
Thi Qar University
College of Medicine
Internal Medicine Department
BY
Dr. FAEZ KHALAF, SUBSPACIALITY GIT
MBChB, FIBMS-CABMS(MED)
MD-FACP(US),FIBMS(GIT&HEP)

DISORDERS OF THE COLON AND RECTUM
Tumours of the colon and rectum
Polyps and polyposis syndromes

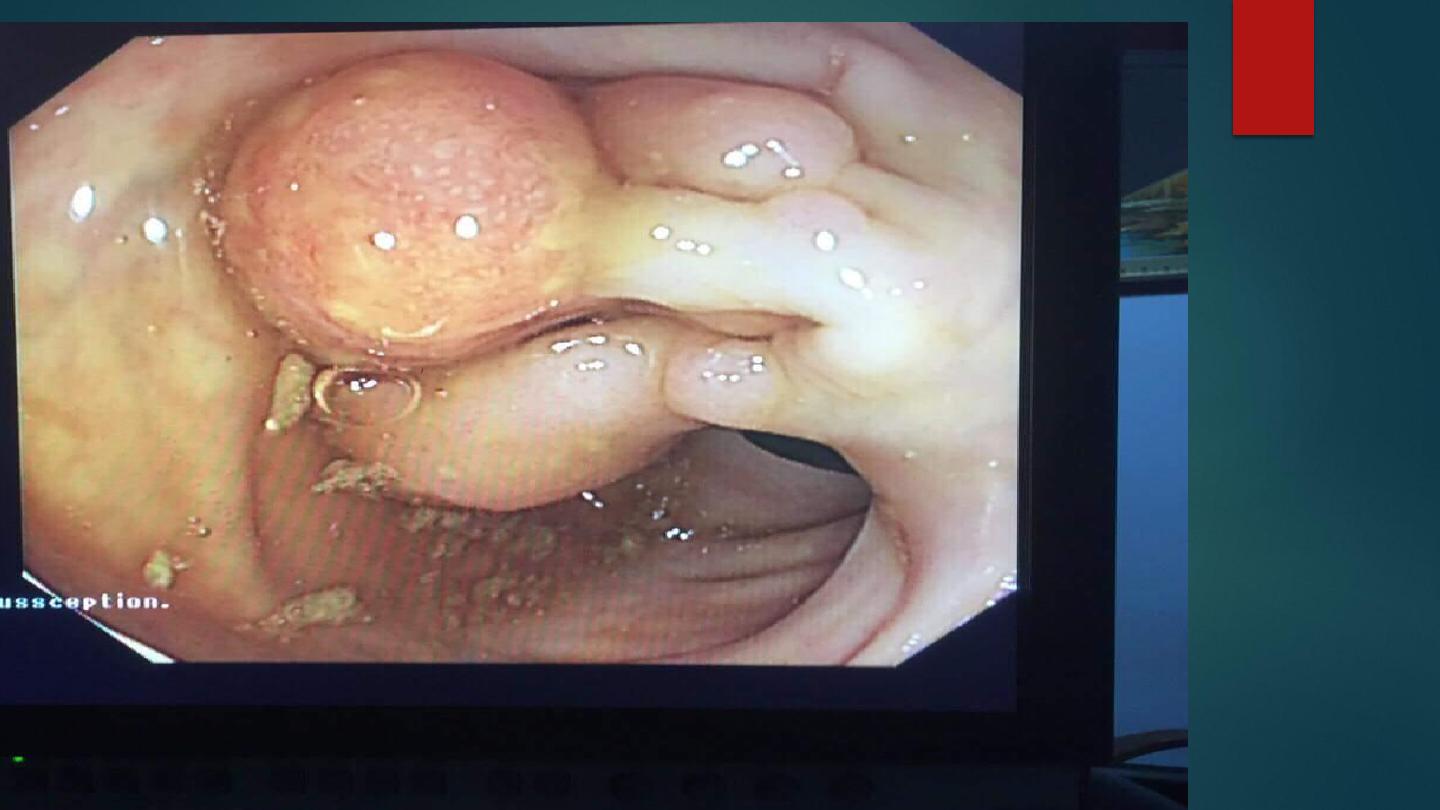
Polyps may be neoplastic or non-neoplastic, single or multiple, and vary from a
few mm to several cm in size.
Colorectal adenomas: Extremely common in the Western world;
50% of people > 60 yrs
. of age have adenomas, usually in the rectum and distal
colon.
Nearly all colorectal carcinomas develop from adenomatous polyps
. Large,
multiple, villous or dysplastic polyps carry a higher risk of malignancy.
Adenomas are usually asymptomatic and discovered incidentally
.
Occasionally, they cause bleeding and anaemia.
Villous adenomas sometimes secrete large amounts of mucus, leading to
diarrhoea and hypokalemia
.

Discovery of a polyp at sigmoidoscopy is an indication for colonoscopy and
polypectomy, which considerably reduce subsequent cancer risk.
Very large or sessile polyps sometimes require surgery.
Once all polyps have been removed, patients < 75 should undergo
surveillance colonoscopy at 3
–5-yr intervals, as new polyps develop in 50%.
Between 10 and 20% of polyps show evidence of malignancy.
When cancer cells are found within 2 mm of the resection margin, and when the
polyp cancer is poorly differentiated or invading lymphatic, segmental colonic
resection is recommended.
Others can be followed up by surveillance colonoscopy.
