1
Antimicrobial chemotherapy
Drugs have been used for the treatment of infectious diseases since the
17th century (e.g. emetine for amebiasis); however, chemotherapy as a
science began in the first decade of the 20th century with understanding
of the principles of selective toxicity, the specific chemical relationships
between microbial pathogens and drugs, the development of drug
resistance, and the role of combined therapy.
The development of antimicrobial chemotherapy began in 1935 with
the discovery of the sulfonamide. In 1940, it was demonstrated that
penicillin, discovered in 1929, could be an effective therapeutic
substance. During the next 25 years, research on chemotherapeutic agents
centered largely around substances of microbial origin called antibiotics.
The isolation, concentration, purification, and mass production of
penicillin were followed by the development of streptomycin ,
tetracyclines and many other agents.
1- Bacteriocidal drugs :- these have a rapid lethal action e.g. pencillins ,
cephalosporins & aminoglycosides .
2- Bacteriostatic drugs :- these are inhibit the division i.e. growth of
organism e.g. sulfonamides , tetracyclines & chloramphenicol .
Range of action of antibiotics
Antibiotics fall into 3 main categories :-
a – a ctive mainly against G
+ve
organisms like : penicillin , erythromycin
& lincomycin .
b – active mainly against G
-ve
organisms like : polymyxin & nalidixic acid
.
c – active against both G
+ve
& G
-ve
organisms ( broad spectrum activity )
like : ampicillin & ciprofloxacin .
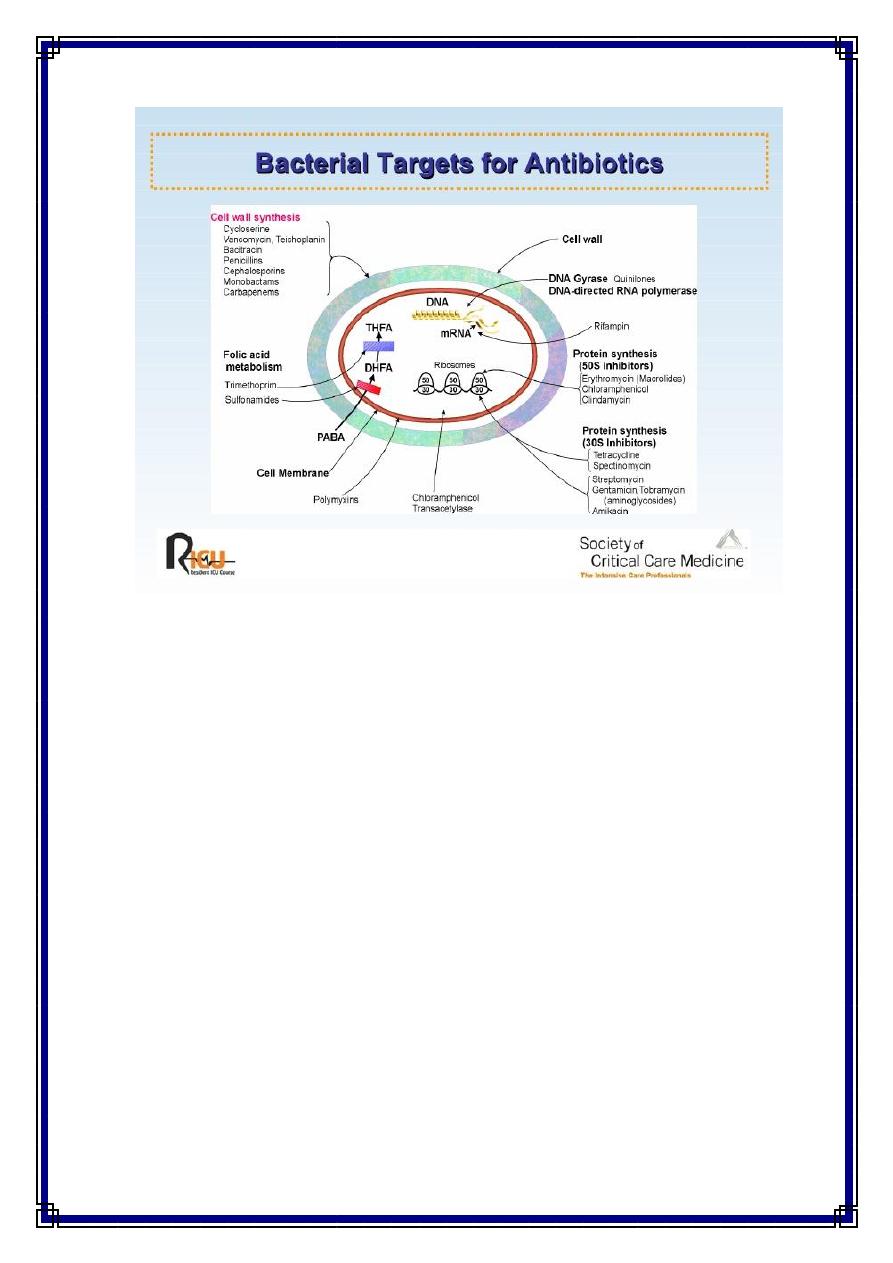
Mechanisms of action of chemotherapeutic agents
An ideal antimicrobial agent should have selective toxicity i.e. it can
kill or inhibit the growth of a microorganism in concentration that are not
harmful to the cells of the host . Disinfectants e.g. phenol and antiseptics
e.g. alcohol & iodine , destroy bacteria but they are highly toxic to tissue
cells & are unsuitable for use as chemotherapeutic agents .
