T
HE
F
EMALE
R
EPRODUCTIVE
S
YSTEM
Assist.prof. Dr.Hammed N.Mousa
Consultant pathology.

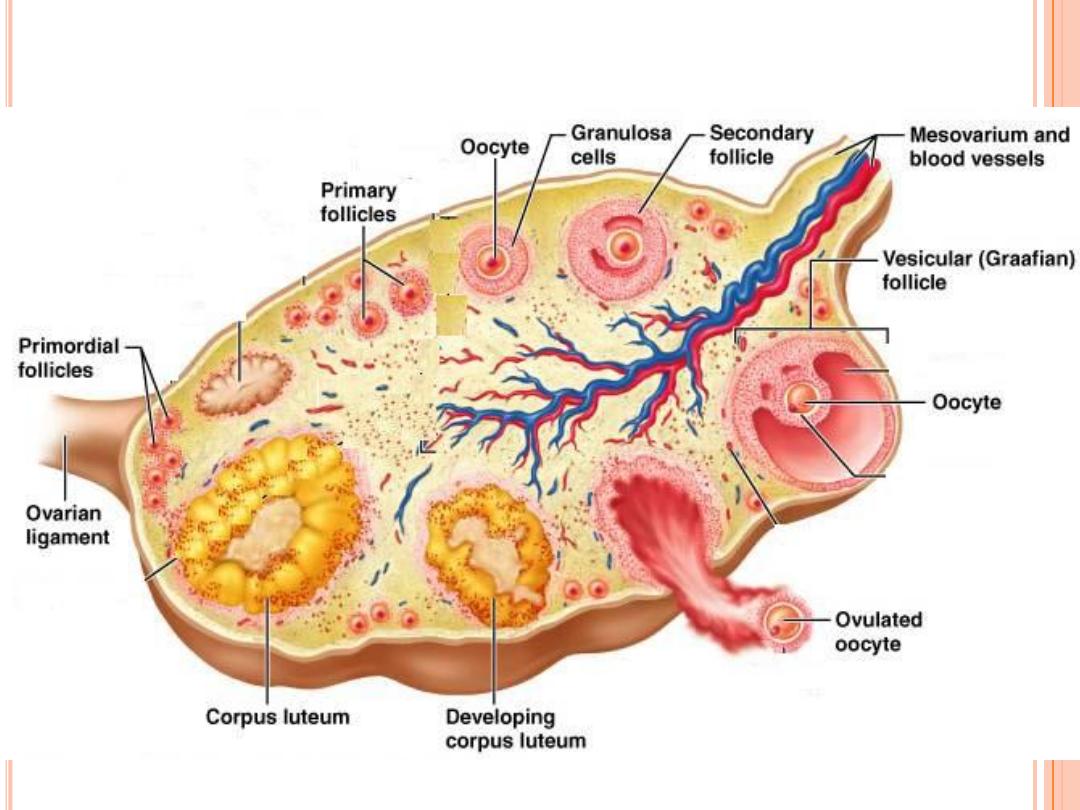
The Ovaries
The ovaries have two functions - "
production" and ovulation of oocytes and the
production and secretion of hormones.
The ovary is attached to the broad
ligament by a short fold of peritoneum, called the mesovarium (or ligament of the
ovary), through which vessels and nerves pass to the ovary and enter it at the
hilus of the ovary.
The surface of the ovary is covered by a single layer of cuboidal epithelium, also
called
germinal epithelium
. It is continuous with the peritoneal mesothelium.
Fibrous connective tissue forms a thin capsule, the tunica albuginea, immediately
beneath the epithelium.
the ovary is divided into an outer cortex and an inner medulla. The cortex
consists of a very cellular connective tissue stroma in which the ovarian follicles
are embedded. The medulla is composed of loose connective tissue, which
contains blood vessels and nerves.

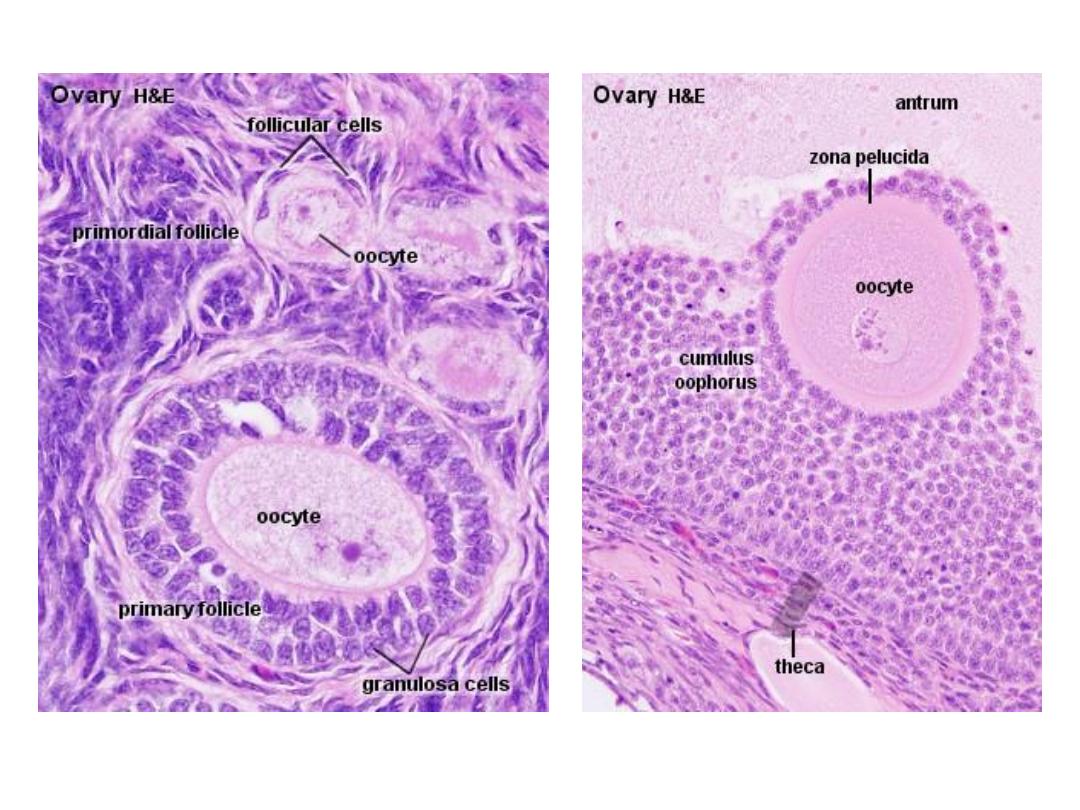
Ovarian Follicles
Ovarian follicles consist of one oocyte and surrounding follicular cells. Follicular
development can be divided into a number of stages.