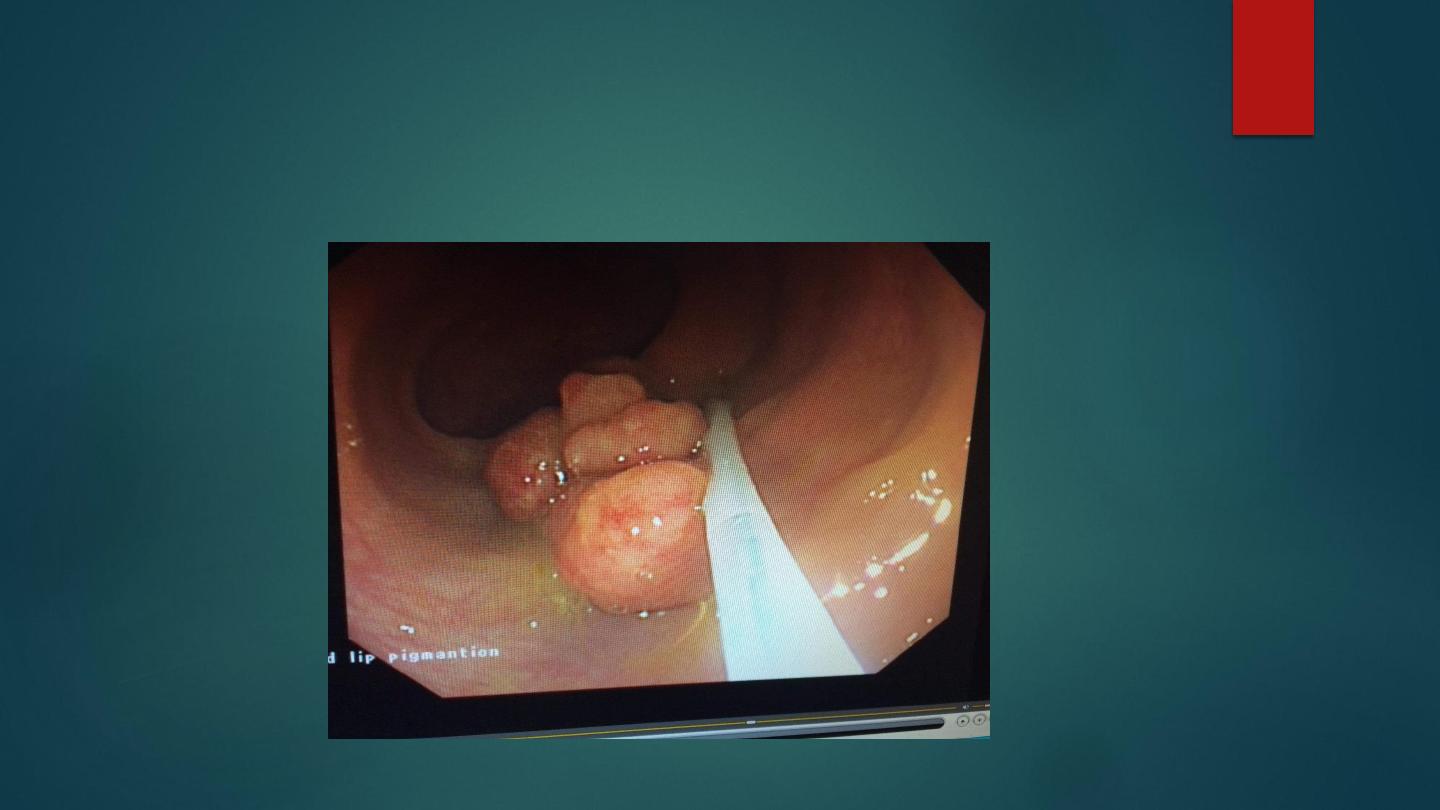
The polyposis syndromes are classified by histopathology. They
include neoplastic
familial adenomatous polyposis
and several
non neoplastic
syndromes, including Peutz
–Jeghers syndrome
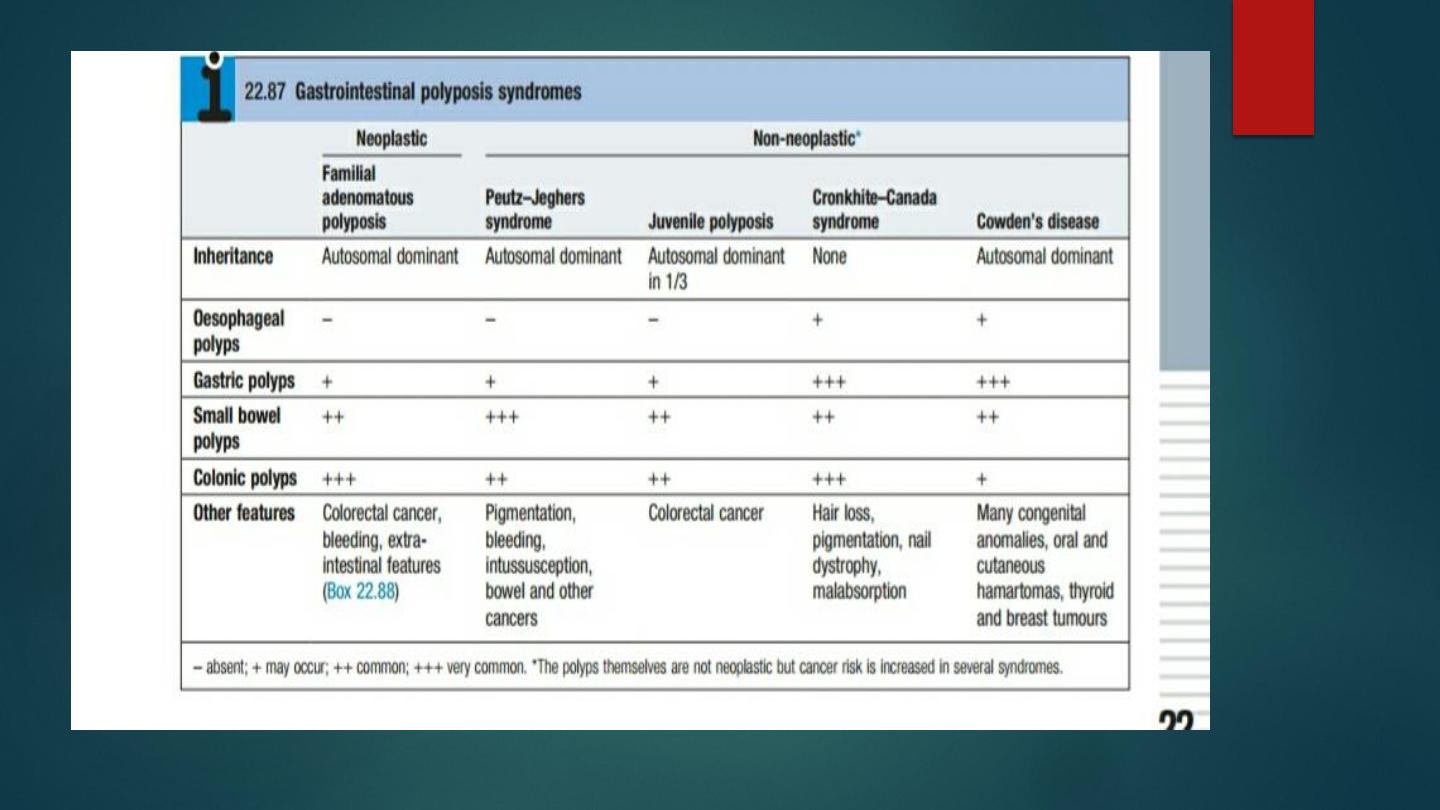

Familial adenomatous polyposis (FAP):
An uncommon (1 in 13 000)
autosomal dominant disorder
. Around 20% are
new mutations with no family history. By age 15, 80% of patients will develop
up to several thousand adenomatous colonic polyps, with symptoms such as
rectal bleeding beginning a few years later.