Thus , the mechanisms of action of a chemotherapeutics must depend
on the inhibition of a metabolic channel or a structure present in the
microbe but not in the host cells . several mechanisms are known :-
2
1 – Inhibition of cell wall synthesis :-
Due to its unique structure & function , the bacterial cell wall is an
ideal point of attack by selective toxic agents , such as ß-lactams that
include penicillins & cephalosporins interfere with cell wall synthesis
and cause bacteriolysis .
2 – Inhibition of cytoplasmic membrane function :-
Some antibiotics cause disruption of the cytoplasmic membrane and
leakage of cellular proteins & nucleotides leading to cell death , for
example polymyxins.
3 – Inhibition of protein synthesis :-
Many chemotherapeutic block protein synthesis by acting on the 30
s
or 50
s
subunit of bacterial ribosomes such as : tetracyclines ,
erythromycin and aminoglycosides e.g. tobramycin & gentamycin .
Bacteria have 70
s
ribosome while mammalian cells have 80
s
ribosome
the composition of each type ,their subunit and function explain why
drugs can inhibit protein synthesis in bacteria but not in mammal .
4 – Inhibition of nucleic acid synthesis :-
These can act on any steps of the DNA replication or RNA synthesis
e.g. quinolone , refampicin , novobiocin & sulfonamide . rifampen inhibit
bacterial growth by binding to DNA-dependent RNA polymerase of
bacteria , thus it inhibit RNA synthesis . While quinolones inhibit DNA
synthesis by blocking of DNA gyrase.
5 – Competitive inhibition :-
In which the drugs compete with an essential metabolite for the same
enzyme e.g. p – aminobenzoic acid ( PABA ) is an essential metabolite
for many organisms because its precursor in folic acid synthesis which is
used in nucleic acid synthesis , sulfonamide are structural analogues to
PABA so its enter in the reaction in place of PABA & compete for the
active center of the enzyme thus inhibiting folic acid synthesis .
3
Mechanisms of resistance to antimicrobial agents
In the treatment of infectious diseases , one of the serious problem is
the development of bacterial resistance to the antibiotic used . The
mechanisms by which the organism develop resistance may be one of the
following :-
1 – The organism produced enzymes that destroy the drug e.g. production
of ß–lactamases that destroy penicillin by penicillin resistant
staphylococci & acetyltransferase which produced by gram negative
bacilli to destroy chloramphenicol.
2 – The organism change its permeability to the drug by modification of
protein in the outer cell membranes , thus impairing its active transport
into the cell e.g. resistance to polymyxins .
3 – The organism develop an altered receptor site for the drug e.g.
resistance to aminoglycosides is associated with alteration of a specific
protein in the 30
s
subunit of the bacterial ribosome that serve as a binding
site in susceptible organisms .
4 – The organism develop an altered metabolic pathway that by passes
the reaction inhibited by the drug e.g. sulfonamide-resistant bacteria
acquire the ability to use performed folic acid with no need for
extracellular PABA .
4
Origin of resistance to antimicrobial agents
These mechanisms may be of non genetic or genetic origins:
A – Non genetic drug resistance :- this include
1 – Metabolic inactivity :- Most antimicrobial agents act effectively
only on replicating cells , non multiplying organisms are phenotypically
resistant to drugs such as M. tuberculosis which survive for years in the
tissues & their resistance is due to metabolic inactivity but if they start
multiply after suppression of cellular immunity of the patient , they
become susceptible to the drugs .