Primordial follicles
are located in the cortex just beneath tunica albuginea. One layer of flattened follicular
cells surround the oocyte (about 30 µm in diameter). The nucleus of the oocyte is
positioned eccentric in the cell. It appears very light and contains a prominent nucleolus.
Most organelles of the oocyte aggregate in the centre of the cell, where they form the
vitelline body (probably not visible in any of the available preparations).

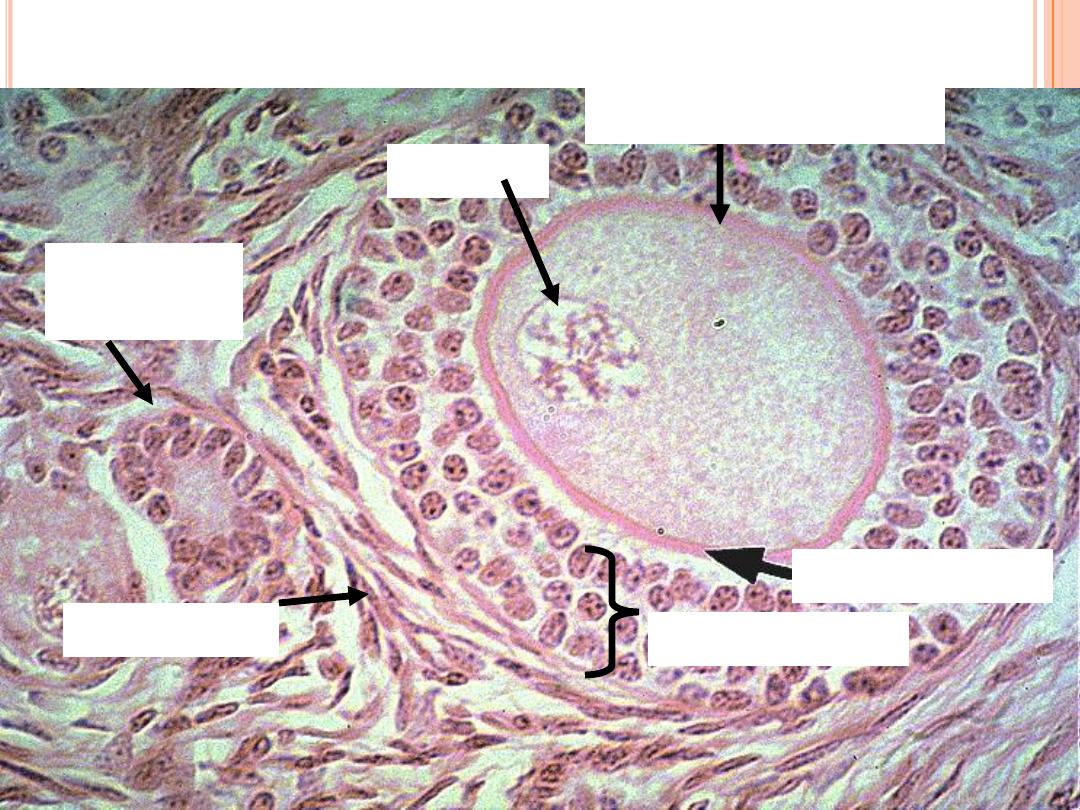
The primary follicle
is the first morphological stage that marks the onset of follicular maturation (Which
hormone stimulates follicular maturation and where is this hormone produced?). The
previously flattened cell surrounding the oocyte now form a cuboidal or columnar
epithelium surrounding the oocyte. Their cytoplasm may have a granular appearance,
and they are for this reason also called
granulosa cells
. The continued proliferation of
these cells will result in the formation of a stratified epithelium (with a distinct
basement membrane) surrounding the oocyte. The
zona pellucida
(glycoproteins
between interdigitating processes of oocyte and granulosa cells) becomes visible.
Parenchymal cells of the ovary surrounding the growing follicle become organised in
concentric sheaths, the
theca folliculi
.
F
EMALE
R
EPRODUCTION
Unlike males, who are
able to produce sperm
cells throughout their
reproductive lives,
females produce a
finite number of egg
cells.
During early fetal
development germ
cells migrate into the
ovaries and
differentiate into
oogonia

Secondary follicle
Small fluid-filled spaces become visible between the granulosa cells as the follicle reaches
a diameter of about 400 µm. These spaces enlarge and fuse to form the follicular antrum,
which is the defining feature of the secondary follicle. The oocyte is now located
eccentric in the follicle in the
cumulus oophorus
, where it is surrounded by granulosa
cells. The theca folliculi differentiates with the continued growth of the follicle into a
theca interna and a theca externa
. Vascularization of the theca interna improves, and the
spindle-shaped or polyhedral cells in this layer start to produce
oestrogens.
The theca
externa retains the characteristics of a highly cellular connective tissue with smooth
muscle cells. The oocyte of the secondary follicle reaches a diameter of about 125 µm.
The follicle itself reaches a diameter of about
10-15 mm.

