شهرزاد سامي
Dental RadiologyRadiolucent Lesions
Radicular Cyst
Radicular cyst also known as apical periodontal cyst, periapical cyst or dental root canal cyst. It’s usually appears as a well-defined, rounded or pear shaped, unilocular radiolucent lesion in the periapical region of non vital tooth and commonly measured less than one cm.
Radicular cyst may be classified as odontogenic cyst in addition to inflammatory cyst, since its arise from epithelial rests of Malassez which is the remnant of Hertwigs epithelial root sheath and is the outcome of odontogenic epithelial layer.
Residual radicular cyst
This term refers to a radicular (dental) cyst remaining after the causative tooth has been extracted.Age: Adults, 20 years old and older.
Radiodensity: Uniformly radiolucent.
Effects: Adjacent teeth displaced, rarely resorbed
— Buccal expansion
— Displacement of the antrum
Lateral periodontal cyst
It is thought to develop from either the cell rests of the dental lamina or from remains of the reduced enamel epithelium on the lateral surface of the root.Site: Lateral surface of the roots of vital teeth in the lower canine/premolar region or upper lateral incisor region.
Shape: — Monolocular, very occasionally multilocular
— Round.
Outline: — Smooth
— Well defined and corticated.
Radiodensity: Uniformly radiolucent.
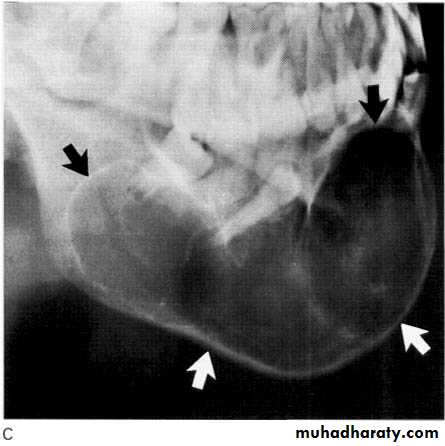
Dentigerous (follicular) cyst
This cyst develops from the remnants of the reduced enamel epithelium after the tooth has formed.
Site: Associated with the crown of an unerupted e.g. 3|3 and 8|8.
Size: Very variable, cyst suspected if follicular space exceeds 3 mm but may grow to several centimeters in diameter and extend up into the ramus.
Shape: — Round or oval, typically enveloping the crown symmetrically
— Monolocular
Outline: — Smooth
— Well defined
— Often well corticated.
• Radiodensity: Uniformly radiolucent
Odontogenic keratocyst (primordial cyst)
This cyst develops from the epithelium of the dental lamina instead of the normal tooth.• Site: — Posterior body/angle of the mandible extending into the ramus
— Anterior maxilla in canine region.
Size: Variable, but often large in the mandible.
• Shape: — scalloped, extending along the body of the mandible
Outline: — Smooth
— Well defined
— Often well corticated.
• Radiodensity. The internal structure is most commonly radiolucent. The presence of internal keratin does not increase the radiopacity. In some cases, curved internal septa may be present, giving the lesion a multilocular appearance.
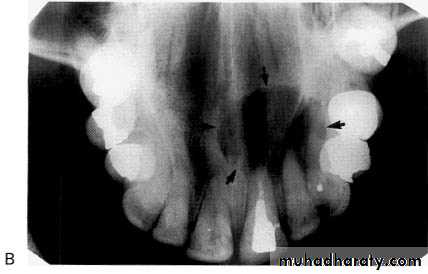
Nasopalatine duct/incisive canal cyst
This cyst develops from epithelial remnants of the nasopalatine duct or incisive canal.
• Site: Midline, anterior maxilla just posterior to the upper central incisors.
• Shape: — Round or oval (superimposition of the nasal septum or anterior nasal spine may cause the cyst to appear heart-shaped or resemble an inverted tear drop)
— Monolocular.
• Outline: — Smooth
—Well defined
—Well corticated (unless infected).
• Radiodensity: Uniformly radiolucent
Nasolabial Cyst
The exact origin of nasolabial cysts is unknown. They may be fissural cysts arising from the epithelial rests in fusion lines of the globular, lateral nasal, and maxillary processes. Alternatively, the source of the epithelium may be from the embryonic nasolacrimal duct.Location. Nasolabial cysts are primarily soft tissue lesions located adjacent to the alveolar process above the apices of the incisors. Because this is a soft tissue lesion, plain radiographs may not show any detectable changes. The investigation could include either CT imaging or magnetic resonance imaging, both of which can provide an image of soft tissues
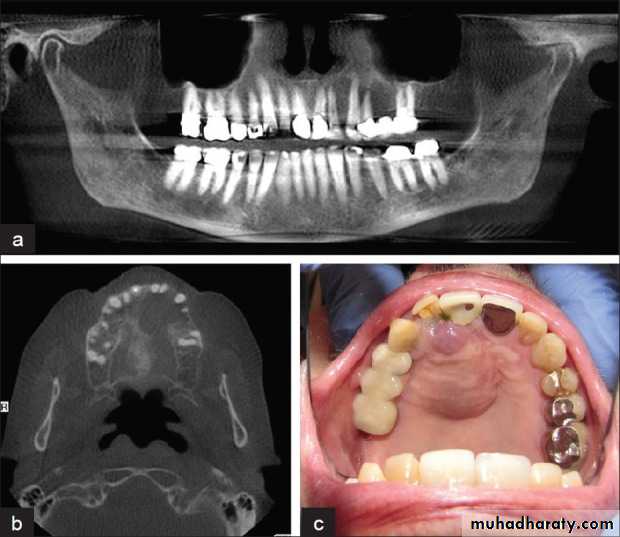
Odontogenic tumours Ameloblastoma
This is an aggressive but non-metastasizing tumour originating from remnants of the odontogenic epithelium of the enamel organ or dental lamina.•Site: Posterior body/angle/ramus of mandible, very occasionally involves the maxilla.
