Coll. Medicine \3rd stage
ParasitologyAssist. Prof. Dr. Amal KH. KH.
Lec.4
Species of TrichomonasThese flagellates have the following common characteristic in their trophozoite stage :
a rounded anterior and a somewhat pointed posterior end .
a semi- rigid translucent rod-like axostyle which arises near the median anterior pole and extends through the entire body .
a small cytostome on one side of the anterior end .
3 to 5 free flagella arise from the anterior end and an additional marginal flagellum on an undulating membrane , which spirals down the sides of the body .
Multiplication is by longitudinal binary fission.
Trophozoites are described only for those species that parasitize man.
Three distinct species of Trichomonas are adapted to the human host . The species which occur in man are: T. hominis, T. tenax and T. vaginalis. Although they closely resemble one another they are morphologically different, develop in different locations and are reciprocally not transplantable.
Trichomonas hominis:-
Trichomonas hominis has a cosmopolitan distribution. It inhabit the lumen of the caecum .Trichomonas tenax:-
Trichomonas tenax is probably a cosmopolitan parasite of man . On the average Trichomonas tenax is smaller than T. hominis. The normal habitat is the mouth, particularly in diseased gums, in tartar around the teeth and in carious teeth. It is not pathogenic but its presence indicates poor oral hygiene.
Trichomonas vaginalis :
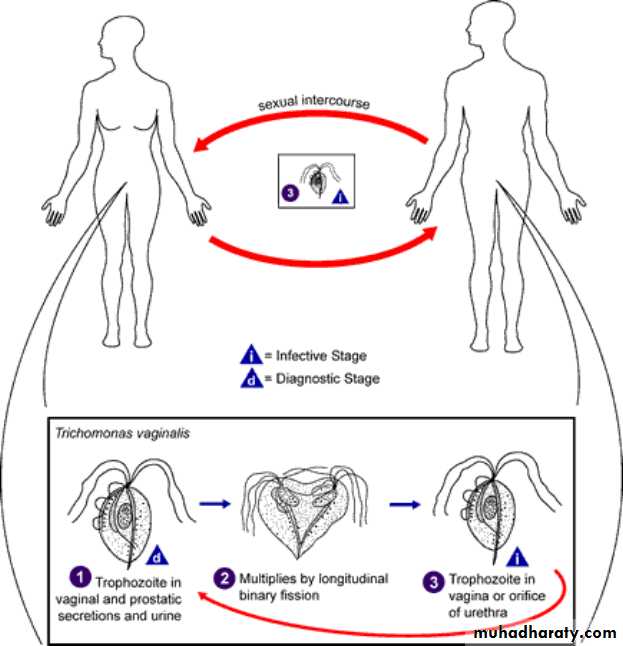
Trichomonas vaginalis, a flagellate, is the most common pathogenic protozoan of humans in industrialized and developing countries. It causes trichomoniasis. The infection is transmitted sexually (STD) .
Morphology :
Trichomonas vaginalis only exists in trophozoite stage and multiplies by longitudinal binary fission. Cystic stage is absent. Trophozoite inhabit the vagina in female, the prostate and seminal vesicles in male and urethra in both sexes. The trophozoites of Trichomonas, measuring 14-17μm×5-15μm have a single nucleus and a large sausage – shaped parabasal body, four anterior flagella and a single lateral flagellum attached to pellicle to form an undulating membrane . They are actively motile, pear-shaped. The inner margin of this membrane is supported by a filament. There is also a central skeletal rod or axostyle. The cytoplasm contains a large numbers of hydrogenosomes and sometimes viral particles. Trophozoite of Trichomonas vaginalis is facultative anaerobic. It is identified by its characteristic twitching motility. Trophozoite is the infective form of the parasite.
Life cycle :
Life cycle of Trichomonas vaginalis is simple. It is completed in a single host either male or female Trichomonas vaginalis resides in the female lower genital tract and the male urethra and prostate, where it replicates by binary fission. The parasite does not appear to have a cyst form, and does not survive well in the external environment. Trichomonas vaginalis is transmitted among humans, its only known host, primarily by sexual intercourse.
Transmission of T. vaginalis :
Trichomoniasis probably is the most common sexually transmit disease (STD) worldwide. Infected women harbouring T. vaginalis in the genital tract and infected men are the chief reservoir of infection. Trophozoite is the infective stage The infection may be transmitted venereally by sexual contact with infected person, also to babies during passage through an infected birth canal, and occasionally non-venereally through fomites such as towels, toilet seats, etc., and also through mud and water bath as well.Pathology & clinical features :
Trichomonas vaginalis infection in the male is often asymptomatic although at times it is associated with urethritis . In the female the propagation of this organism in the vagina may be symptomless , it may produce a characteristic type of vaginitis or it may be complicated by bacterial, fungous or spirochetal infection. There is definite evidence that time at Trichomonas vaginalis is at least an important contributor to a distance type of vaginitis characterized by leucorrhea , pruritus vaginae and vulvae , burning of the vagina and vulva or dysuria, and chafing of the vulva . The ph of the vaginal discharge in these symptomatic infections is typically alkaline as distinguished from the slightly acid condition of the normal vagina. The symptoms vary from mild to almost intolerable pruritus but the disease is more annoying than disabling .