2 – Loss of target structure :- Protoplast or L-forms of bacteria are
penicillin resistant because they lost their cell wall which is a structural
target site of the drug .
3 – Bacteria may infect the host in the sites where antimicrobial are
exclude or not active.
B – Genetic drug resistance :- this include
1 – Plasmid mediated resistance :- Plasmid is an extra-chromosomal
genetic elements associated with bacterial resistance to antibiotics ,
plasmids frequently carry many genes that code for the production of
enzymes that inactivate or destroy the antibiotics e.g. ß- lactamases
which destroys the ß- lactam ring in penicillin & cephalosporin , plasmids
may result in epidemic resistance among bacteria by moving from one to
the other by conjugation , transduction or transformation .
2 - Transposon-mediated resistance :- Many transposons carry genes
that code for drug resistance , as they move between plasmids &
chromosomes they can transfer this property to bacteria . the process
called transposition .
3 – Chromosomal drug resistance :- This develop as a result of
spontaneous mutation in a genes that controls susceptibility to an
antimicrobial agents , the most common result of chromosomal mutation
is alteration of the receptors for a drug . For example : streptomycin
resistance can result from a mutation in the chromosomal gene that
controls the receptor for streptomycin located in the 30s
bacterial
ribosome .
Complications of antibacterial chemotherapy
1 – Development of drug resistance :-
This is one of the most serious complications of chemotherapy , the
emergence of resistant mutants is encouraged by inadequate dosage ,
prolonged treatment , the presence of closed focus of infection and the
5
abuse of antibiotics without in vitro susceptibility testing . The problem is
more serious when resistant strain develop in the community e.g. in
hospitals its common to find that about 90 % of Staphylococcus aureus
strains are resistant to penicillin .
2 – Drug toxicity :-
Many of antibacterial drugs have toxic side effects , this can be due
to the over dosage , prolonged use or narrow margin of selective toxicity
e.g. streptomycin affect on the 8
th
cranial nerve leading to deafness ,
aminoglycosides are nephrotoxic , tetracyclines inhibit growth &
development of the bones and teeth in the developing infants & children .
3 – Super infection :-
a – this may occur by pre-existing resistance strains present in the
environment e.g. penicillin resistance Staph. aureus in hospital infection .
b – Another type of super infection is due to suppression of normal flora
by the antibiotic used and their replacement with drug resistant organisms
which cause disease like : Candida in the mouth causing oral thrush .
4 – Hypersensitivity :-
The drug may act as hapten , binds to tissue proteins and stimulates an
immune response leading to tissue damage i.e hypersensitivity .
Any type of hypersensitivity reaction can occur with the several
antibiotics . the more serious is anaphylactic shock which may occur with
penicillin & cephalosporins . Mild manifestations are urticaria , skin rash
, diarrhea , vomiting and jaundice .
Chemoprophylaxis
Is the use of antimicrobial agents to prevent rather than to treat
infectious diseases . The following are principal conditions for which
prophylactic antibiotics are positively indicated :-
1 – The use of benzathine penicillin G injections every 3-4 weeks to
prevent reinfection with Streptococcus pyogenes in rheumatic patients
2 – A single large dose of amoxicillin given immediately prior to dental
procedures is recommend for patients with congenital or rheumatic heart
disease to prevent endocarditis .
3 – Rifampicin 600 mg twice a day for 2 days give to the exposed
patients during epidemics of meningitis .
4 – Oral administration of tetracycline to prevent cholera .
5 – The use of ampicillin to prevent neonatal sepsis & meningitis in
children born to mothers carrying group B streptococci in the vagina .
6 – Ceftriaxone to prevent gonorrhea .
7 – Chemoprophylaxis in surgery .
Clinical use of antibiotics
6
The following principles should be observed :-
1 – Antibiotics should not be given for trivial infections .
2 – They used for prophylaxis in special conditions .
3 – Treatment should be based on a clear clinical and bacteriological
diagnosis .
4 – Antibiotics for systemic treatment must be given in a full therapeutic
doses for adequate period .
5 – Combined therapy with two or more antibiotics is required for some
conditions : -
a – serious resistant infections such as meningitis .
b – Severe mixed infections e.g. peritonitis following perforation of the
colon.
