Inflammatory cells
Neutrophiles & Monocytes
N & monocytes are closely related phagocytic L.What are the differences between them ???
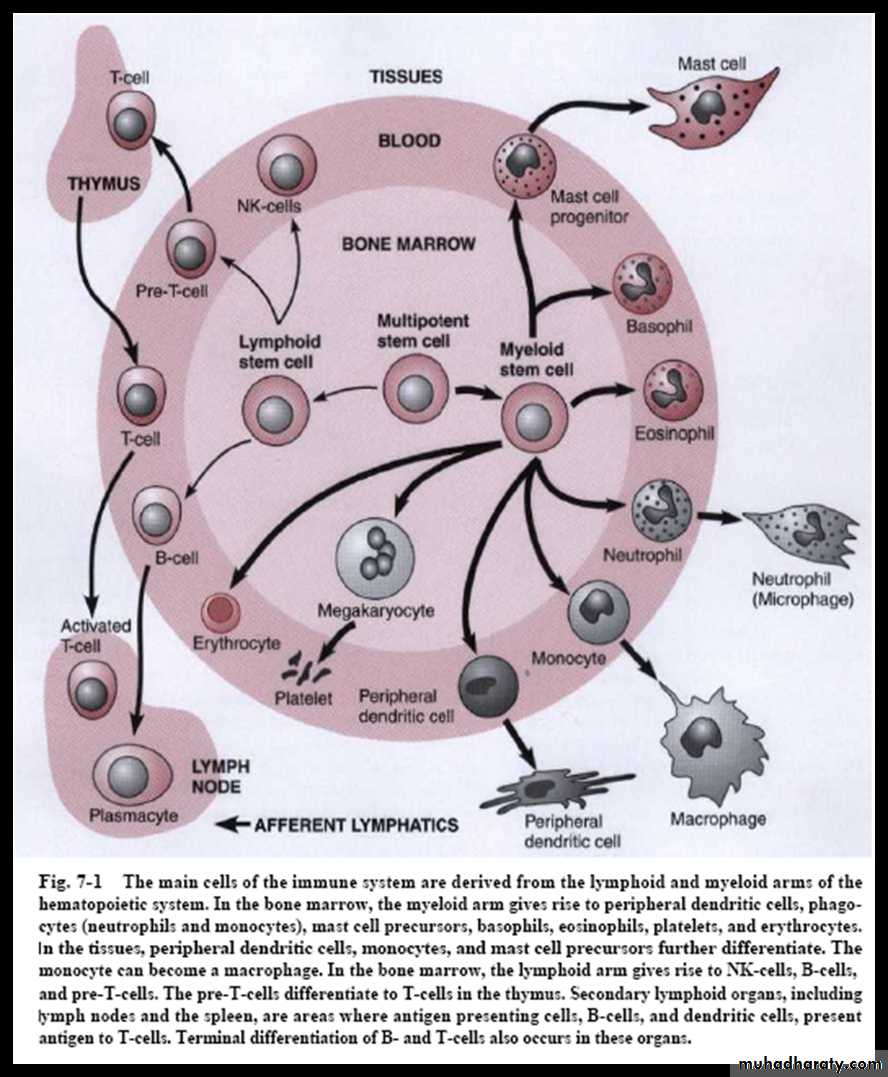
1. N almost completely differentiate within the bone marrow whereas M exit bone marrow in an immature form & differentiate in the tissues
2. N are the predominant inflammatory cells in blood (about 2/3), small size (microphages) & posses receptors for C. & IgG
3. M complete their differentiation in local tissues to become large in size (macrophages), live in tissues long enough to present Ag to T cells
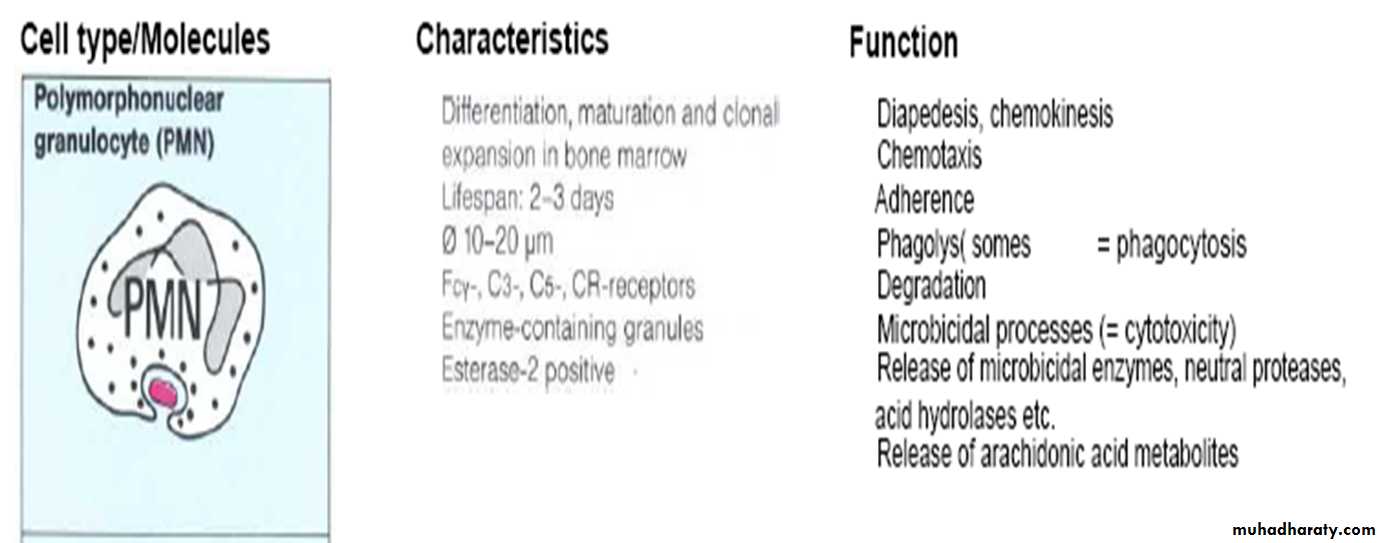
NEUTROPHILES (PNL,PMN,N )