DIAGNOSIS
The specific diagnosis of trichomoniasis is made by demonstration of organisms (a jerky motile trophozoites) in the genital specimens and also in the urine by microscopy. Microscopic examination of wet mounts may establish the diagnosis by detecting actively motile organisms. This is the most practical and rapid method of diagnosis (allowing immediate treatment). women, examination should be performed on highly vaginal swab (HVS) and urethral secretions. In men, anterior urethral or prostatic secretions should be examined. PCR also useful .
Treatment
Treatment should be implemented under medical supervision, and should include all sexual partners of the infected persons. The drug of choice for treatment is metronidazole therapy is usually highly successful. Tinidazole, which is a better-tolerated alternative drug.
Preventive measures
1) Detection and treatment of cases either male or female.
2) Avoidance of sexual contact with infected partners, and
3) Use of condoms.
Hemoflagellates :
Medically important Haemoflagellates require two hosts to complete their life cycle and are therefore called heteroxenous. They live in the blood and tissues of human and other vertebrate hosts, and in the gut of insect vectors.
Haemoflagellates infecting human belong to two genera, in the family, Trypanosomatidae— Trypanosoma and Leishmania. Members of this family have a nucleus, a kinetoplast and a single flagellum. The kinetoplast (sometimes referred to incorrectly as the micronucleus) consists of a deeply staining parabasal body and a adjacent dot-like blepharoplast. The blepharoplast and parabasal body are connected by one or more delicate fibrils. The flagellum arises from the blepharoplast. The portion of the flagellum which is inside the body of the parasite is called the axoneme.
Fig :Basic morphology of haemoflagellates. (1) Nucleus, (2) Karyosome, (3)
Parabasal body, (4) Blepharoplast, (5) Axoneme, (6) Undulating membrane, (7) Flagellum, (8)Multiplication in vertebrate and in vertebrate hosts is by binary fission. No sexual cycle is known.
Haemoflagellates exist in two or more of four morphological stages. These were formerly called the leishmanial, leptomonad, crithidial and trypanosomal stages. But as the above names have also been given to different genera within the family, it led to confusion. The names of the morphological forms have, therefore, been changed as described below .
Amastigote (formerly leishmanial) stage is rounded or ovoid without any external flagellum. The nucleus. kinetoplast and axial filament can be seen. This is the stage in which T. cruzi and Leishmania are found intracellularly in vertebrate hosts.
Promastigote (formerly called leptomonad) stage is lanceolate. The kinetoplast is anterior to the nucleus , near the anterior end of the cell, Parabasal body and blepharoplast together constitute the kinetoplast from which emerges the flagellum. There is no undulating membrane. This is the infective stage of Leishmania found in the midgut and proboscis of the insect vector. This is also the form in which Leishmania occur in cultures in vitro.
Epimastigote (formerly called crithidial) stage is more elongated, with the kinetoplast placed more posteriorly though close to and in front of the nucleus The flagellum runs alongside the body as a short undulating membrane before emerging from the anterior end. This is the stage in which T.gambiense and T. rhodesiense occur in the salivary glands of the vector testes fly, and T.cruzi in the midgut of the vector reduviid bug. This stage is lacking in leishmania.
Trypomastigote (formerly called trypanosomal) stage is elongated, spindle shaped with a central nucleus and the kinetoplast posterior to the nucleus situated at the posterior end of the body. The flagellum runs alongside the entire length of the cell to form a long undulating membrane before emerging from the anterior end. This is the infective stage of trypanosomes found in the vector arthropod and the stage found in the blood of the infected vertebrate. This stage is lacking in Leishmania.
