Coll. Medicine \3rd stage
ParasitologyAssist. Prof. Dr. Amal KH. KH.
Lec. 2
Class (1) : Sarcodina (lobosea)
All the Amoeba have a trophozoite and cyst stages except Entamoeba gingivalis .No sexual reproduction has been demonstrated for any species of amoeba.
Pseudopoda is the mean of movement .
Simple life cycle that complete in a single host .
This class include the amoeba species of human which can be divide into two group based on the location of infection :
Intestinal species
Entamoeba histolytica
Entamoeba dispar
Entamoeba coli
Endolimax nana
Iodamoeba butschlii
Extra - Intestinal species
Entamoeba gingivalis (mouth)
Naegleria fowleri (brain)
Entamoeba histolytica :-
E. histolytica produces intestinal and extra – intestinal diseases . it is a leading cause of morbidity and mortality in developing countries . Entamoeba histolytica infect more than 10% of the world population. Amoebiasis can affect all age groups and both the sexes .
Morphology:-
Entamoeba histolytica exists as trophozoite , and cysts .
Trophozoite: the trophozoite range in size from 18-40 µm and do not have a definite shape . the trophozoite exhibit active unidirectional movement achieved with the help of broad ,hyaline , finger- like pseudopodia . their cytoplasm has an outer , clear ectoplasm and inner , granular endoplasm . The trophozoite of E. histolytica engulf red blood cell , bacteria , yeast and other debris . the presence of RBC in the cytoplasm is diagnostic of E. histolytica as it is the only intestinal amoeba to exhibit this characteristic .
The trophozoite contain a single , spherical nucleus . the nucleus has a delicate nuclear membrane . on the internal surface of the nuclear membrane there are minute granules known as chromatin dots . in the centre of the nucleus is a single dense karyosome or nucleolus . the nuclear pattern E. histolytica differentiates the parasite from other species of amoeba .
The trophozoite of E. histolytica live in the mucosal folds of the large intestine and divide by binary fission .they may invade the intestinal wall. Trophozoite when passed in faeces ,die on exposure to air .gastric acid also destroys them. Therefore, trophozoite can not transmit infection . thus , for transmission of infection and continuation of the species , E. histolytica has to change from a trophozoite to a cyst to enter a new host .
2- Cyst: The trophozoite of Entamoeba histolytica encyst themselves under condition like :
Overpopulation of amoeba .pH change.
Extreme change in the available food and oxygen .
Increased resistance developed by the host .
-Encystations of E. histolytica trophozoite:
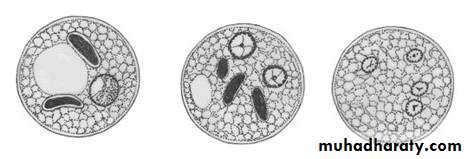
In the process of encystations , the trophozoite become non- motile , rounded and devoid of inclusion . this is precystic stage . the precysts stage are smaller than trophozoites and usually larger than cysts . they secrete a highly refractive cyst wall around themselves and become the cysts .The cyst of E. histolytica are spherical . depending upon the maturity of the cyst , they may contain one , two or four nuclei . the immature cysts have a single nucleus , , diffuse glycogen mass and sausage – shaped chromatoid bodies . the glycogen mass serves as a food reserve.
The cyst mature with two mitotic divisions of the nucleus to form binucleate and then quadrinucleate cysts . in this process the nuclear size is reduced and also the glycogen mass and the chromatoid bodies reduced in size and disappears . immature cyst if passed in the faeces can mature outside the human body . the mature cysts can survive in moist environment for 10 days. They withstand the gastric acid and therefore act as the infective forms . it is important to note that , the strength of chlorination used in purification of public water supply is insufficient to kill the cysts of Entamoeba histolytica . hence , boiling , filtration of water is necessary to prevent infection.