• The most important inflammatory cellsContinuously migrate through PD tissues to G. fluid to be in contact with MO
N palisade on the surface of plaque to form barrier
Form in B.M. & stay in blood for 6h & in tissues for 4d.
Migration to tissue, margination , adherence, accumulation & penetration
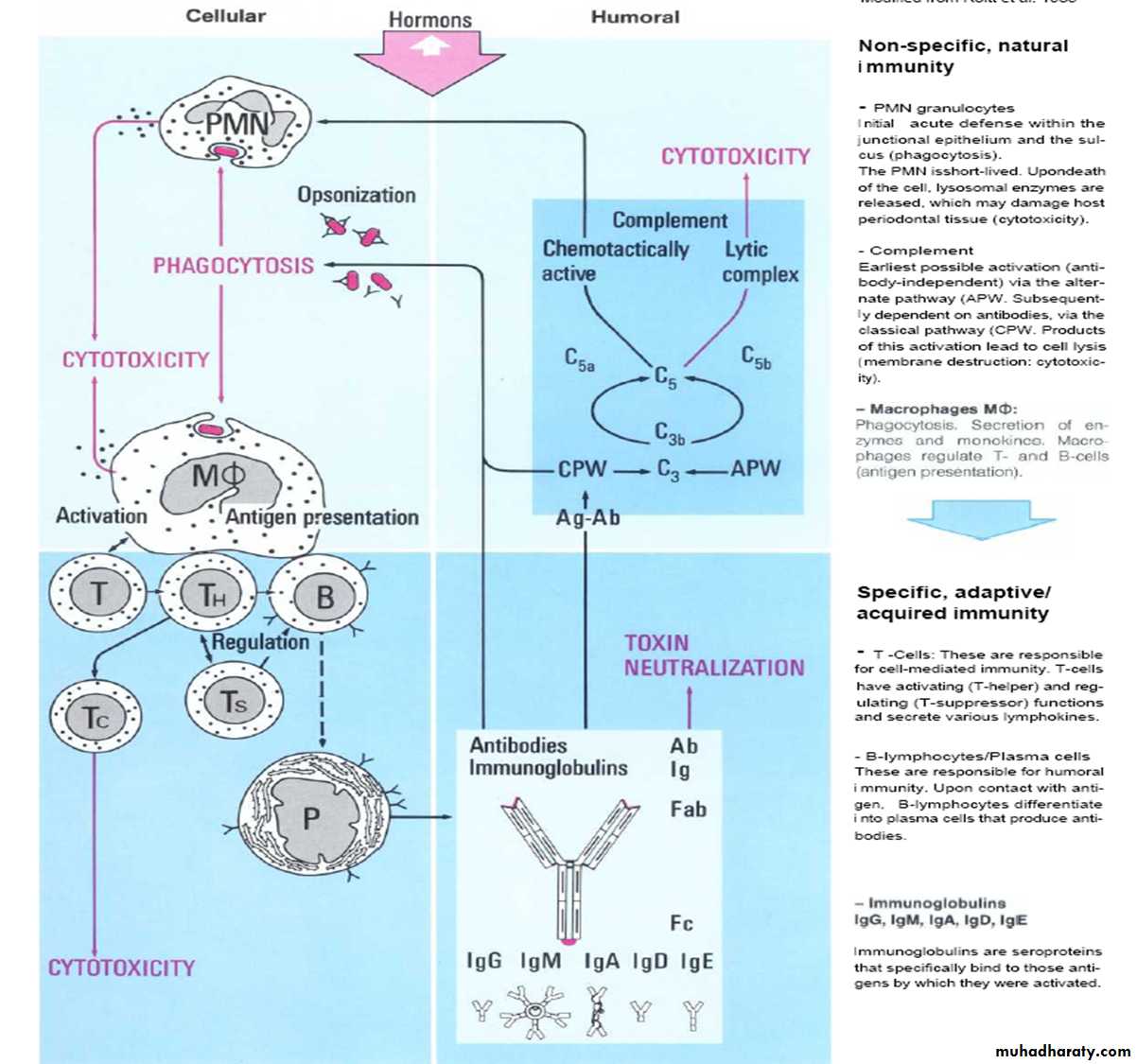
Respond to MO invasion through:
Chemotaxis
Phagocytosis
Microbiocidal activity
•
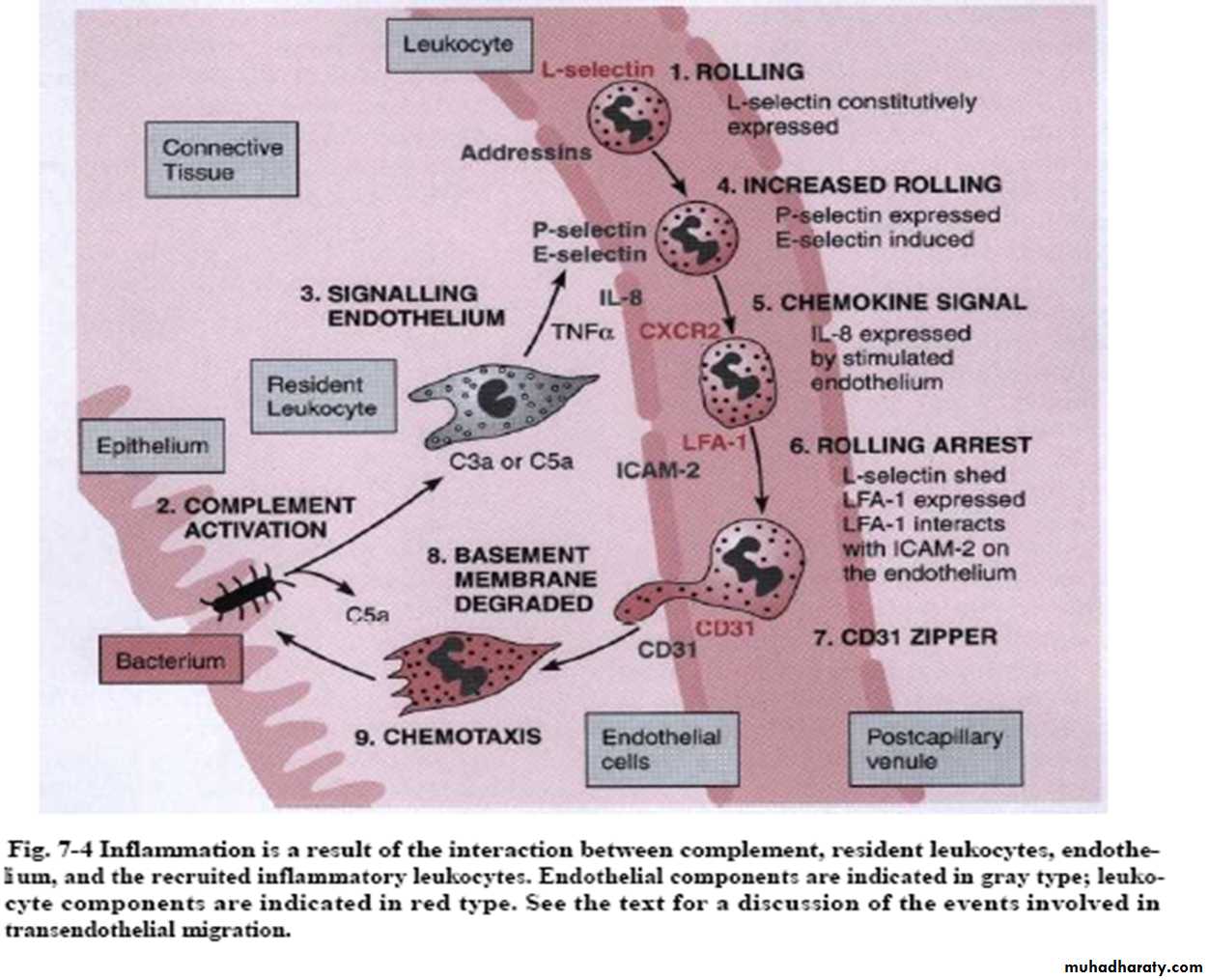
Trans-endothelial migration
Direct movement of L. from blood to local tissues by interaction between L. & endothelium that result in pushing L. between the endothelial cells to exit blood & enter tissueDefect in such process associated with some conditions such as Aggressive PD