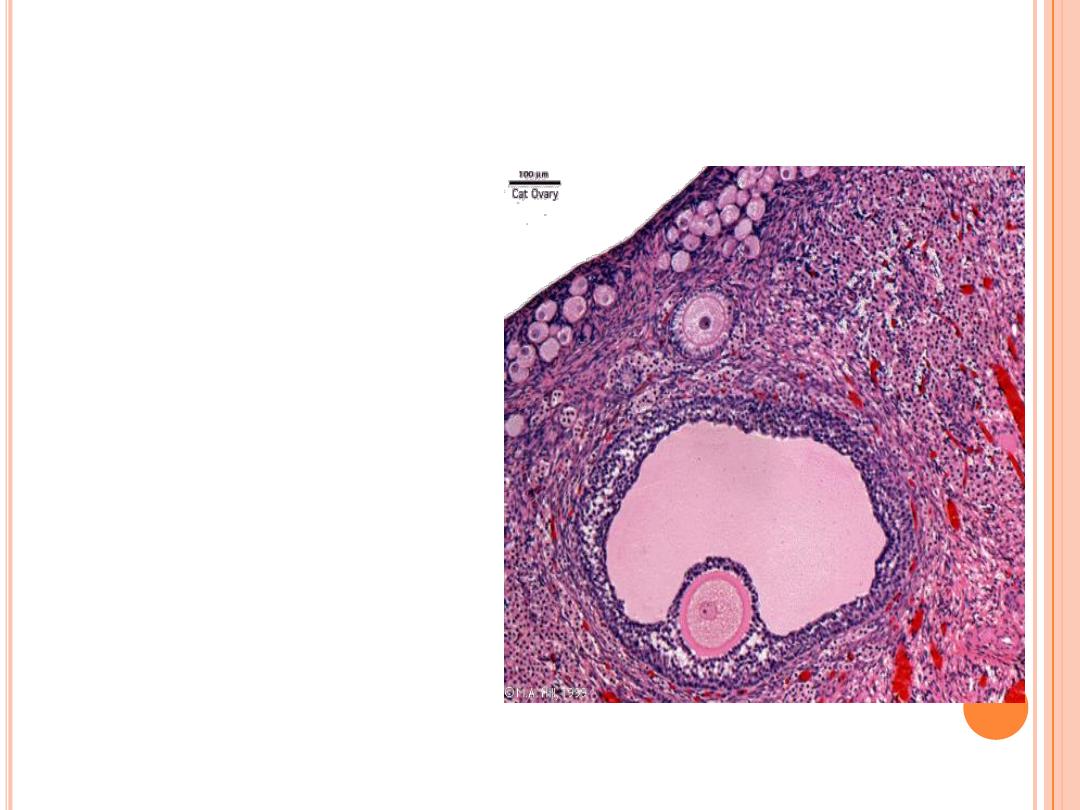
The mature or tertiary or preovulatory or Graafian follicle
increases further in size (in particular in the last 12h before ovulation). The Graafian
follicle forms a small "bump" on the surface of the ovary, the stigma (or macula
pellucida). The stigma is characterised by a thinning of the capsule and a progressive
restriction of the blood flow to it. Prior to ovulation the cumulus oophorus separates
from the follicular wall. The oocyte is now floating freely in the follicular antrum. It is
still surrounded by granulosa cells which form the
corona radiata
. The follicle finally
ruptures at the stigma and the oocyte is released from the ovary.

9
O
VARIES
Each follicle consists of an immature egg called an
oocyte
Cells around the oocyte are called:
Follicle cells
(one cell layer thick)
Stimulated to mature by FSH from the pituitary gland
Granulosa cells
(when more than one layer is present)
Thecal cells
: Cells in the ovarian stroma
Thecal & granulosa cells work together to produce
estrogen
A protective layer of glycoprotein forms around the
egg called the zona pellucida

10
F
OLLICLE
D
EVELOPMENT
1.
Primordial follicle
: one layer of squamous-
like follicle cells surrounds the oocyte
2.
Primary follicle:
two or more layers of
cuboidal granulosa cells enclose the oocyte
3.
Secondary follicle:
has a fluid-filled space
between granulosa cells that coalesces to
form a central antrum
4.
Graafian follicle
: secondary follicle at its
most mature stage that bulges from the
surface of the ovary
5.
Corpus luteum
: ruptured follicle after
ovulation

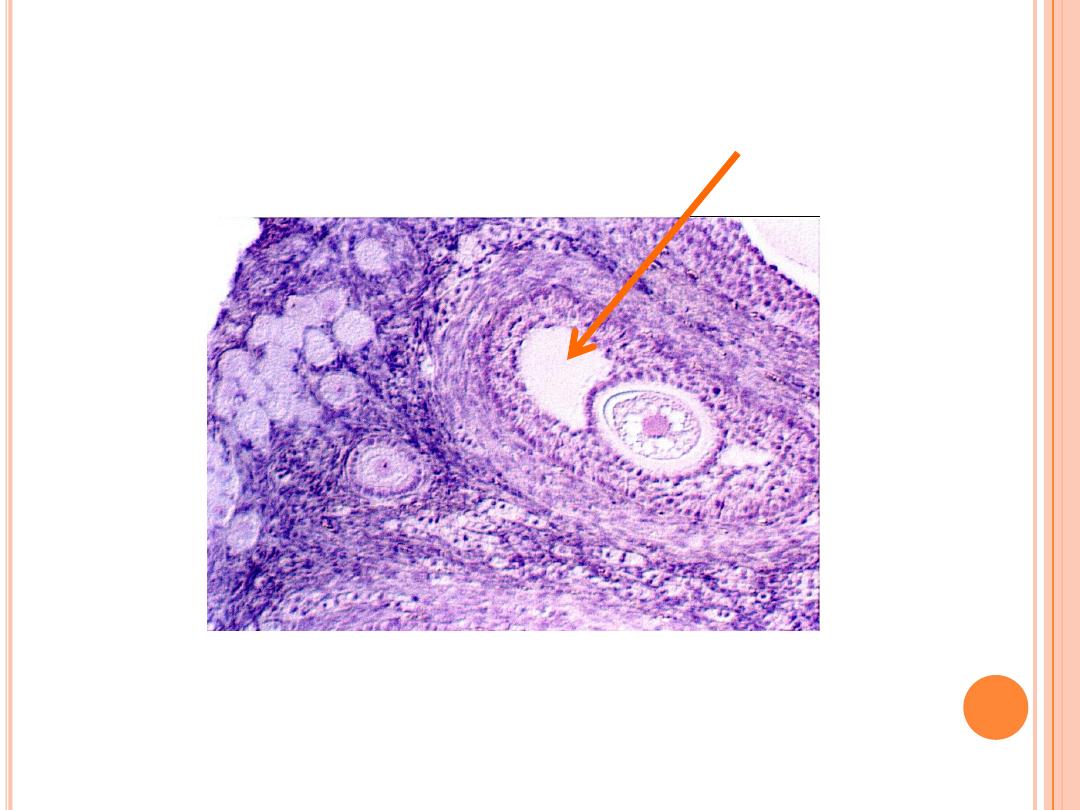
Atresia
Atresia is the name for the degenerative process by which oocytes (and follicles) perish
without having been expelled by ovulation. Only about 400 oocytes ovulate - about 99.9 %
of the oocytes that where present at the time of puberty undergo atresia. Atresia may effect
oocytes at all stages of their "life" - both prenatally and postnatally. By the sixth month of
gestation about 7 million oocytes and oogonia are present in the ovaries. By the time of
birth this number is reduced to about 2 million. Of these only about 400.000 survive until
puberty.