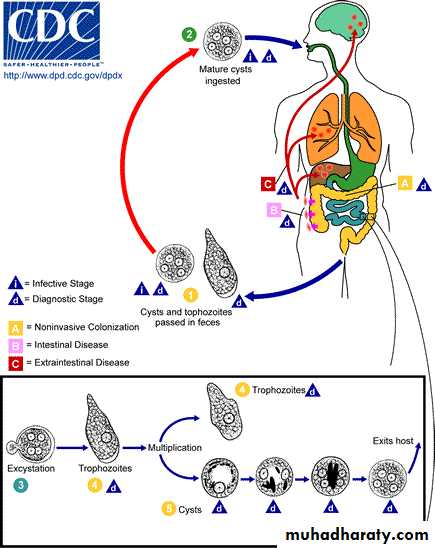
Life cycle: -
Entamoeba histolytica has a simple life cycle . the mature cysts are the infective forms of Entamoeba histolytica . they infect human through contaminated food or water . contamination of food and water with the cyst occur due to faeces ,flies or unwashed hands of food handlers . the cyst pass up to the ileo – caecal region ; the surrounding alkalinity and the damage caused by trypsin to the cyst wall during the transit leads to excystation in this region.A quadrinucleate metacyst emerge from a cyst . the metacyst rapidly divides to produce eight small amoebae (amoebulae or metacystic trophozoites ) these amoebule mature and develop into trophozoites . the trophozoite established themselves at areas of stasis in the large intestine . the static area in the glandular crypts of the colon (caecum ) provide the optimum habitat .
The trophozoites may live in the lumen without invading the intestinal mucosa (not have PGM) in about 90% of infected person . in such person the trophozoite feed on colonic contents and mucus . the trophozoite encyst them under the previous condition and pass in feces such this cyst passers act as carrier and are responsible for maintenance and spread of infection in the community .
In the remaining 10% of the infected person , amoeba invade the host tissue . invasion of bowel mucosa leads to dysentery . motile haematophagous trophozoite are frequently present in the fresh stool of these person . encystation dose not occur during the acute phase of dysentery but for the previous condition . such persons recovering from dysentery and passing cysts in feces are called convalescent carriers . the cyst of cyst passers and convalescent carriers continue the life cycle of E. histolytica.
Virulence factors of E. histolytica :
The trophozoite of E. histolytica can invade the intestinal wall . the are distinct invasive and non invasive strains of E. histolytica . these strains vary according to their zymodemes (isoenzyme patterns). Zymodemes are include 4 enzymes include : glucose phosphosphate isomerase , L-malate :NADP oxodoreductase , phosphoglucomutase (PGM), and hexokinase . PGM is more important for determine the virulence of E. histolytica. Electrophoresis of PGM can show one or more of the 4 bands: α, β, γ, and δ. Strain of E. histolytica show an absence of α band together with presence of β band are virulent or invasive . E. histolytica strains have 22 zymodemes , of these ,10 are invasive and 12 are non invasive . zymodeme status is a stable character and always indicate virulence . other character of virulence of E. histolytica include:enhanced erythrophagocytosis .
reduced surface charge.
Resistance for compliment mediated factors.
Greater cytopathic effect on cell monolayers .
Agglutination by concavalin-A.
Pathology of E. histolytica :
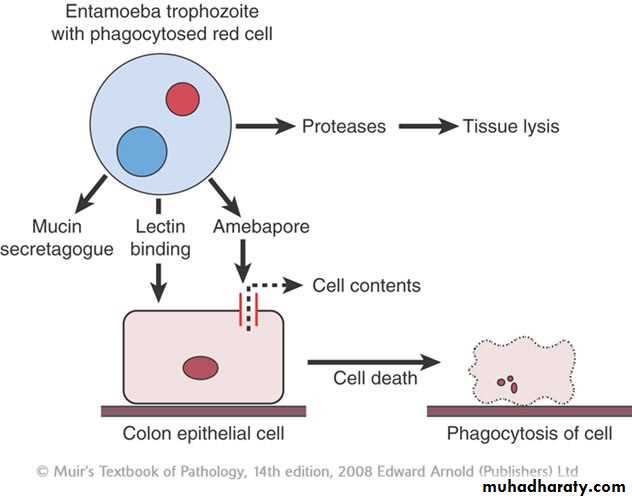
Trophozoites can invade tissue after penetrating through the intestinal mucosa . the cyst lack this ability . trophozoite can come in contact with colonic mucosa when colonic mucus is depleted. Trophozoites attach to interglandular epithelium by surface lectins present on the surface of Entameoba. these lectins attach to receptors on mucosal cells. On contact with these cells trophozoites release phospholipase-A and amoebopore (a pore forming complement – like protein ) this protein responsible for lysis of the cells. And Entameoba produce other enzymes like proteases that degrade collagen , elastin of extracellular matrix and disrupt glycoprotein bonds between mucosal epithelial cells in the gut. The trophozoite can lyse neutrophils , monocytes, lymphocytes and other cells .
