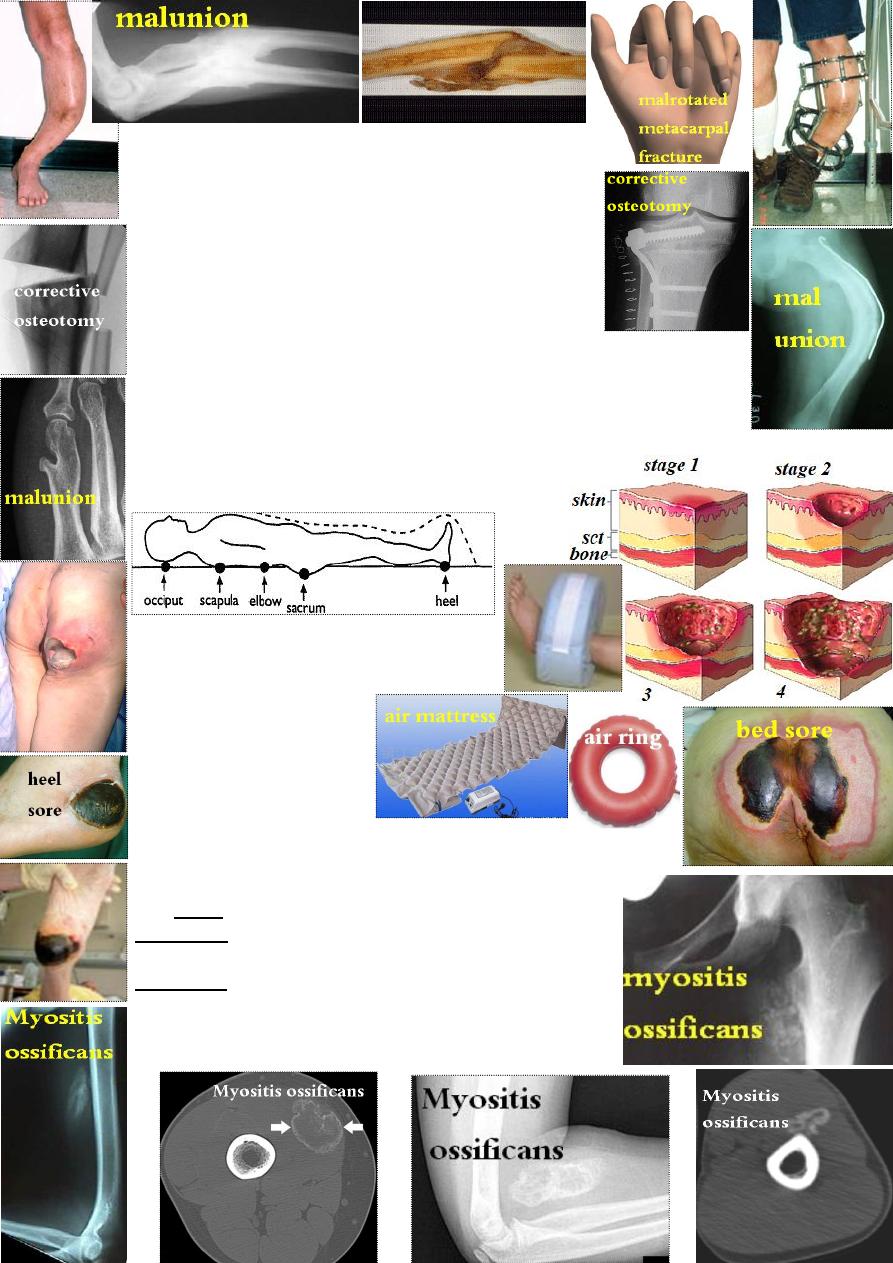
Malunion:
means unacceptable angulation, shortening or rotation.
In the lower limb, 2cm shortening or 15˚ angulation is
acceptable. CF: malunion may be evident, comparism
with other side is of help. X-ray: for measurement.
Ŗ→ MUA to acceptable alignment or if fully united,
corrective osteotomy with internal or external fixation.
Growth disturbance:
In children, # that pass transversely through growth plate are usually
harmless, while those splitting growth plate are more dangerous bec.
of later asymmetrical growth. Fractures that damage the entire growth
plate may cause slowing or arrest of growth leading to shortening.
Sometimes, hyperaemia may accelerate growth leading to bone
lengthening.
Soft tissue complications:
Bed sore:
The usual sites are over sacrum & heel.
It is ˃ common in old ¶lyzed patients.
Prevention: careful nursing
& early mobilization.
Ŗ→ debridement &
skin graft.
Myositis ossificans:
Is a heterotopic ossification in muscle following injury.
The usual sites is elbow or arm, sometimes, it occur without
history of local trauma as in unconscious or elderly patients.
ray is normal.
-
X
tenderness.
pain, swelling &
:
early
:
CF
the joint become stiff.
: the pain ↓ &
3 weeks
At
X-ray shows fluffy calcifications.
ray.
-
can be felt and seen on X
mass
y
: a bon
At 8 weeks
Ŗ→ rest the joint in position of function till pain subside,
then start gentle active (not passive) exercise. Later, the
bony mass, if limit the joint MVT, can be excised.

Tendonitis: like tibialis posterior tendonitis in ankle #.
Tendon rupture: like extensor pollicis longus tendon
rupture after 2 months of Colle's #. Ŗ→ transfer of
extensor indicis tendon to distal stump of EPL.
