Pulpal diseases and related periapical pathosis
PULPAL DISEASES
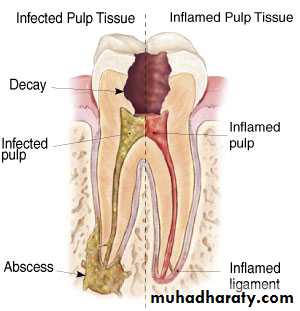
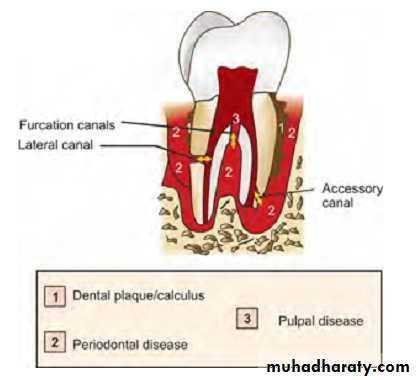
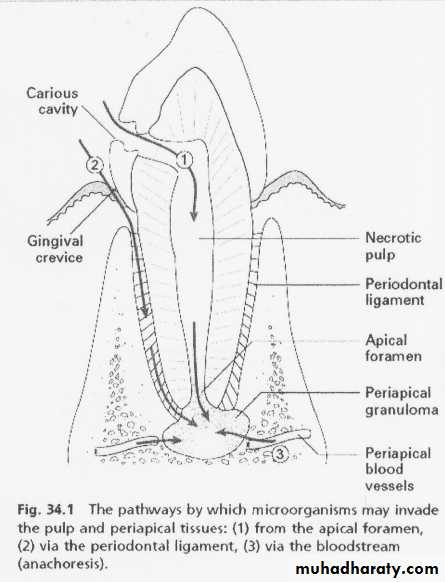
Etiology1. Bacteria and bacterial irritants: bacteria are a main cause of pulpal inflammation. Bacteria or their products may enter pulp through a break in dentin either from:
Caries
Accidental exposure
Fracture
Percolation around a restoration
Extension of infection from gingival sulcus
Periodontal pocket and abscess
Anachoresis (Process by which microorganisms get carried by the bloodstream from another source localize on inflamed tissue).
2. Traumatic
a) Acute trauma like fracture, luxation or avulsion of tooth.b) Chronic trauma including para-functional habits like bruxism.
3. Iatrogenic (Pulp inflammation for which the dentists own procedures are responsible is designated as Dentistogenic pulpitis). Various iatrogenic causes of pulpal damage can be:
a. Thermal changes generated by cutting procedures, during restorative procedures, bleaching of enamel, electrosurgical procedures, laser beam, etc. can cause severe damage to the pulp if not controlled.
b. Orthodontic movement
c. Periodontal curettage
d. Periapical curettage
e. chemicals: A use of chemicals like temporary and permanent fillings, liners and bases and use of cavity desiccants such as alcohol.
4. Idiopathic
a. Agingb. Resorption: internal or external
5. Radiation therapy: Radiation therapy affect pulps of fully formed teeth in patients exposed to radiation therapy. The pulp cells exposed to ionizing radiation may become necrotic, there may occur vascular damage and the interference in mitosis of cells.
Progression of pulpal pathologies
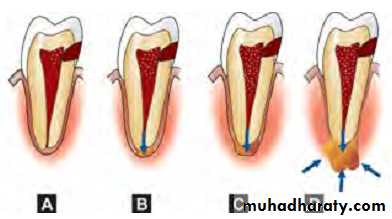
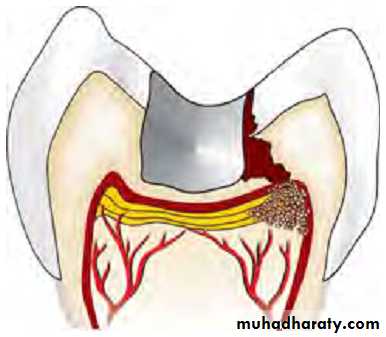
Pulp reacts to above mentioned irritants as do other connective tissues. Degree of inflammation is proportional to intensity and severity of tissue damage. For example, slight irritation like incipient caries or shallow tooth preparation cause little or no pulpal inflammation, whereas extensive operative procedures may lead to severe pulpal inflammation.Pulpal reaction to microbial irritation
Carious enamel and dentin contains numerous bacteria↓
Bacteria penetrate in deeper layers of carious dentin
↓
Pulp is affected before actual invasion of bacteria via their
toxic byproducts
↓
Byproducts cause local chronic cell infiltration
↓
When actual pulp exposure occurs pulp tissue gets locally infiltrated by PMNs to form an area of liquefaction necrosis at the site of exposure
↓
Eventually necrosis spreads all across the pulp and periapical tissue resulting in severe inflammatory lesion.