Mechanism of invasion of intestinal tissue by trophozoite of E. histolytica
Invasion of the mucosa by E. histolytica leads to ulceration. In early stages of ulcers are pin- head sized with heaped up margins. They may progress to over one inch in diameter . the intervening mucosa between the ulcers appears normal. Submucosal extensions of ulceration under viable appearing surface mucosa causes the classic ' flask-shaped' ulcer. The invading trophozoites are present at the margins of dead and viable tissue. The superficial ulcers that have not penetrated the muscularis mucosae heal without scarring . occasionally , the deep ulcers may progress to a full – thickness necrosis leading to perforation . these ulcer occur in the colon . the ulcer can affect the entire length of colon . more often the ulcers affect the caecum or the segmoidorectal region of the colon.Rarely , there is an extensive formation of granulation tissue in a deep ulcer instead of the usual fibrotic tissue response . a mass formed in this way is an amoeboma . amoeboma frequently involves the right side of the colon . it looks similar to colon carcinoma .
The trophozoites can enter the damaged veins at the site of amoebic ulcers to reach liver through portal venous system . these invasive trophozoites are resistant complement mediated lysis. This property is critical for survival in blood and tissue. The trophozoites destroy the liver parenchyma with the battery of enzymes they have . the presence of amoebae in the liver initiates a protective acute neutrophilic response . paradoxically , the neutrophils are lysed on contact with the trophozoites . lysosomal enzymes released from these ruptured neutrophils contribute to the liver damage . necrotic materials replaced liver parenchyma to form amoebic liver abscess . a thin rim of congested liver tissue surrounds the abscess . the necrotic content of a liver abscess are classically described as ' anchovy –sauce pus ' . it is chocolate brown , although the color can be variable . the trophozoite are present in the peripheral rim . it is important to note that E. histolytica cysts are absent in amoebic liver abscess , these cysts are also absent in other extra- intestinal amoebic lesions. Amoebic peritonitis is the most frequent complication of amoebic liver abscess . it is usually results from the rupture of left lobe abscesses . pleuro – pulmonary amoebiasis is another complication of amoebic liver abscess . it usually results due to rupture of the liver abscess through the diaphragm into the pleural space. Other extra – intestinal complications amoebiasis with brain abscess and genitor-urinary amoebiasis are rare cutanous amoebiasis follow direct extension around the anus , colostomy site or sinuses from liver abscess .
Clinical features :-
Clinical conditions associated with the E. histolytica infection are :Intestinal :
Non- invasive :
asymptomatic
symptomatic
Invasive :
acute dysenteryfulminant colitis
toxic megacolon
chronic colitis
amoeboma
perianal ulceration
Extra – intestinal :
liver abscess.
Lung abscess .
Brain abscess.
Genitor – urinary disease.
Asymptomatic non- invasive intestinal infection by E. histolytica is the most common event. Excretion of E. histolytica cysts characterizes it . non – invasive intestinal infection may manifest as non – specific intestinal symptoms like increase frequency of bowel movement and abdominal pain . if not treated , the above mentioned condition resolve spontaneously in 8 to 12 months .
Amoebic colitis present as dysentery . the patient present with abdominal pain and tenderness . patient may have blood and mucus in faeces . the frequency passage of stool is 6 to 8 per day . only one third of patient are febrile .
Laboratory diagnosis:
Stool examination is the most important test to establish the diagnosis of amoebic dysentery . demonstration of the trophozoites clinches the diagnosis . the trophozoites , being delicate , die on exposure to air , water and temperature change . therefore , early examination of stool is necessary . in saline preparation trophozoites show active uni- directional – motility . the trophozoite are haematophagous (that is , they ingest RBC ) . cyst also represent the diagnostic stage of E. histolytica which can be found during stool examination .
Treatment :
In the treatment of amoebiasis , imidazole drug as metronidazole , tinidazole and cornidazole (750mg tid for 10 days ).
Prevention :
Proper disposal of sewage .
Human stool should not be used as fertilizer.
Good personal hygiene .
Washing of raw vegetable and fruits before consumption and protection of food from flies and cockroaches .
Quadrinucleate cyst is resistant to routine chlorination therefore drinking water should be purified by either boiling , filtration or iodination.