Atresia is also the mode of destruction of follicles whose maturation is initiated during the
cyclus (10-15) but which do not ovulate. Atresia is operating before puberty to remove
follicles which begin to mature during this period (none of which are ovulated). Given that
atresia affects follicles at various stages of their development it is obvious that the process
may take on quite a variety of histological appearances.
The Corpus luteum
The corpus luteum is formed by both granulosa cells and thecal cells after
ovulation has occurred. The wall of the follicle collapses into a folded structure,
which is characteristic for the corpus luteum. Vascularization increases and a
connective tissue network is formed. Theca interna cells and granulosa cells triple
in size and start accumulating lutein (Which hormone stimulates this process?
Where is this hormone produced?) within a few hours after ovulation. They are
now called granulosa lutein cells and theca lutein cells and produce
progesterone
and oestrogens.
Hormone secretion in the corpus luteum ceases within
14 days
after ovulation if
the oocyte is not fertilised. In this case, the corpus luteum degenerates into a
corpus albicans
- whitish scar tissue within the ovaries.
Hormone secretion continues for
2-3 month
after ovulation if fertilisation occurs.
13
O
VARY
H
ISTOLOGY
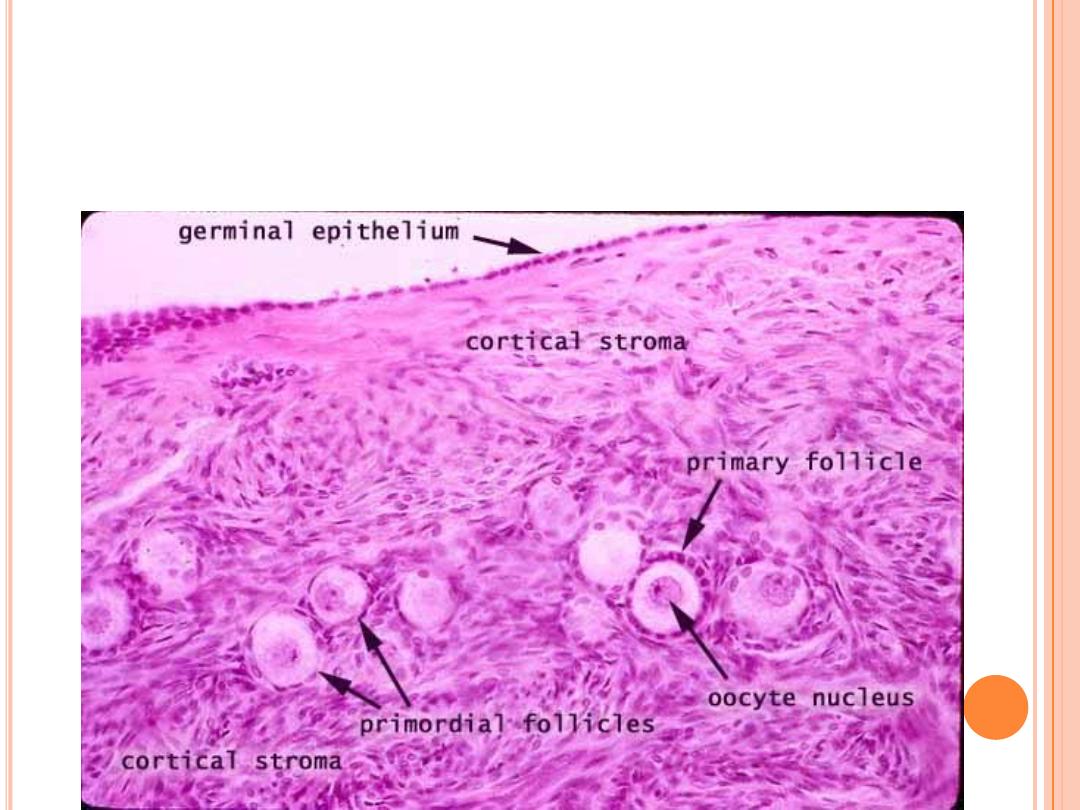
14
O
VARY
H
ISTOLOGY
15
Zona pellucida
1° Oocyte
Granulosa cells
Thecal cells
Nucleus
Primordial
follicle
Primary Follicle
16
S
ECONDARY
F
OLLICLE
Fluid-filled
antrum
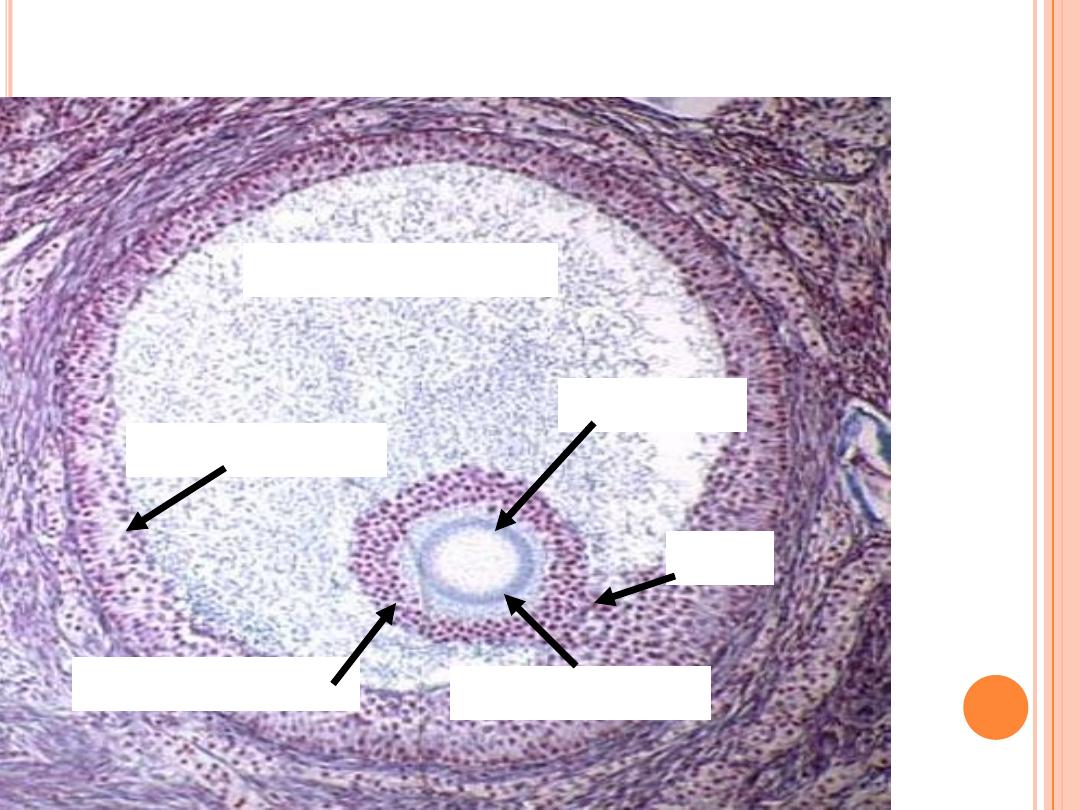
17
G
RAAFIAN
F
OLLICLE
Fluid filled antrum
Granulosa cells
Oocyte 2°
Corona radiata
Stalk
Zona pellucida
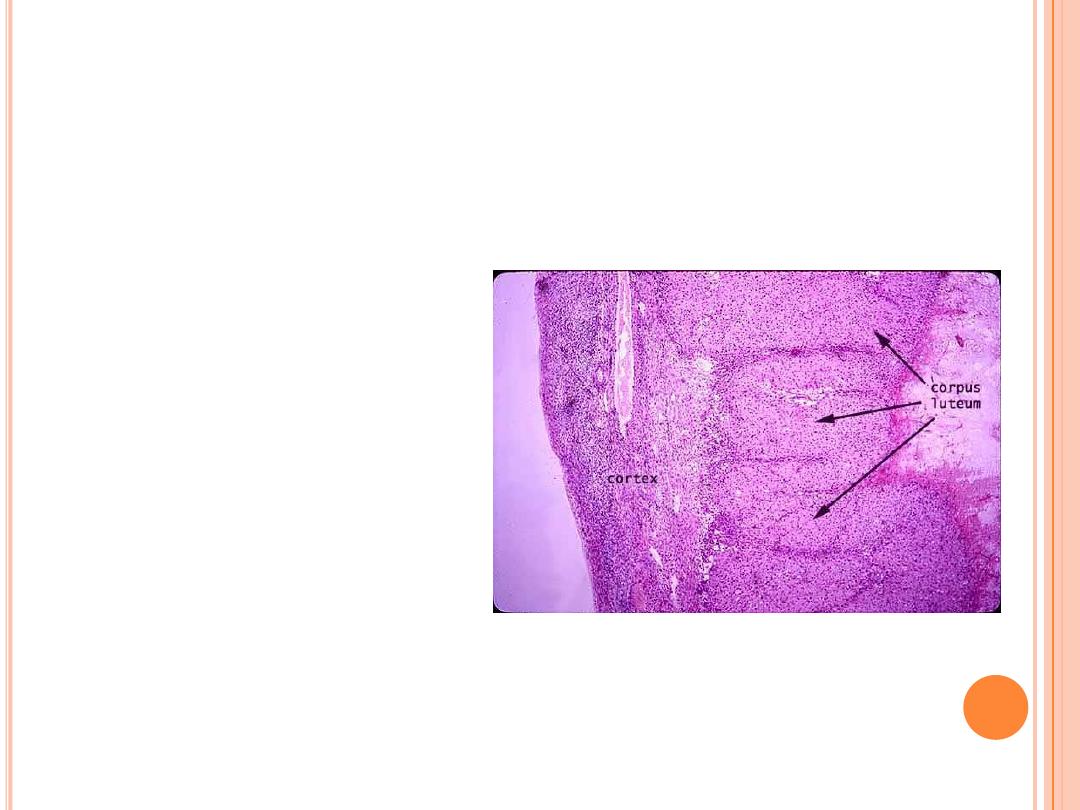
C
ORPUS LUTEUM
After ovulation, the
remains of the follicle
are transformed into a
structure called the
corpus luteum.
If a pregnancy occurs,
it produces
progesterone to
maintain the wall of
the uterus during the
early period of
development.