Nerve compression:
a
entrapment in the callus of
nerve
al
radi
like
compression
nerve
median
; or
humerus #
healing
in the carpal tunnel after Colle's # because of
deformity &callus; or ulnar neuritis due to cubitus
valgus resulting from
un united lateral condyle
# of humerus.
Joints complications:
Joint instability: causes:
1- ligament injury;
2- muscle weakness due to immobilization;
3- bone loss as in bullet injury.
Recurrent joint dislocation: like
shoulder and patella recurrent traumatic
dislocation, due to poor healing of
stabilizing soft tissue (ligaments &capsule).
Joint stiffness:
Common sites: shoulder, elbow, knee & hands.
Causes:
1- intra articular causes: trauma to the joint causes
haemarthrosis → synovial adhesions.
2- peri articular causes: edema in the capsule & soft
tissues around the joint→ fibrosis & adhesion.
3- extra articular causes: adhesion of soft tissue &
muscle to underlying bone causes limitation of MVT.
Prevention: early exercise from the start and, if the joint
has to be splinted, this should be in a position of function
where the ligaments are at their longest (position of safety).
Ŗ→ physiotherapy, MUA, operative release of adhesion.
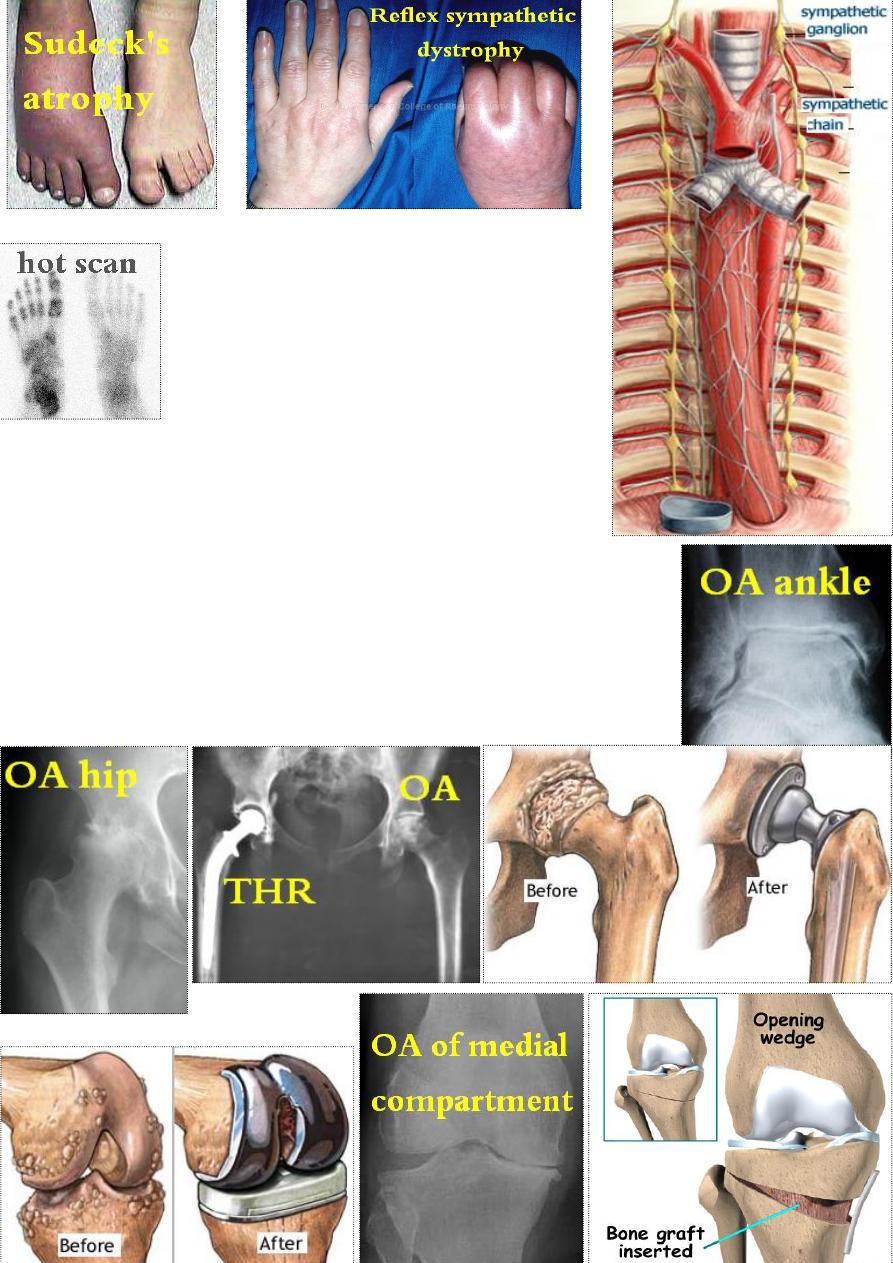
Reflex sympathetic dystrophy (algodystrophy, Sudeck's
atrophy, complex regional pain syndrome): is
due to peripheral sympathetic over activity.
Early: continuous burning pain, swelling, redness
&warmth of the affected part e.g. following
Colle's #, the hand is affected.
After few weeks: stiffness ↑&skin become atrophic.
X-ray shows patchy osteoporosis.
Ŗ→ elevation, active exercise, NSAID, severe cases
may get benefit from IV gaunithidine (sympatholytic
drug). Finally, sympathectomy may be required.
Osteoarthritis: causes:
1- intra articular # may damage the articular cartilage
causing early OA (within months); or imperfect
reduction of the # with irregularity of the joint surfaces
causing late OA.
2- malunited shaft # may alter the mechanics
of nearby joints causing late OA.
Ŗ→ early, conservative. Late, operative:
Realignment osteotomy or Joint replacement.