Within 10
–15 yrs of the appearance of adenomas, colorectal cancer will
develop, affecting 90% by the age of 50.
Malignant transformation of duodenal adenomas occurs in 10% and is the
leading cause of death after prophylactic colectomy
.
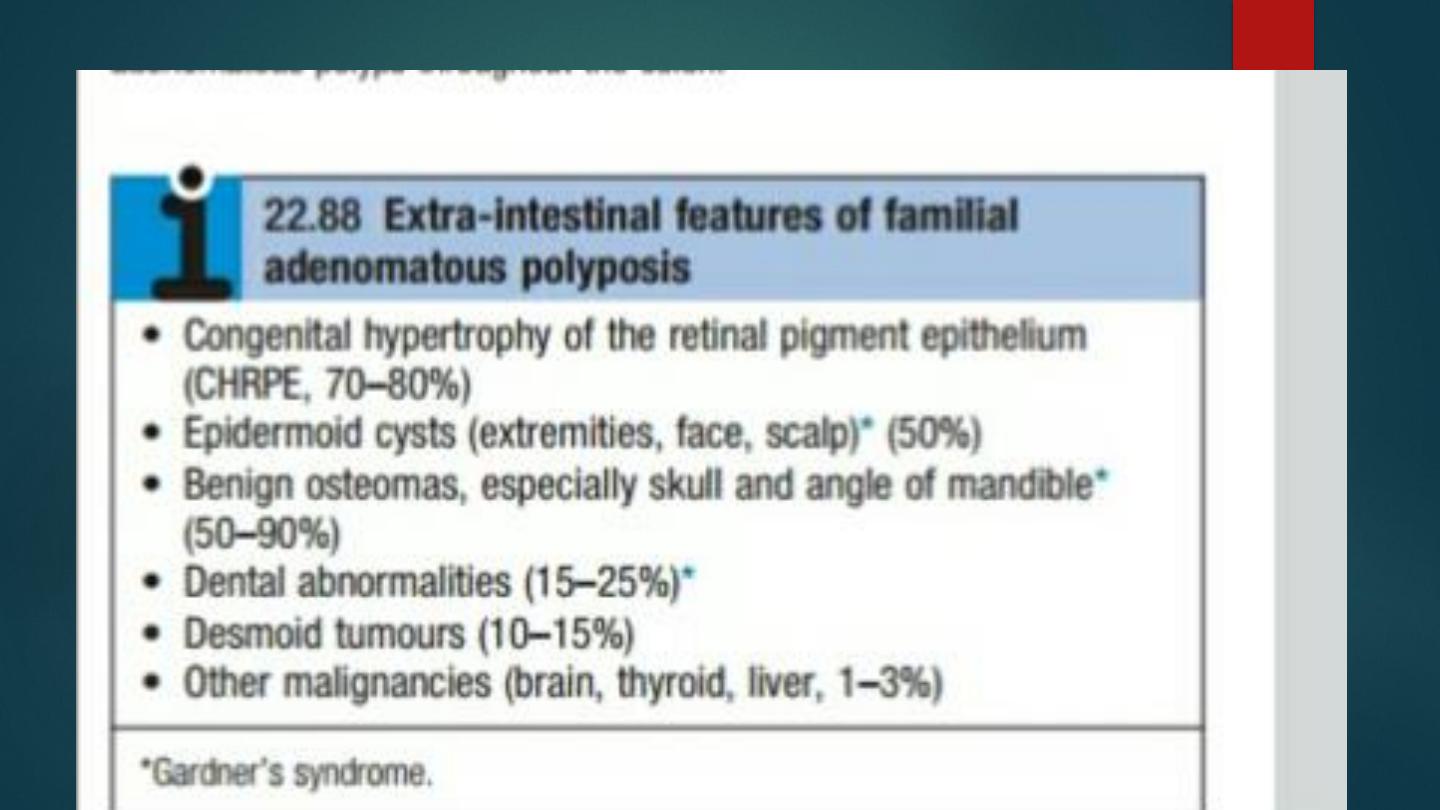
Extra-intestinal features include subcutaneous epidermoid cysts, benign
Osteomas, dental abnormalities and lipomas. Dark, round, pigmented retinal
lesions
Early identification is essential. Sigmoidoscopy, if normal, excludes the
diagnosis. Genetic testing confirms the diagnosis, and
first-degree relatives should also be tested.

Children of FAP families should undergo mutation
testing at 13
–14 yrs of
age, followed by regular sigmoidoscopy in those carrying the mutation.
Affected
individuals should undergo colectomy on leaving school or college.
Periodic upper GI endoscopy is recommended to detect duodenal
adenomas
.