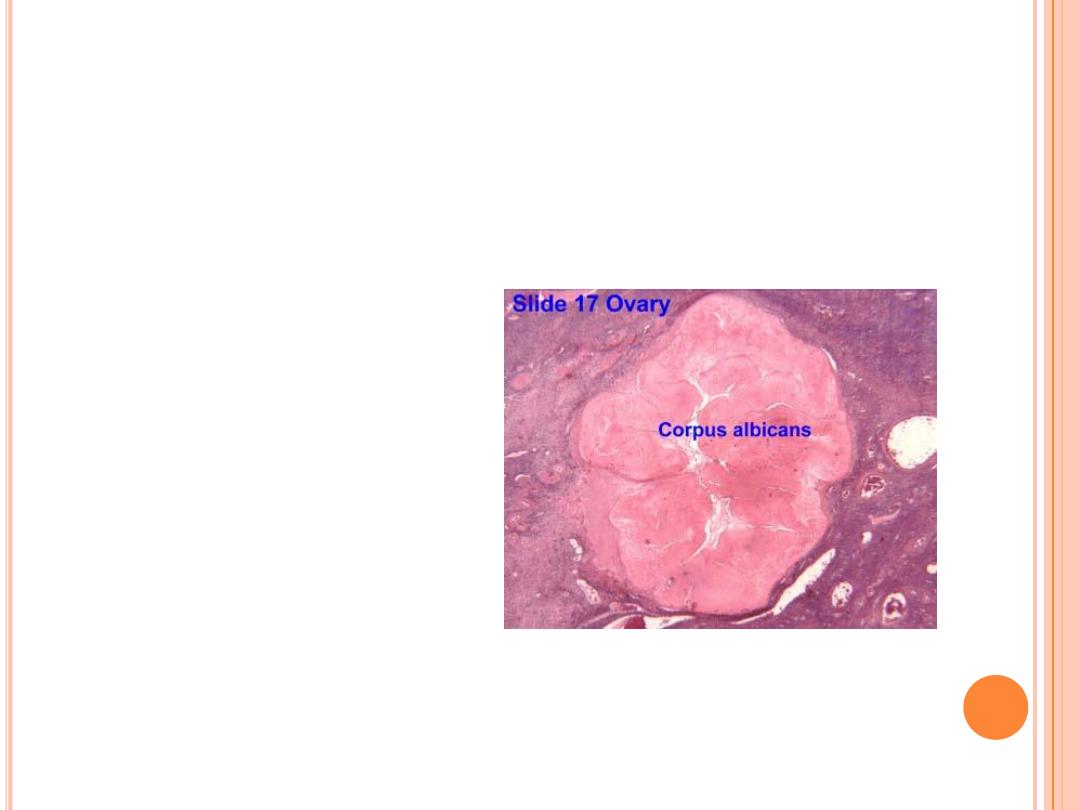
C
ORPUS ALBICANS
If fertilization does
not occur, the corpus
luteum will begin to
break down about 2
weeks after ovulation.
Degeneration occurs
when fibroblasts enter
the corpus luteum and
a clump of scar tissue
forms called the
corpus albicans.
Fallopian tube)
)
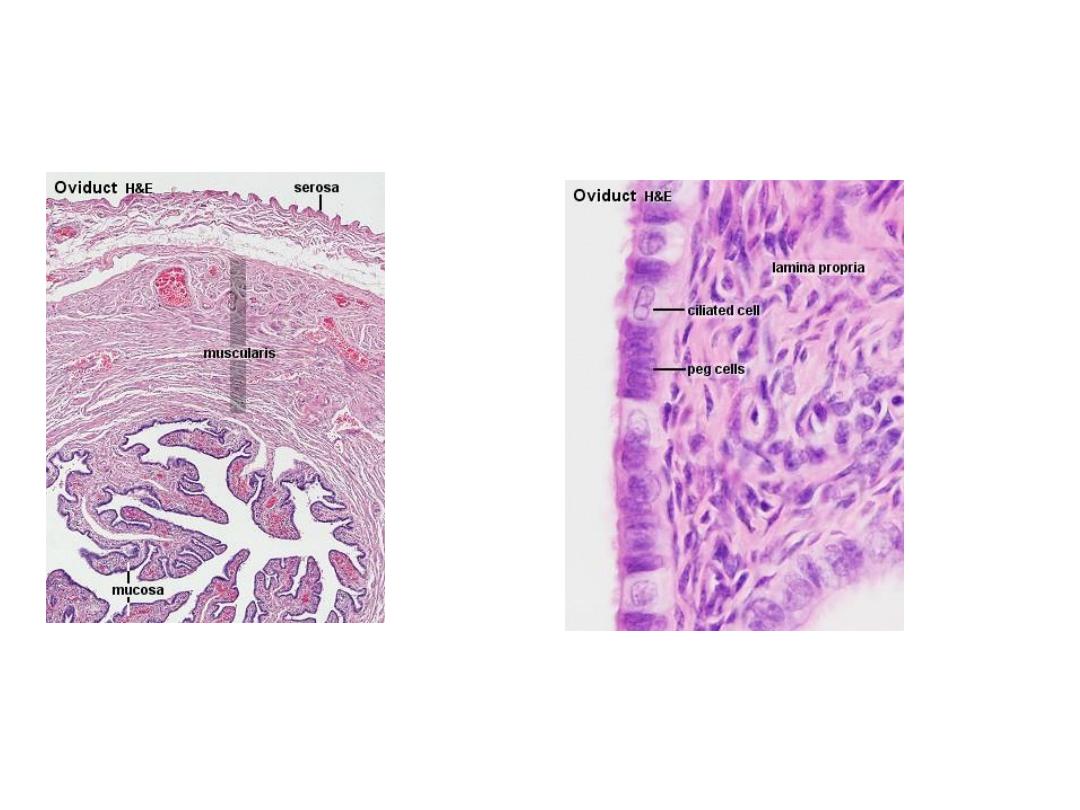
The Oviduct
The oviduct functions as a conduit for the oocyte, from the ovaries to the uterus.
Histologically, the oviduct consists of a mucosa and a muscularis. The peritoneal surface of
the oviduct is lined by a serosa and subjacent connective tissue.
The mucosa
is formed by a ciliated and secretory epithelium resting on a very cellular lamina propria. The
number of ciliated cells and secretory cells varies along the oviduct. Secretory activity varies
during the menstrual cycle, and resting secretory cells are also referred to as peg-cells. Some
of the secreted substances are thought to nourish the oocyte and the very early embryo.
The muscularis
consists of an inner circular muscle layer and an outer longitudinal layer. An inner
longitudinal layer is present in the isthmus and the intramural part of the oviduct. Peristaltic
muscle action seems to be more important for the transport of sperm and oocyte than the
action of the cilia.

four subdivisions of the oviduct
.