N & M spend less than 12h in circulation, to exit and enter tissues
•
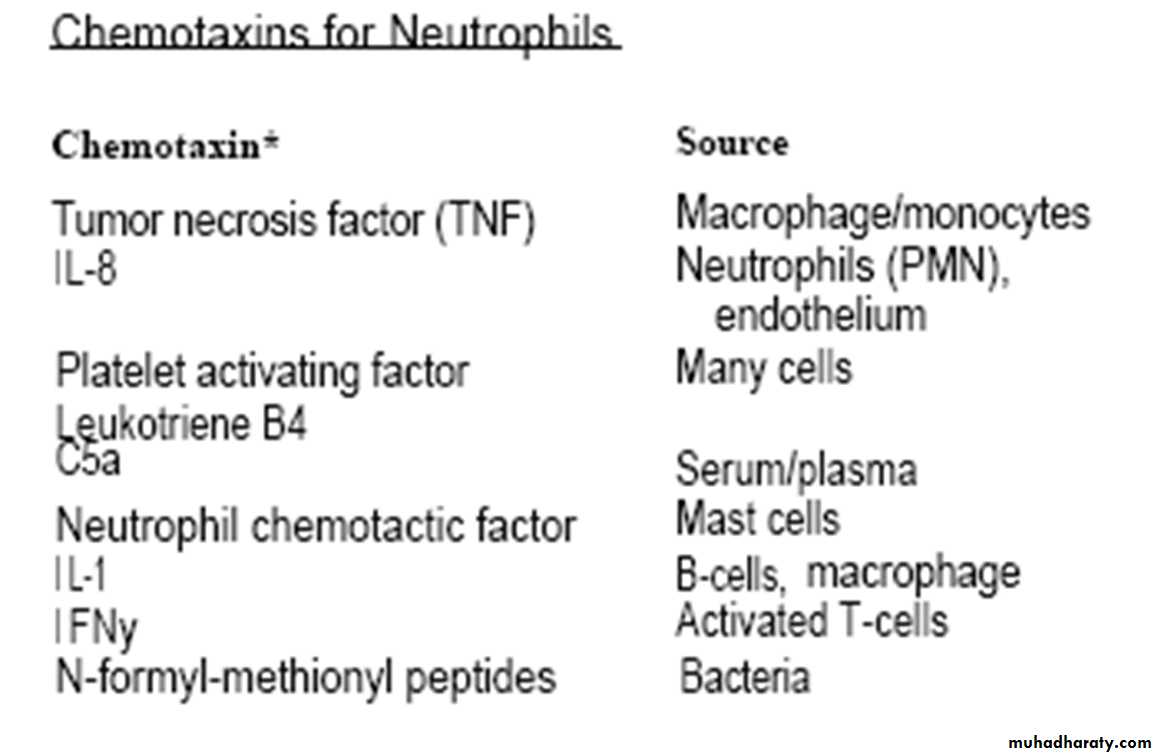
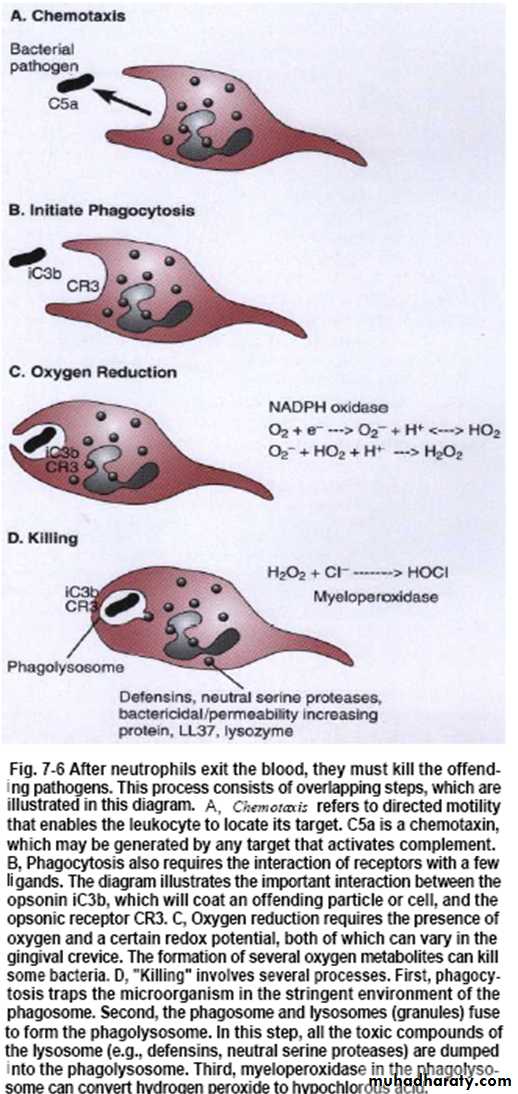
Chemotaxis
Trans-endothelial migration & migration of L. through tissue to the site of infection by the action of:• 1. Activated complements (C3a,C5a)
• 2. lymphokines
• 3. N.(leukotriene)
• 4. Kinin
• 5. Bacteria itself & their products
Cells (N, L) change from spherical shape with limited mobility to mobile, active & polarized
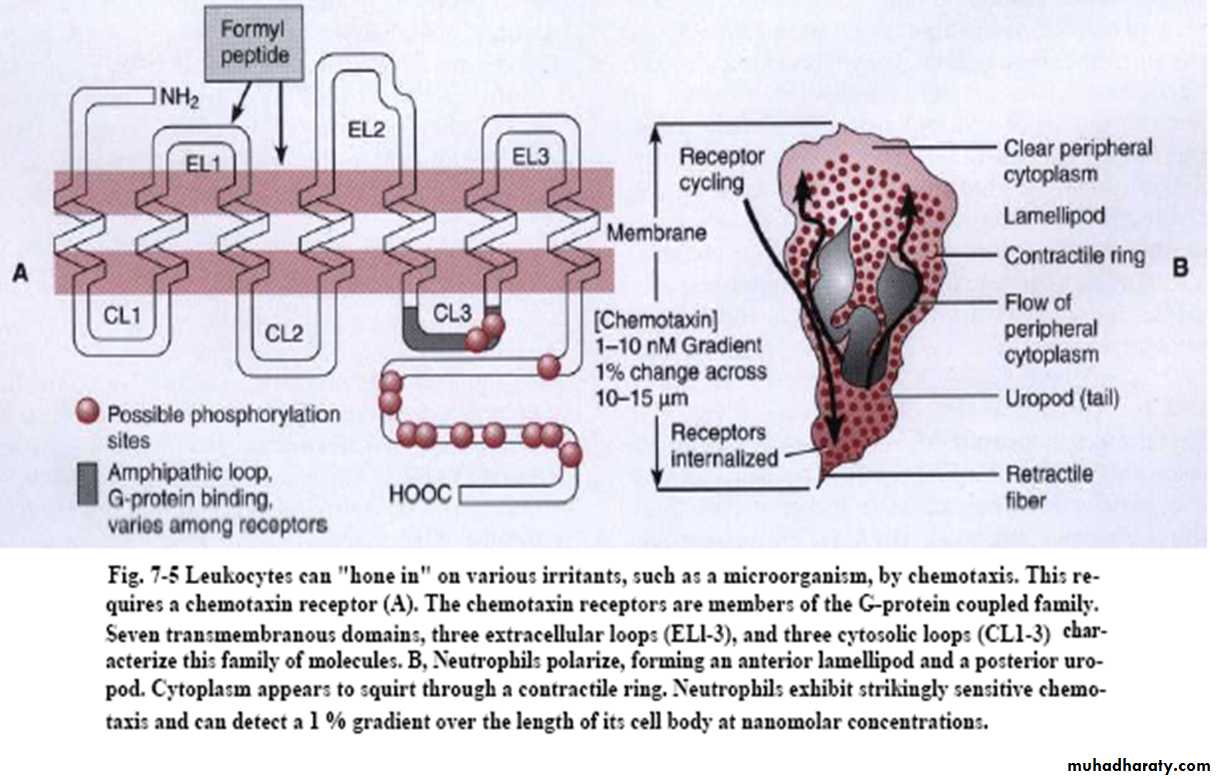
Chemotaxis