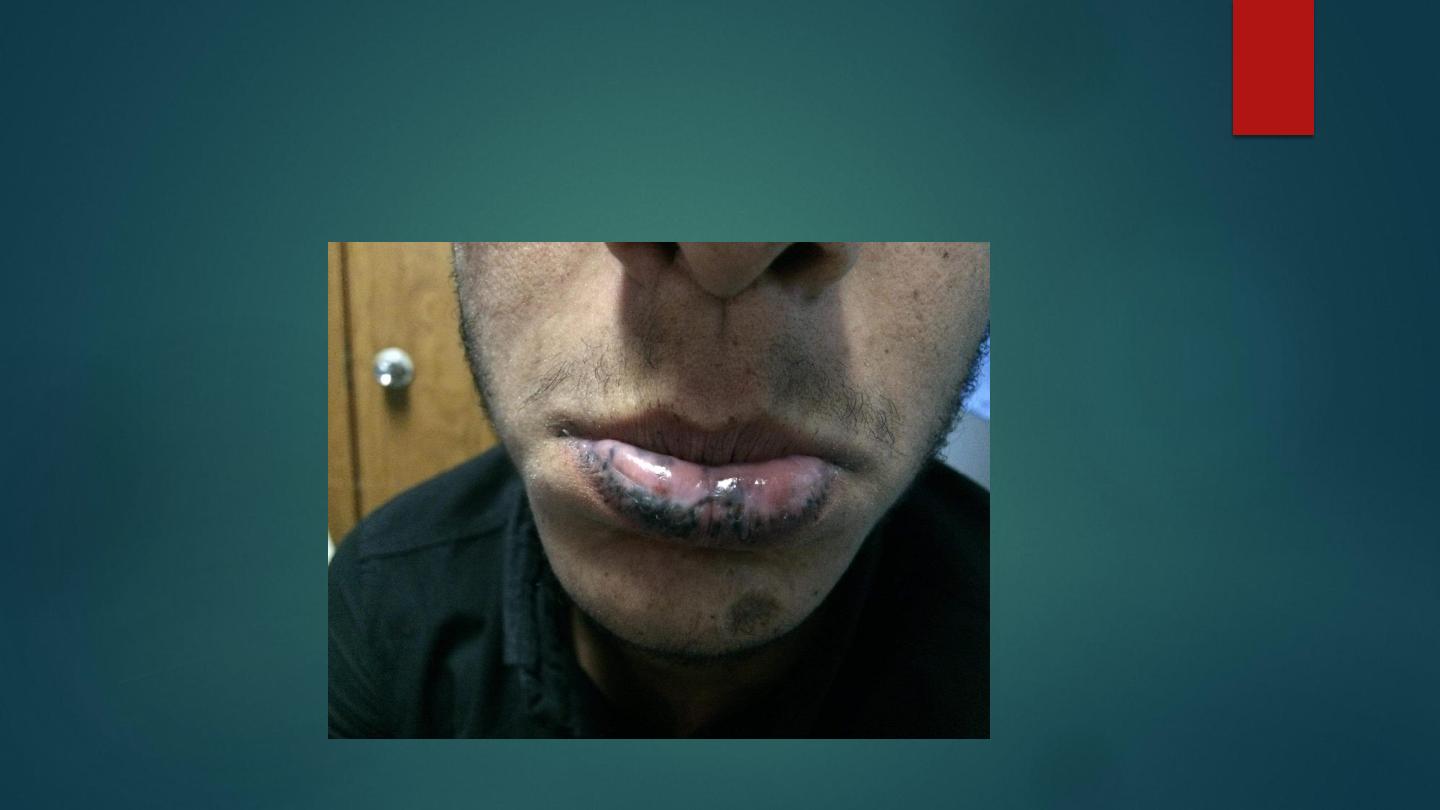
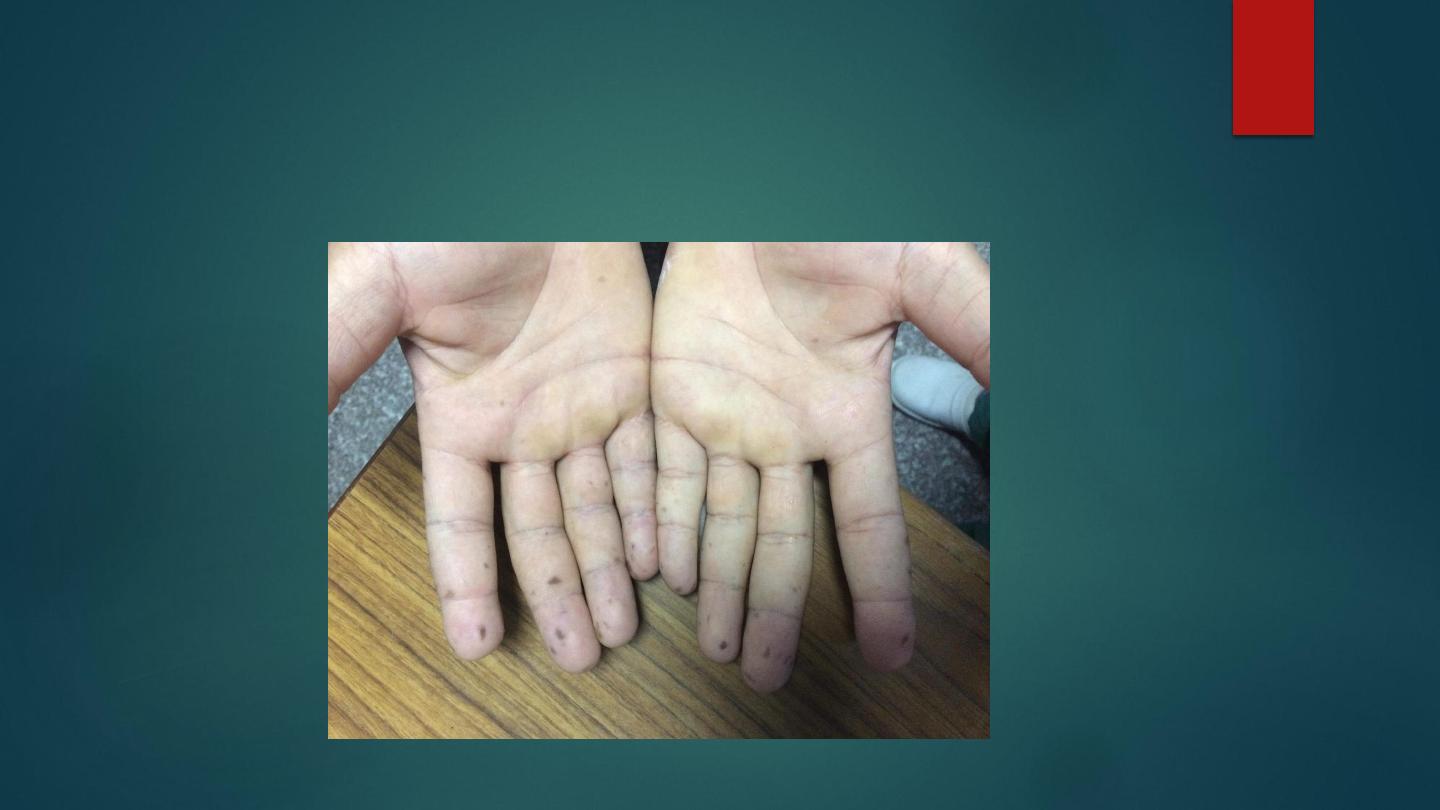
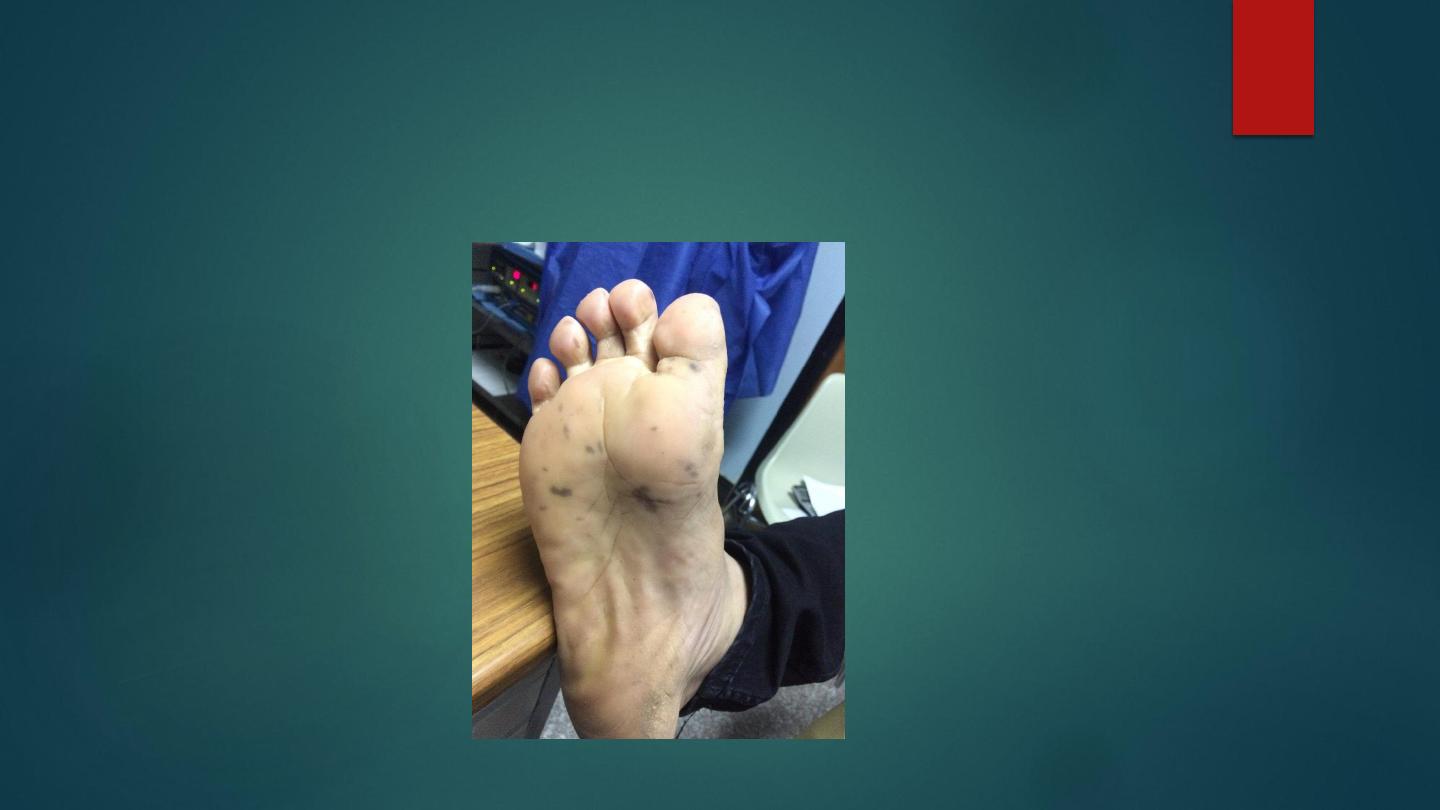
Peutz
–Jeghers syndrome
Comprises multiple hamartomatous polyps in the small intestine and colon,
and melanin pigmentation of the lips, mouth and digits, and is usually
asymptomatic.
There is a small but significant risk of small bowel or colonic
adenocarcinoma
and of cancer of the pancreas, lung, ovary, breast and endometrium
.