1-The infundibulum :
is the funnel-shaped (up to 10 mm in diameter) end of the oviduct.
Finger-like extensions of its margins, the fimbriae, are closely applied to the ovary. Ciliated
cells are frequent. Their cilia beat in the direction of
2-the ampulla of the oviduct
. Mucosal folds, or plicae, and secondary folds which arise from
the plicae divide the lumen of the ampulla into a very complex shape. Fertilization usually
takes place in the ampulla.
3-The isthmus :
is the narrowest portion (2-3 mm in diameter) of the parts of the oviduct
located in the peritoneal cavity. Mucosal folds are less complex and the muscularis is thick.
An inner, longitudinal layer of muscle is present in the isthmus and the
4-
intramural part of the oviduct:
which penetrates the wall of the uterus. The term
"intramural" should be familiar to you ..... The mucosa is smooth, and the inner diameter of
the duct is very small.
Obstruction of the oviduct as a consequence of
salpingitis
is one possible cause of infertility,
and alterations of luminal structure by inflammatory processes are a risk factor for tubal
pregnancies.

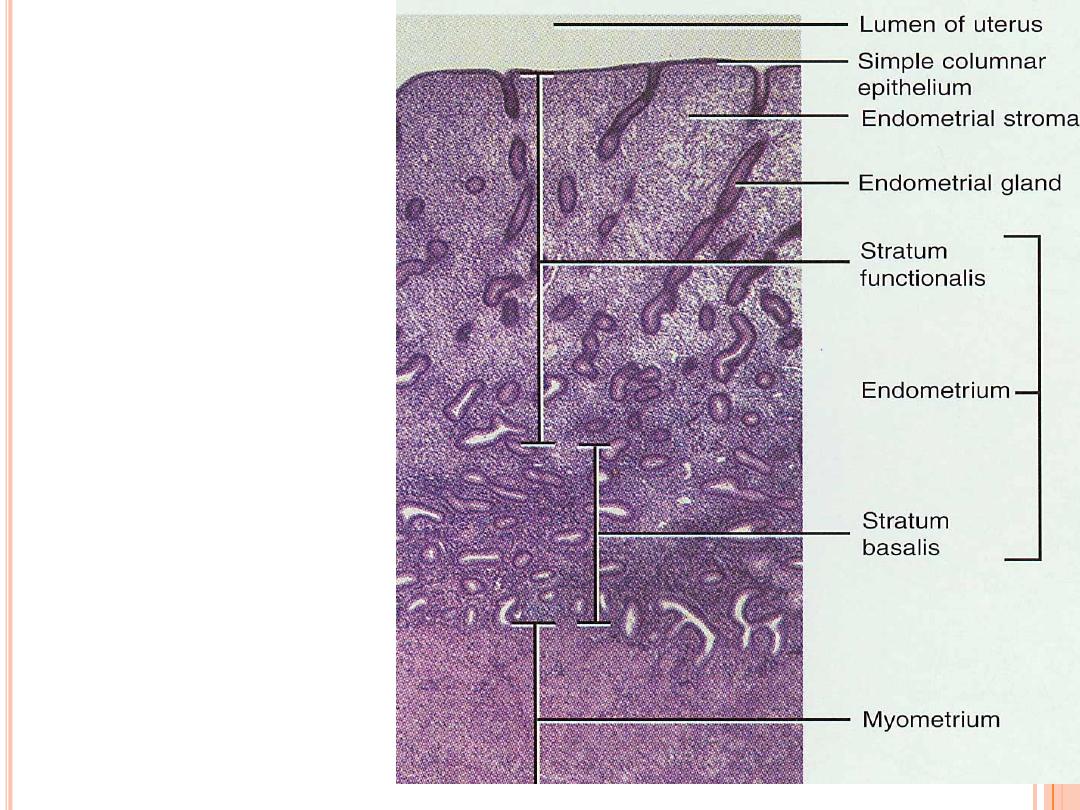
The Uterus
The uterus is divided into body (upper two-thirds) and cervix. The walls of the uterus are
composed of a mucosal layer, the endometrium, and a fibromuscular layer, the myometrium.
The peritoneal surface of the uterus is covered by a serosa.
Myometrium
The muscle fibres of the uterus form layers with preferred orientations of fibres (actually 4),
but this is very difficult to see in most preparations. The muscular tissue hypertrophies during
pregnancy, and GAP-junctions between cells become more frequent.
Endometrium
The endometrium consists of a simple columnar epithelium (ciliated cells and secretory cells)
and an underlying thick connective tissue stroma. The mucosa is invaginated to form many
simple tubular uterine glands. The glands extend through the entire thickness of the stroma.
The stromal cells of the endometrium are embedded in a network of reticular fibres. The
endometrium is subject to cyclic changes that result in menstruation.
Only the mucosa of the
body of the uterus takes part in the menstrual cycle.

The endometrium can be divided into two zones based on their involvement in the
changes during the menstrual cycle: the
basalis and the functionalis.
The
basalis
is not sloughed off during menstruation but functions as a regenerative
zone for the functionalis after its rejection.