Diagnostic aids for pulpal pathology
• Subjective symptoms—most common being pain• Objective symptoms
1. Visual and tactile inspection — 3Cs rule–
i. Color
ii. Contour
iii. Consistency
2. Thermal tests
i. Heat tests— isolation of tooth — use of:– Warm air
– Hot water
– Hot burnisher
– Hot gutta-percha stick
ii. Cold tests:
– Ethyl chloride spray
– Ice pencils
– CO2 snow — temperature 18ºC
3. Electrical pulp testing
4. Radiographs
5. Anesthetic tests
6. Bite test
7. Cavity test
8.Recent advances in diagnostic aids for pulpal pathology include:
Laser Doppler flowmetry
Pulp oximetry
Pulp conditions
Normal when there is a response to the stimulus provided by the sensibility test and this response is not pronunced or exaggerated,and it does not lingerPulpitis is present when there is an exaggerated response that produce pain. Pulpitis can be considered as reversible or irreversible, depending on the severity of pain and whether the pain lingers or not.
Pulp necrosis: the pulp tissuues are dead
Pulpal diseases
1) Reversible pulpitis/hyperemia/hyperactive pulpalgiaDefinition: Pulpal inflammation, the tissue is capable of returning to a normal state of health.
Etiology: Pulpal irritation to external stimuli is related to dentin permeability. Under normal circumstances, enamel and cementum act as impermeable barrier to block the patency of dentinal tubules at dentinoenamel junction or dentinocemental junction.
Other factors:
• Trauma– Accident or occlusal trauma
• Thermal injury
– While doing tooth preparation
– Overheating during polishing of a restoration
• Chemical stimulus—Like sweet or sour foodstuff
• Following insertion of a deep restoration
Symptoms:
- Symptomatic reversible pulpitis is characterized by sharp pain lasting for a moment, commonly caused by cold stimuli. Pain does not occur spontaneously and does not continue when irritant is removed.- Asymptomatic reversible pulpitis may result from incipient caries and is resolved on removal of caries and proper restoration of tooth.
Diagnosis
1. Pain: It is sharp but of brief duration, ceasing when irritant is removed.2. Visual examination and history: It may reveal caries, traumatic occlusion and undetected fracture.
3. Radiographs: These show normal PDL and lamina dura.– Depth of caries or restoration may be evident.
4. Percussion test: It shows negative responses, i.e. tooth is not tender to percussion.
5. Vitality test: Pulp responds readily to cold stimuli. Electric pulp tester requires less current to cause pain.
Treatment
• No endodontic treatment is needed for this condition. The best treatment of reversible pulpitis is prevention.• Usually, a sedative dressing is placed, followed by permanent restoration when symptoms completely subside.
• Periodic care to prevent caries, desensitization of hypersensitive teeth and use of cavity varnish or base before insertion of restoration is recommended.
• If pain persists in spite of proper treatment, pulpal inflammation should be considered as irreversible and it should be treated by pulp extirpation.
2) Irreversible pulpitis
DefinitionIt is a persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by a noxious stimulus. It has both acute and chronic stages in pulp.
Etiology
• Most common cause of pulpitis is bacterial involvement of pulp through caries
• Chemical, thermal, mechanical injuries of pulp may induce pulp inflammation
• Reversible pulpitis when left untreated deteriorates into irreversible pulpitis.
Symptoms
• A rapid onset of pain, which can be caused by sudden temperature change, sweet or acidic food. Pain remains even after removal of stimulus• Pain can be spontaneous in nature which is sharp, piercing, intermittent or continuous in nature
• Pain exacerbated on bending down or lying down due to change in intrapulpal pressure
• Presence of referred pain
• In later stages, pain is severe, boring, throbbing in nature which increases with hot stimulus. Pain is so severe that it keeps the patient awake in night. The relief of pain can be simply done by use of cold water. The patient may report dental office with jar of ice water.
Diagnosis
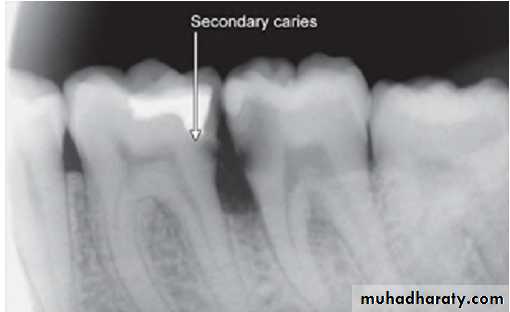
Visual examination and history: Examination of involved tooth may reveal previous symptoms. On inspection, one may see deep cavity involving pulp or secondary caries under restorations.2. Radiographic findings:
– May show depth and extent of caries.– Periapical area shows normal appearance but a slight widening may be evident in advanced stages of pulpitis.
3. Percussion: Tooth is tender on percussion (due to increased intrapulpal pressure as a result of exudative inflammatory tissue).
4. Vitality tests:
i. Thermal test: pulp responds more readily to cold stimulation than for normal tooth, pain may persist even after removal of irritant.
As the pulpal inflammation progresses, heat intensifies the response because it has expansible effect on blood vessels. Cold tends to relieve pain because of its contractile effect on vessels, reducing the intrapulpal pressure.
ii. Electric test: Less current is required in initial stages. As tissue becomes more necrotic, more current is required.