Patients should undergo regular upper endoscopy, colonoscopy and
imaging of the small bowel and pancreas


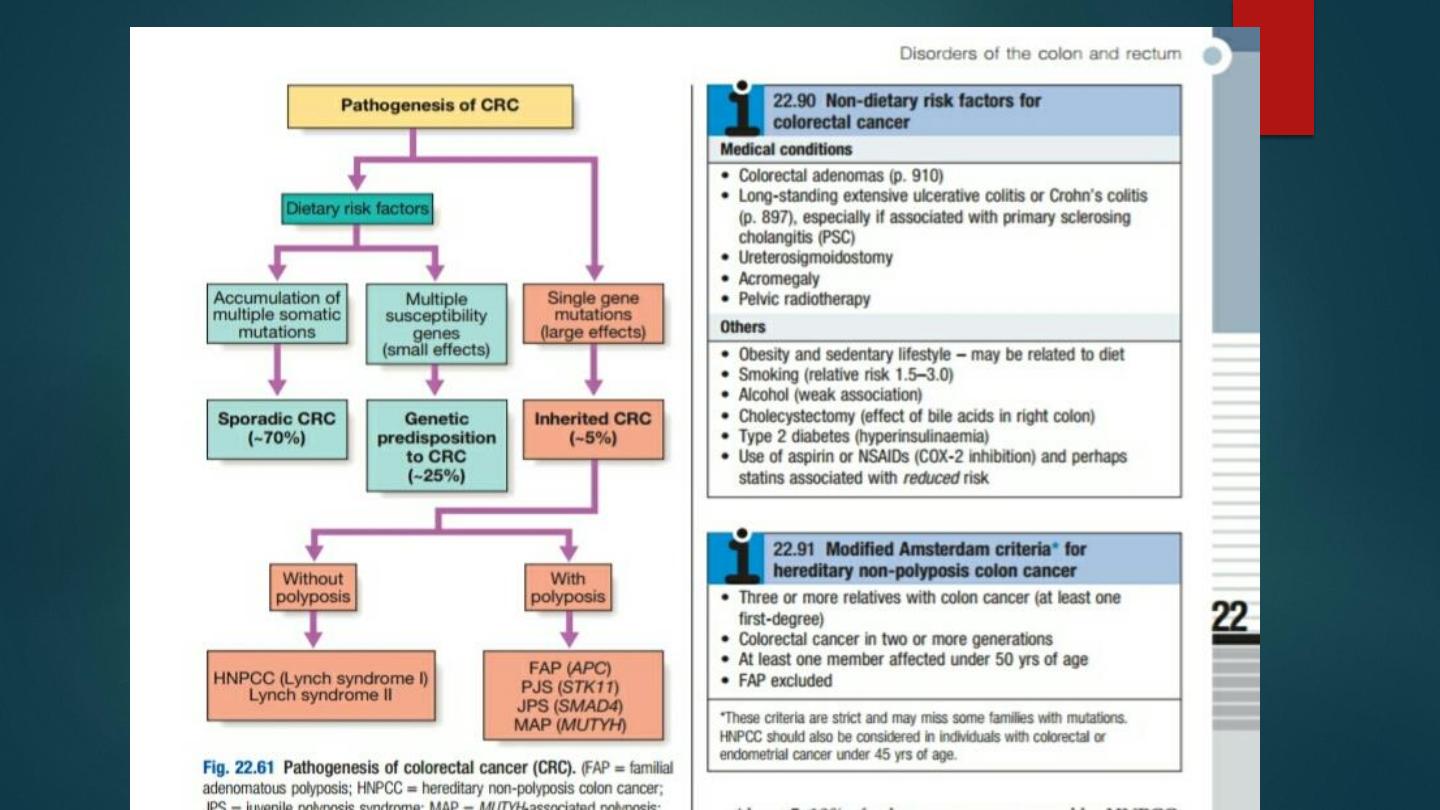
Colorectal cancer
Although relatively rare in the developing world,
colorectal cancer is the
second most common internal malignancy and the second leading cause of
cancer deaths in Western countries
.
In the UK the incidence is 50
–60 per 100 000/yr.
The condition becomes increasingly common over the age of 50.
Around 80% are
‘sporadic’, 5–10% are hereditary non-polyposis
colon cancer (HNPCC), 1% are associated with FAP and 1% with
inflammatory bowel disease
.
Environmental factors account for > 80% of all
‘sporadic’ colorectal
cancers. The risk declines in migrants who move from high- to low-risk
countries.
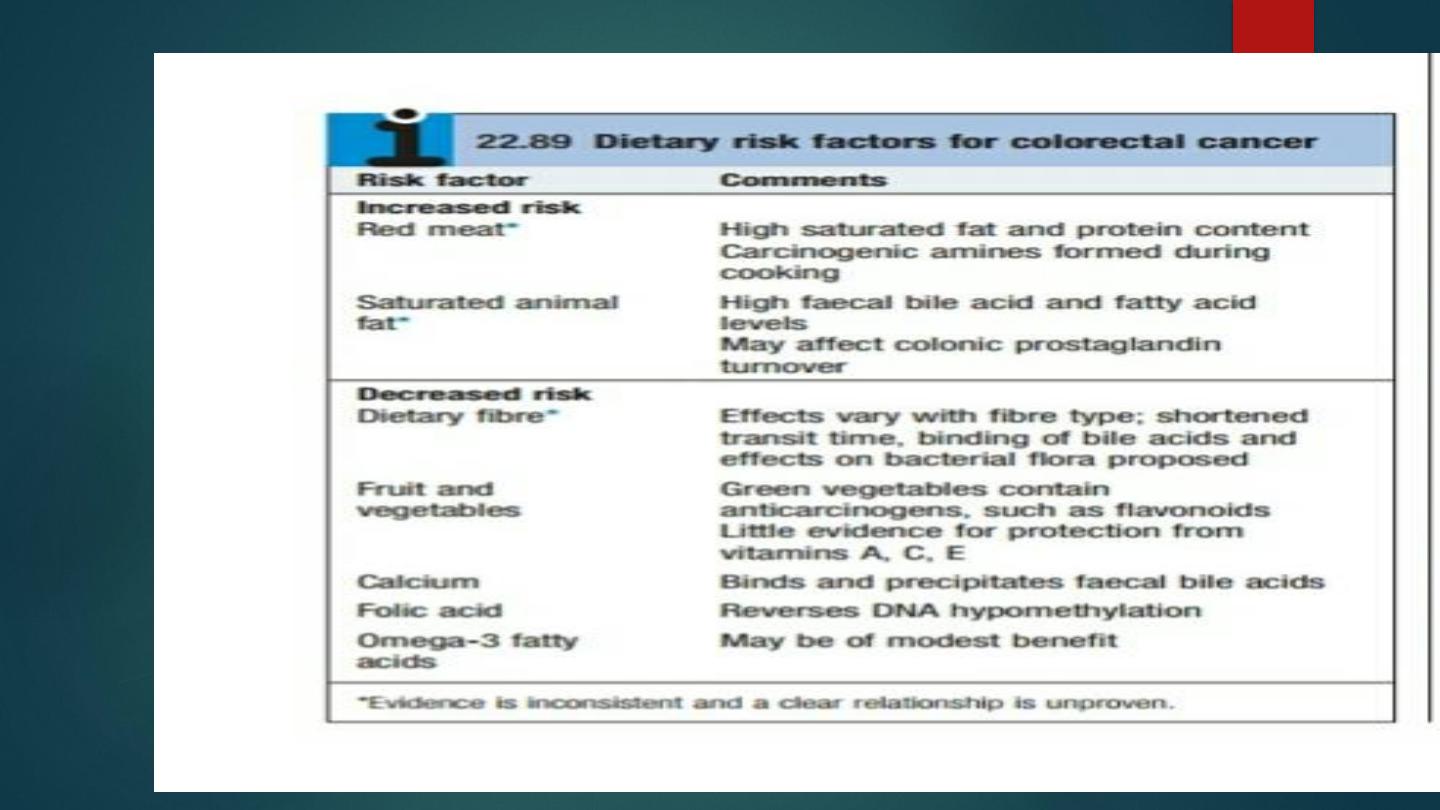
Dietary factors increasing risk are
red meat and saturated fat
, while
fibre, fruit,
vegetables, folic acid and calcium appear to protect

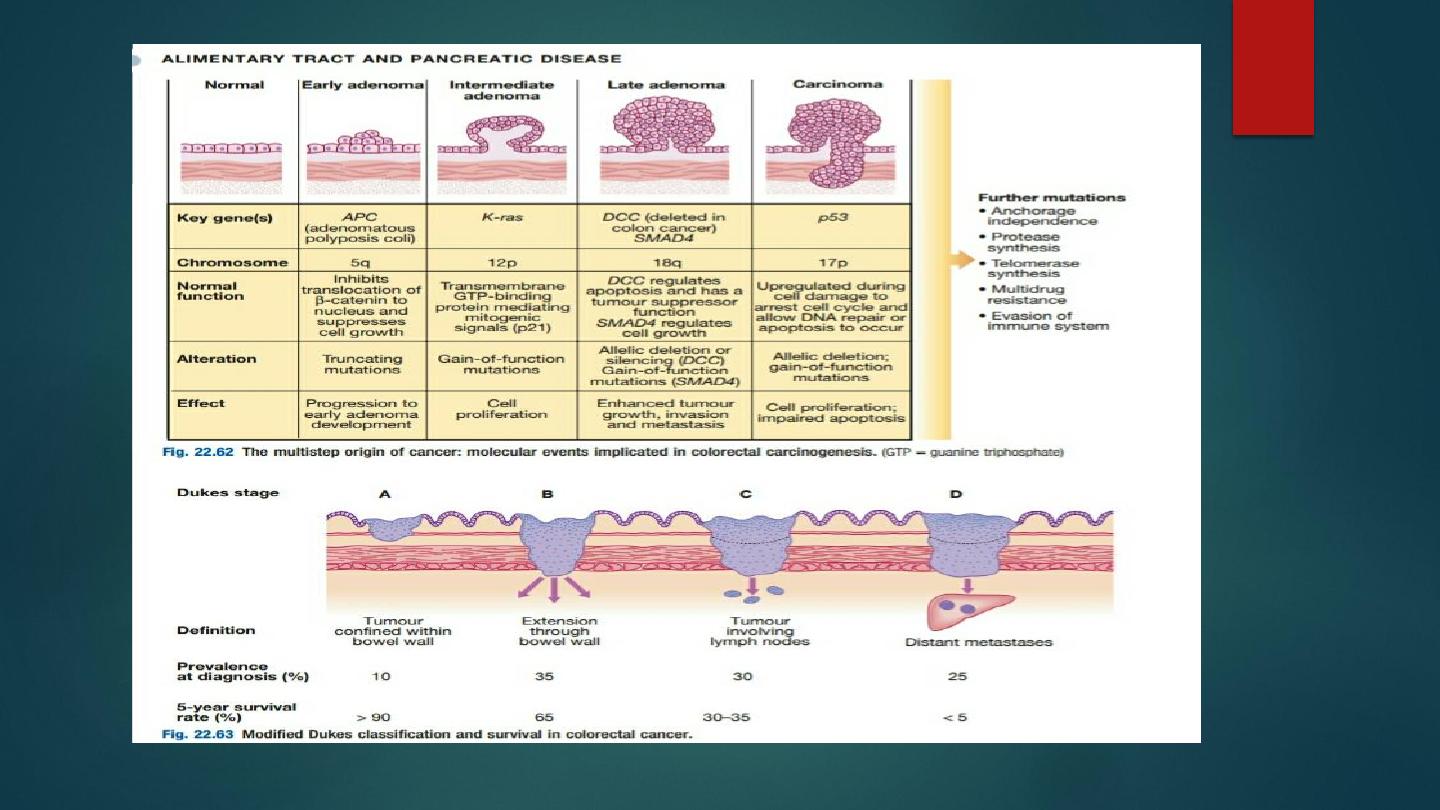
Colorectal cancer development results from the accumulation of multiple
genetic mutations.
HNPCC occurs in those with a family history, often having relatives who were
affected at a young age.
The lifetime risk of colorectal cancer in affected individuals is 80%.
Those who fulfil the criteria for diagnosis should be referred for pedigree
assessment, genetic testing and colonoscopy, which needs to be repeated
every 1
–2 yrs, despite which interval cancers still occur. The lifetime risk of
developing cancer with one or two affected first-degree relatives is 1 in 12 and
1 in 6, respectively.

The risk is even higher if relatives were affected at an early age.
Most tumours arise from malignant transformation of a benign adenomatous
polyp
.
Over 65% occur in the recto sigmoid
and a further 15% recur in the caecum or
ascending colon.
Rectal cancers may invade the pelvic viscera and side walls.
Lymphatic
invasion is common at presentation, as is hepatic spread. Tumour stage at
diagnosis
determines prognosis.