1st event is the detection of chemical stimulant by binding of chemotactic factor (chemotaxin) to specific receptor on N followed by polarization (reorganization of microfilament), occur due to change in permeability or membrane potentialIt depends on L. ability to sense a chemical gradient across its cell body & migrate in the direction of increasing concentration
Polarization of N
Phagocytosis
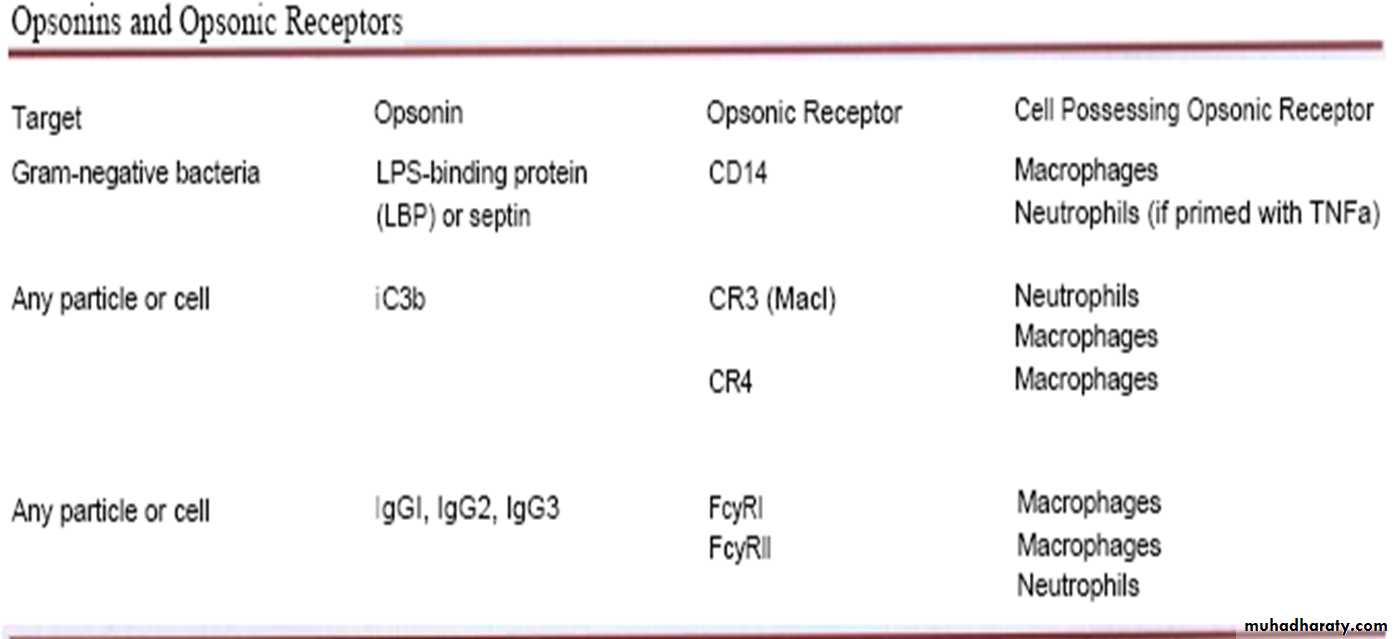
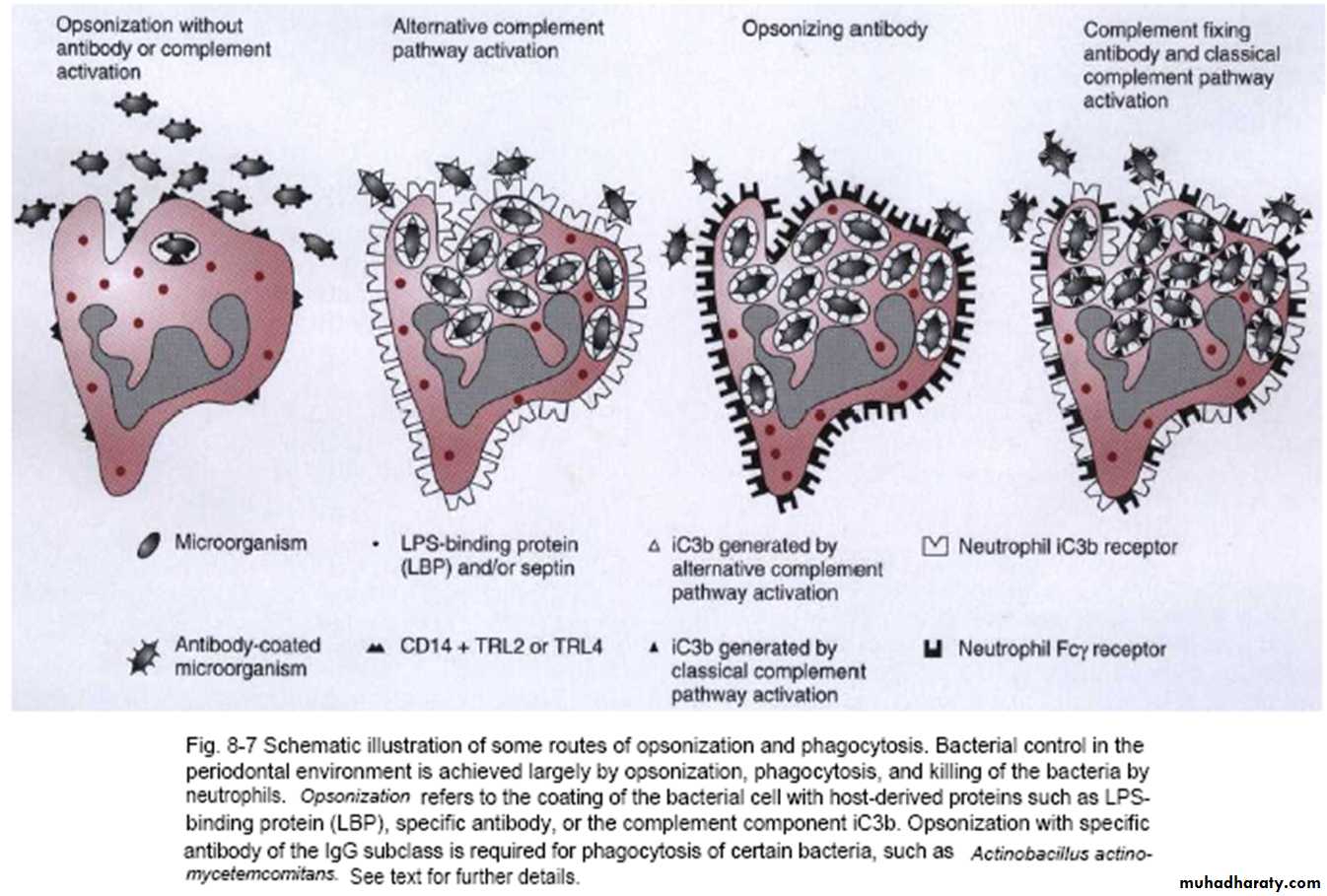
Recognition appear by contact of N with the bacterial surface & through action of IgG & C3b that bound with bact. sur. (opsonin)Opsonization, means coating the pathogen with a few recognizable ligands that enable phagocyte to bind to & ingest pathogen