• Shape: — Multilocular,
— Occasionally monolocular in early stages
— Rarely honeycomb or soap-bubble appearance or multicystic
• Outline: — Smooth and scalloped
— Well defined
— Well corticated.
• Radiodensity: Radiolucent with internal radiopaque septa.
Ameloblastic Fibroma
A rare, benign, mixed odontogenic tumour originating from both the odontogenic epithelium and the connective tissue of the developing tooth germ.
Radiographically these tumours closely resemble ameloblastomas but develop in a younger age group.
Age: Children and adolescents.
Site: Mandible (usually) or maxilla premolar/ molar region.
Size: Variable.
Shape: — Multilocular
— Monolocular in the early stages.
Outline: — Smooth
— Well defined
— Well corticated.
Radiodensity: Radiolucent with internal radiopaque septa if multilocular.
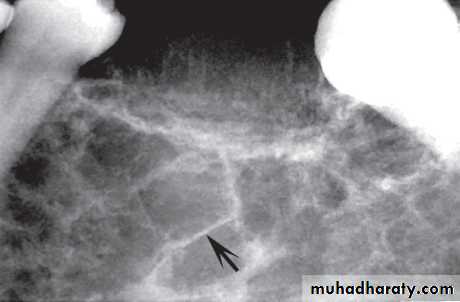
Odontogenic Fibroma and Myxoma
These very similar non-invasive tumors originate from the odontogenic connective tissue fibroblasts of the developing tooth germ, which produce either excessive fibrous collagen (fibroma) or excessive ground substance (myxoma). Radiographically they are often indistinguishable.Age: Young adults.
Site: Posterior mandible or maxilla.
Shape: — Multilocular
— Occasionally monolocular
— May be associated with a missing or unerupted tooth.
Outline: — Smooth and often scalloped
— Well defined with variable cortication
Radiodensity: Radiolucent with fine internal radiopaque septa or trabeculae often arranged at right angles to one another, producing an appearance sometimes described as resembling the strings of a tennis racket.
Multiple Myeloma
Multifocal proliferation of the plasma cell series within the bone marrow, resulting in overproduction of immunoglobulins.• Age: Adults, middle-aged.
• Site: Multiple lesions affecting:
— Skull vault
— Posterior parts of the mandible
— Other parts of the skeleton.
Radiodensity: Radiolucent
Outline: Punched-out border
Central giant cell granuloma
A relatively uncommon, non-neoplastic mass in the jaws producing an expansible radiolucent lesion.• Age: Variable, but usually young adolescents and adults under 30 years old.
Origin: Giant cells involved in the lesion may have been derived from the odontoclasts, which led to resorption of the deciduous teeth. This might explain why they were found in a certain age group and generally found in areas of the jaws that had previously held deciduous teeth.
Sit: Mandible, anteriorly often crossing the midline and maxilla.
Size: Very variable, up to 6 cm in diameter.
Shape: Multilocular, may be monolocular in early stages.
Outline: — Smooth and undulating
— Moderately well defined
— Generally not well corticated
Radiodensity: Radiolucent, larger lesions have thin internal septa or trabeculae producing the multilocular, or sometimes honeycomb appearance.
Squamous cell carcinoma
Squamous cell carcinomas of the oral mucosa directly overlying bone, in their latter stages, often invade the underlying bone to produce a destructive radiolucency.• Age: Adults over 50 years old.
• Site: Mandible, or maxilla if originating in the antrum.
Shape: Irregular area of bone destruction often initially saucer-shaped.
Outline: — Irregular and moth-eaten
— Poorly defined
— Not corticated.
Radiodensity: Radiolucent, radiodensity dependent on degree of destruction.
Secondary (Metastatic) Bone Tumors
Carcinomas from the bronchus, breast, prostate, kidney and thyroid sometimes metastasize to the jaws and produce the typical destructive radiolucency of a malignant lesion.
• Site: Usually centrally in the mandible, molar and premolar regions, occasionally at the apex of a tooth.
Shape: Irregular area or areas of bone destruction
• Outline: — Irregular and moth-eaten
— Poorly defined, not corticated.
• Radiodensity. Radiolucent, but some carcinomas from the prostate and breast may be osteogenic and show areas of bone production/sclerosis.