Leishmania :
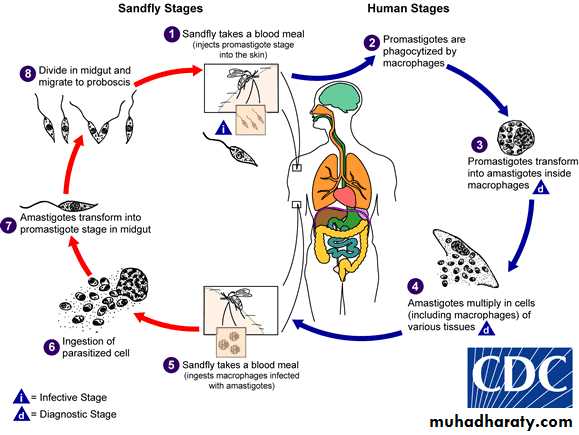
The genus Leishmania is named after Sir William Leishman who discovered the flagellate protozoon causing kala-azar, the Indian visceral leishmaniasis. All members of the genus Leishmania are obligate intracellular parasites that pass their life cycle in two hosts, the mammalian host and the insect vector, female sandfly. In human and other mammalian hosts, they multiply within macrophages, in which they occur exclusively in the amastigote form, having an ovoid body containing a nucleus and kinetoplast. In the sandfly, they occur in the promastigote form, with a spindle shaped body and a single flagellum arising from the anterior end.FIG: Morphology of Leishmania spp. a. Amastigote (LD body). b. Promastigote. 1. Nucleus 2. Parabasal body 3. Blepharoplast 4. Vacuole 5. Axoneme 6. Flagellum
Life cycle :
The life cycle is complex . two hosts are essential to complete their life cycle . leishmaniasis is a zoonotic infection . human and other vertebrates act as vertebrate host . sandfly of genus Phlebotomus (Ph. argentipes for L. donovani , Ph. papatasie for L. tropica) and Lutzomyia (for L. braziliences) . act as invertebrate host . The infective forms for human are the promastigotes . they are introduced in the tissue by the bite of an infected sandfly. They enter macrophages , lose their flagella and transform into amastigotes . amastigotes are obligate intracellular forms. Amastigotes multiply by binary division to reach numerous number in the macrophages ; this distends and ruptures the macrophages . liberated amastigotes enter other macrophages . few amastigote found in the peripheral blood . they are also present in monocytes. Amastigotes is the exit forms . The female sandfly needs a blood meal to lays eggs . when it feed on infected person , the amastigotes present in the peripheral blood and tissue fluid are sucked in. amastigotes reach the midgut of the sandfly , where they elongate and develop into promastigotes. The promastigotes multiply by binary division . they migrates to pharynx and buccal cavity in large numbers . the mature promastigotes block these passages . during the next blood meal of the sandfly , mature promastigotes ready to infect new host . the life cycle is thus completed.Routes of transmission :
The parasite is wide spread throughout the world. transmission takes place by the bite of sand flies. The infection sources are wild animals. Promastigote is the infective form. The infection is transmitted mainly by the bite of vector sandfly, rarely, by blood transfusion or accidental inoculation by cultured promastigores in the laboratory workers, or congenital infection, and sexual coitus.Dog-to-human transmission : The infection sources is domestic dogs; Most of patients are children , usually under 10 years old.
Leishmaania tropica :
Leishmania produce Cutaneous leishmaniases. cutaneous leishmaniasis (oriental sore) also called Delhi boil, Baghdad boil, Aleppo boil, is produced by Leishamnias belonging to Leishmania tropica complex. There are 2 serologically and biochemically distinct species of L. tropica complex:-1- L. tropica minor
2- L. tropica major
Pathology :
Cutaneous leishmaniasis include the following steps (see the diagram):Formation core of cells parasitized by amastigotes and remains localized to skin .
Acanthosis of this core by cellular infiltration which is also remain localized to skin .
Formation of Ulcer with sharp cut edges and surrounding indurations .
Granulation by infiltration of fibroblast, then healing occur within 2-12 months with depressed pigmented scar or leishmanoma.
Leishmanoma : a primary cutaneous lesion manifests as a nodule in the skin, which measures 2.5 to 4cm. This is not seen in kala-azar.
Comparison between L. tropica minor and L. tropica major
1- L. tropica minor: (causes dry sore or urban cutaneous leishmaniasis).
Produce chronic disease that if not treated, lasts for year or longer.
with 2month – 3year incubation period
It is characterized by the production of dry lesions that ulcerate only after several months .
The lesions occur primarily on the face.
The lesions are dry and non ulcerated.
It is found in urban areas, it is found in Iraq and around the Mediterranean basin and in Asia Minor, Afghanistan, India and Kenya.
The dog may be a natural host.
2. L. tropica major: (causes wet sore or rural cutaneous leishmaniasis).
Produces an acute infection with duration of 3-6 months.
With as little as 2 weeks incubation period.
The lesions occur primarily on the lower limb.
The lesions are moist and tend to ulcerate very early.
There may be secondary or satellite lesions.
L. major occurs in Asia Minor, Middle East (Iran, Syria, Palestine and Jordan) and in north and middle Africa.
It is primarily a disease of rural areas.
Reservoir hosts (Rodents) are important source of human infection.
Diagnosis
Usually made in endemic areas on clinical groundsMicroscopic detection of amastigotes (L.D. bodies) within large monocytic cells in Giemsa stained smear obtained by aspiration of fluid from beneath the ulcer bed, especially its active borders. Scraping taken from the ulcer surface do not reveal the organisms, which are destroyed in areas secondarily infected with bacteria.