The
functionalis
is the luminal part of the endometrium. It is sloughed off during
every menstruation and it is the site of cyclic changes in the endometrium. These
cyclic changes are divided into a number of phases: proliferative (or follicular),
secretory (or luteal), and menstrual
25
U
TERINE
H
ISTOLOGY
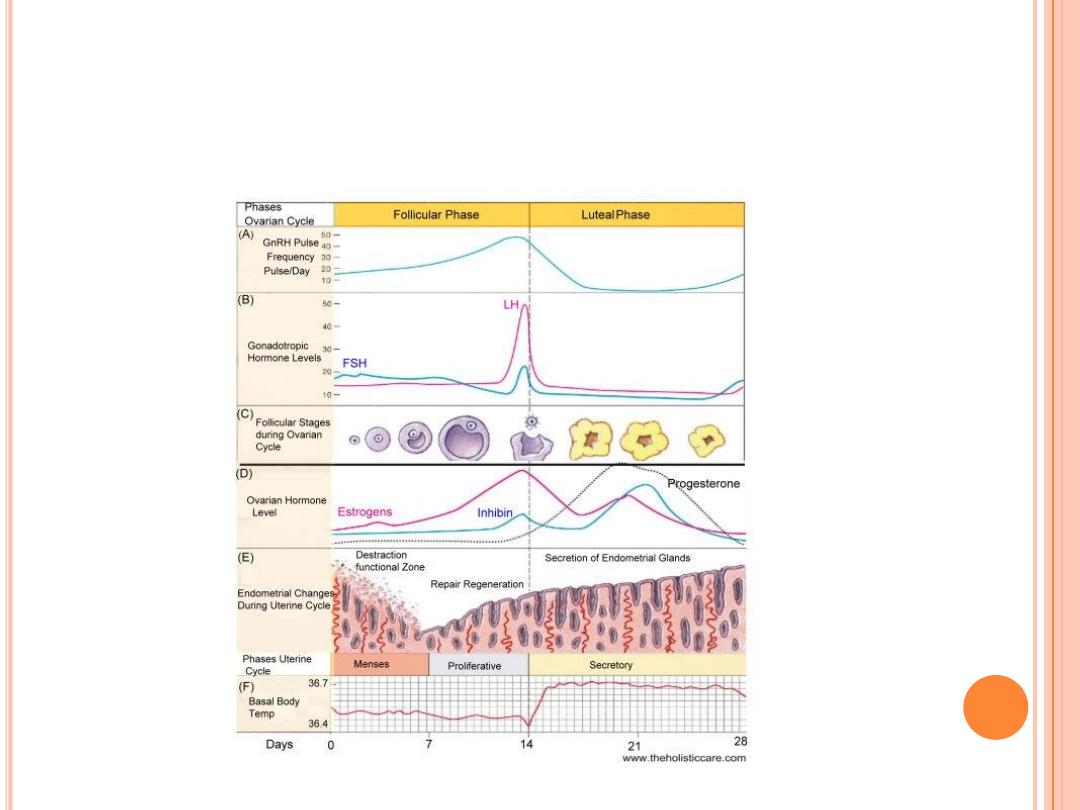
O
VARIAN AND
U
TERINE
C
YCLES

27
C
ERVIX
Narrow lower neck of the uterus
which projects into
the vagina inferiorly
Cervical canal
– cavity of the cervix that
communicates with:
The vagina via the
external os
The uterine body via the
internal os
Cervical glands secrete mucus that covers the
external os and blocks sperm entry except during
midcycle
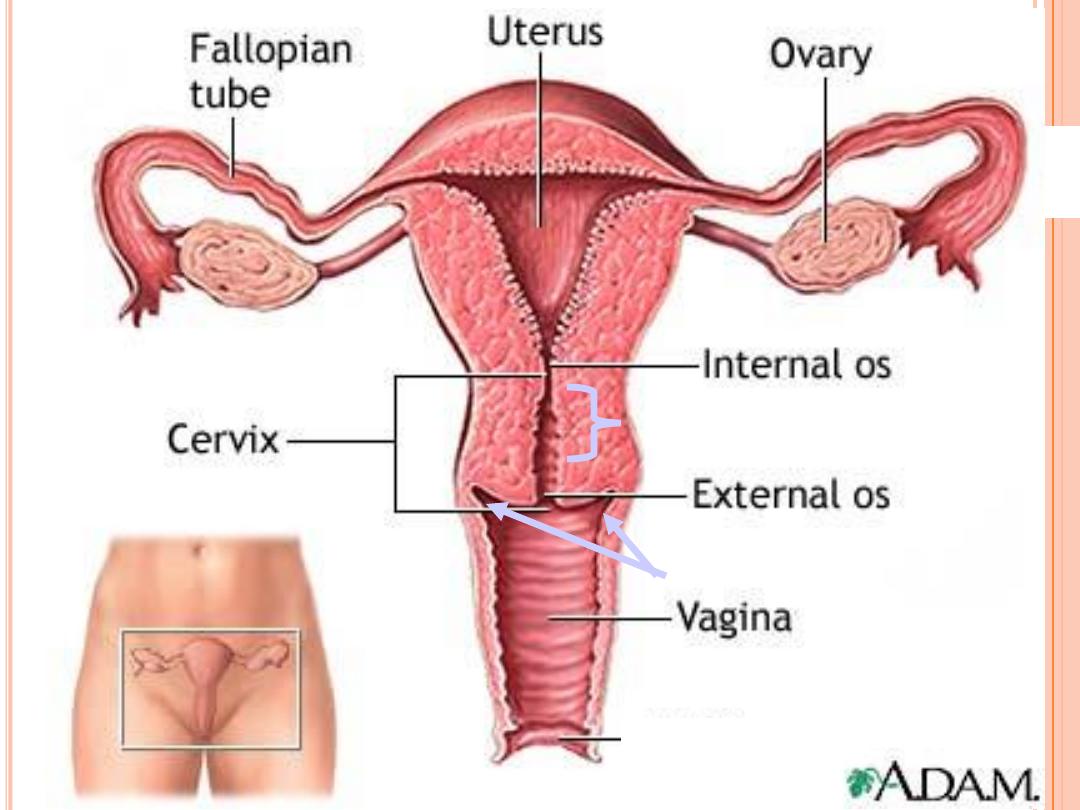
28
Fornix
Endocervical canal
Vagina
The vagina is a fibromuscular tube with a wall consisting of three layers: the mucosa,
muscularis and adventitia of the vagina
Mucosa
The stratified squamous epithelium (deep stratum basalis, intermediate stratum
spinosum, superficial layers of flat eosinophilic cells which do contain keratin but which do
not normally form a true horny layer) rests on a very cellular lamina propria (many
leukocytes). Towards the muscularis some vascular cavernous spaces may be seen (typical
erectile tissue).
Muscularis
Inner circular and outer longitudinal layers of smooth muscle are present. Inferiorly, the
striated, voluntary bulbospongiosus muscle forms a sphincter around the vagina.
Adventitia
The part of the adventitia bordering the muscularis is fairly dense and contains many
elastic fibres. Loose connective tissue with a prominent venous plexus forms the outer
part of the adventitia.