N recognize opsonin then firm attach occur
Plasma membrane (of N) flows around & then invaginate to internalize attached bact. which is contained within phagosomes
Microbiocidal activity
Intracellular:• 1. O2 dependent (Myeloperoxidase)
• 2. O2 independent: Lysozyme, Lactoferrin, NP, Acidity (4-6 pH), Cationic proteins & peptides (e.g. bacterial permeability increasing protein)
• Lysosomes (granules): posses enzyme dependent bactericidal activity (as lysozymes or NP) & enzyme independent bactericidal activity (as myeloperoxidase)
• Lysosomes move to phagosome & fuse with it to form phagolysosome. In this step, all the toxic components of lysosome (as lysozymes or neutral proteases) are dumped into the phagolysosome
Extracellular: Enzymes escape to outside
•
Microbiocidal activity
Marked rise in O2 consumption if present as in subgingival area (usually there is no O2) indicates microbicidal activity; however, N can function under anaerobic condition• Also, marked rise in O2 consumption if present indicates O2 reduction to yield O2 radicals (toxic for MO especially anaerobic)
Increase in glycolysis & glucose utilization to provide energy required for phagocytosis & result in drop in the intracellular pH (increased acidity) due to formation of lactate
Microbiocidal activity
Lysosomes move to phagosome & fuse with it to form phagolysosomeO2 radicals and myeloperoxidase released into phagosome to kill bacteria
Before invagination is completed, some of products released from phagosome into external environment which will induce damage to the host tissue, so extracellular enzymes are those enzymes that escape to outside the cell
Non-oxidative path is very important in PD disease because of highly anaerobic conditions in subgingival environment
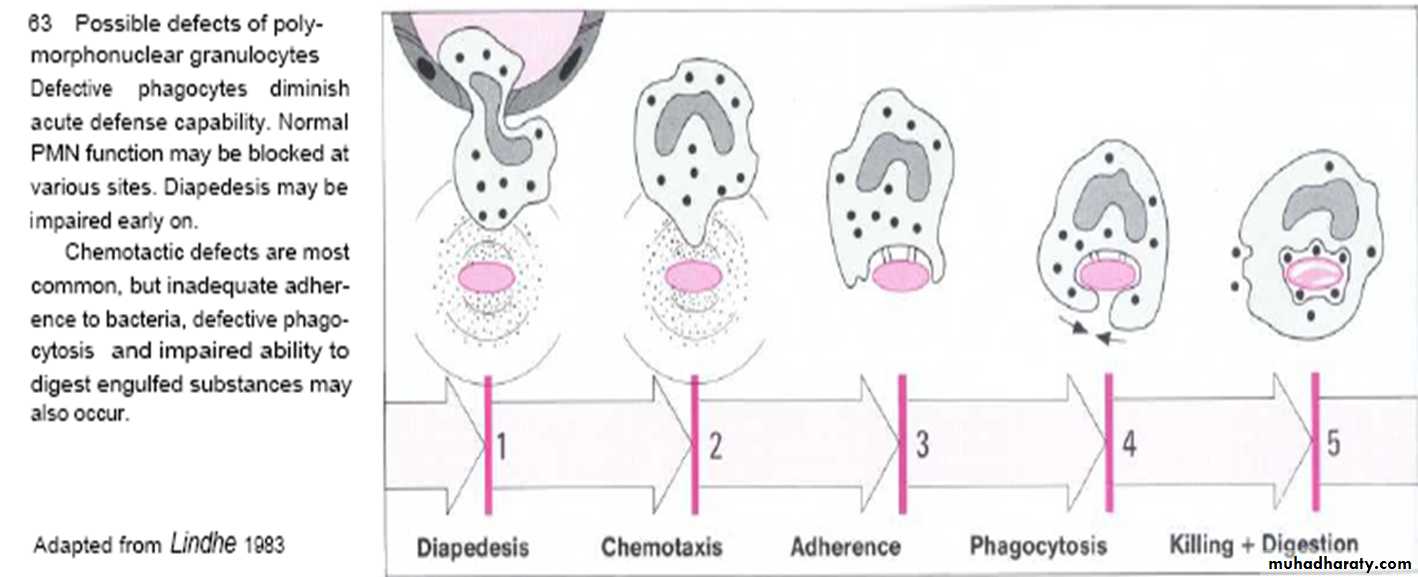
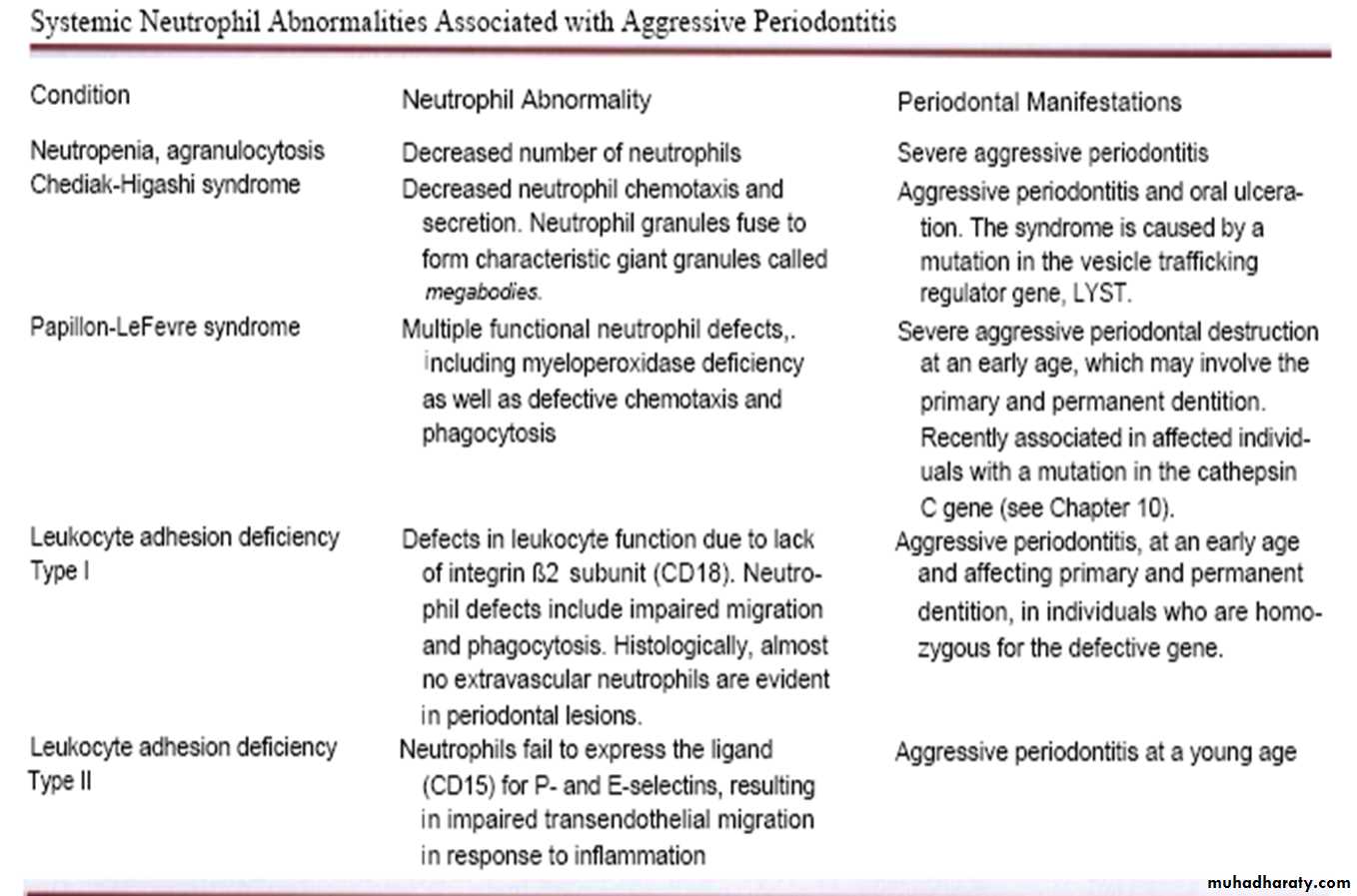
N dysfunction
Seen in:• 1)AIDS. 2) DM. 3) Liver disease. 4) Chédiak–Higashi syndrome. 5) Down syndrome. 6) Papillon–Lefèvre syndrome. 7) Ulcerative colitis. 8) Thalassemia. 9) Neutropenia (Agranulocytosis) 10) Aggressive periodontitis (AP)
• 75% of patients with AP & LAP have chemotactic defect of N (reduction in binding site) which is genetic in origin
• or environmental as G-ve MO
• 1-Block receptors.
• 2-Inhibit function by bacterial metabolites.
• 3-There is a genetic predisposition for such environmental factors.
• 4-Receptors degradation by proteases or O2 radicals.
• also Phagocytic defect by blocking C3b receptor. Its localized phenomenon as only diseased (PD tissue) sites affected by toxic & non-toxic factors from A.a.
•