Treatment
1- Sodium stibogluconate (Pentostam)2- Pentamidine (isothionate)
Visceral leishmaniasis :
Leishmania donovani was reported by Leishman and Donovan independently in eplenic smear of patient with kala azar . kala azar is also known as vesiral leishmaniasis . it is endemic disease in many part of the world. LD bodies multiply by binary division . Amastigotes subsequently invade throughout the reticuloendothelial system of the spleen, liver, bone marrow and lymph nodes and multiply in large numbers.It is also known as kala azar, is the most severe form of the disease, which, if untreated, has a mortality rate of almost 100%. It is characterized by irregular bouts of fever, substantial weight loss, swelling of the spleen and liver, and anaemia. The incubation period of visceral leishmaniasis is generally about 3 months.
Fever : is the first symptom to appear. Typically, it is nocturnal or remittent with a twice-daily temperature spikes. Sweating with chills but seldom rigor, accompanies the temperature spikes, less commonly, fever is continuous. Diarrhea and cough are frequently present.
Pathological changes in organs:
Spleen : Spleen is grossly enlarge, surrounded by a thick capsule. It is soft and non-tender. The splenic pulp is greatly increased, congested and turns purple or brown black and becomes highly friable. Splenic cells are densely packed with amastigotes of L. donovani.
Liver : Liver is enlarged with a sharp edge, soft consistency and smooth surface. The Kupffer cells are largely increased both in their size and number. They are filled with amastigotes. In contrast, hepatocytes do not contain any parasites. Atrophic areas, swelling and also fatty degeneration often are seen in the liver cells.
Bone marrow : It is dark red in colour and shows extensive proliferation of reticuloendothelial cells. Haemopoetic tissue of the bone marrow are replaced by large numbers of parasitised macrophages. Plasma cells often are increased in number.
Lymph nodes : Lymph nodes are enlarged. amastigotes are demonstrated in the enlarged lymph nodes.
Kidney :Kidney shows cloudy swelling and is invaded with macrophages parasitized by amastigotes.
Heart : It is pale but does not show any amastigotes in the myocardium .
Haematological changes occur. Typically:
anaemia is present in kala-azar. It is normocytic and normochromic. Anaemia is multifactoral . It is caused by increased haemolysis, haemorrhage, haemodilution, replacement of bone marrow with parasitised macrophages and splenic sequestration of red cells.
Leucopenia is well-marked. White blood cell count falls down to as low as 1100/mm3 of blood. Thrombocytopenia is caused by destruction of platelets .
Post kala-azar dermal leishmaniasis (PKDL) or black fever : It is a non-ulcerative lesion of the skin, The condition is characterised by a spectrum of lesions in the skin ranging from depigmented macules to wart-like nodules over the face and exposed surfaces of limbs.
As the disease progresses, the skin becomes dry, thin and scaly. The hairs become dull, thin and are lost. The nails become brittle. The skin on the hands, feet, abdomen and around the mouth and fore-head becomes grayish and dark coloured. This hypo pigmentation of the skill characteristically is seen in Indian patients giving tile name kala-azar, which means black fever. Peripheral oedema, epistaxis, gingival bleeding, petechiae and echymoses are the late manifestations.
Without treatment, death occurs with in 3 to 20 months in 40 to 94% of adult and in 75 to 85% cases of children. Death often is due to superinfection bacterial pneumonia, septicaemia, concurrent infections (tuberculosis, dysentery) or uncontrolled severe haemorrhage from GIT and severe anaemia.
Diagnosis :
In endemic areas, the persons with prolonged fever , progressive weight loss and weakness, marked splenomegaly, hepatomegaly, anaemia, leucopenia, hypergammaglobulinaemia and low serum albumin are highly suggestive of visceral leishmaniasis.Laboratory or Parasitic diagnosis: Demonstration of Leishmania spp. in appropriate clinical specimens is the definitive diagnosis of the condition. The parasites are demonstrated in different clinical specimens by direct microscopy, culture or animal inoculation.
1- Direct microscopy: Direct microscopy of the splenic, bone marrow, liver or lymph node aspirotion smears, fixed with methanol, then stained with Giemsa stain as for thin blood film; show L.D. bodies (amastigotes of L. donovani). L.D. bodies are usually found within macrophages. Some of the L.D. bodies can also be demonstrated free, released from the cells ruptured during making of the film. L.D. bodies can also be seen occasionally within non-nuclear cells in the stained smear of the bully coat of the peripheral blood.
2-Serological tests : to demonstrate specifc anti-le ishmanial antibodies in the serum are specially useful in the diagnosis of early phase of visceral leishmaniasis by :
-indirect immuno-fiuorescent (IFA):
- indirect haemagglutination(IHA):
- enzyme-linked Immunosorbent assay (EL1SA)