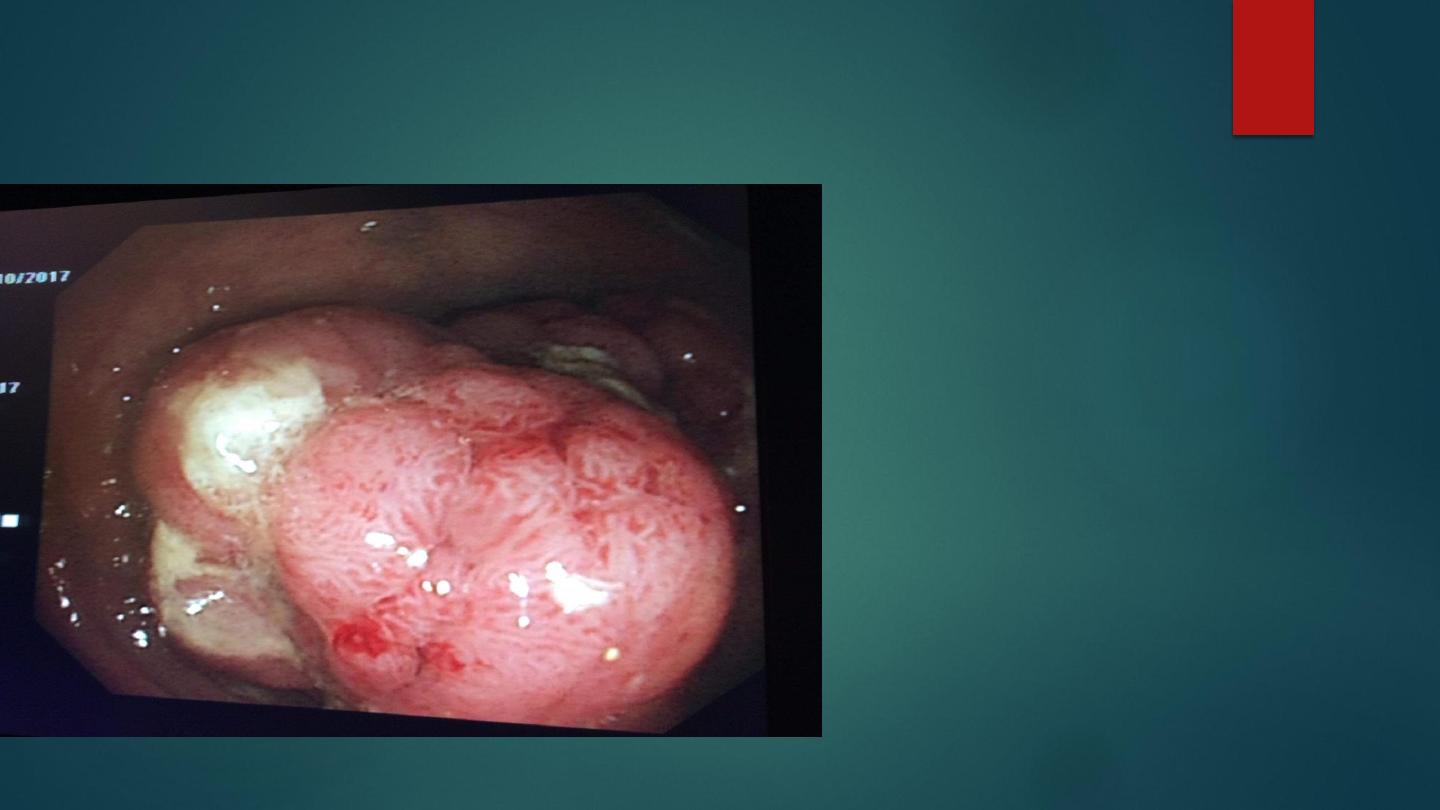

Clinical features
In tumours of the left colon, fresh rectal bleeding is common and obstruction
occurs early.
Tumours of the right colon present with anaemia from occult bleeding or with
altered bowel habit, but obstruction is a late feature
.
Colicky lower abdominal pain is present in two-thirds of patients and rectal
bleeding occurs in 50%.
A minority present with either obstruction or perforation.
Carcinoma of the rectum usually causes early bleeding, mucus discharge or a
feeling of incomplete emptying
.
On examination there may be a palpable mass, signs of anaemia or
hepatomegaly from metastases.
Low rectal tumours may be palpable on digital examination
.

Investigations
Colonoscopy: more sensitive and specific than barium enema and permits
biopsy
●
CT colonography: detects tumours and polyps > 6 mm diameter and can
be used if colonoscopy is incomplete or high risk.
●
CT: valuable for
detecting hepatic metastases.
●
Pelvic MRI: to stage rectal tumours.
●
Intraoperative USS: increasingly being used for this purpose.
●
Carcinoembryonic antigen (CEA): normal in many patients and so of little
use in diagnosis, but serial CEA can help to detect early recurrence during
follow-up.
Treatment should be discussed and planned at a multidisciplinary meeting.

management
Neo-adjuvant therapy: Pre-operative radiotherapy or chemo radiotherapy is used
to
‘down-stage’ large rectal cancers, making them resectable.
Surgery: The tumour is removed, along with pericolic lymph nodes.
Direct anastomosis is performed wherever possible or colostomy if not.
Solitary hepatic or lung metastases are sometimes resected at a later stage.
Post-operatively, patients should undergo colonoscopy after 6
–12 mths and
periodically thereafter to search for local recurrence or development of new
‘metachronous’ lesions, which occur in 6% of cases
.

Adjuvant therapy
: Two-thirds of patients have lymph node or distant
spread at presentation and are, therefore, beyond cure with surgery alone .
Most recurrences are within 3 yrs, either at the site of resection or in lymph
nodes, liver or peritoneum.
Adjuvant chemotherapy reduces recurrence risk in patients with
Dukes C colon cancer and some Dukes B tumours.
Post-operative radiotherapy is used to reduce the risk of local recurrence if
resection margins are involved.
Palliation
: Surgical resection of the primary tumour is appropriate for
some patients with metastases to treat obstruction, bleeding or pain.
Palliative chemotherapy with 5-fluorouracil/folinic acid, oxaliplatin or
irinotecan improves survival. Pelvic radiotherapy is sometimes useful for
rectal pain, bleeding or severe tenesmus.
Endoscopic laser therapy or insertion of an expandable metal stent can be
used to relieve obstruction

Secondary prevention (screening):
This aims to detect and remove lesions at an early or pre-malignant stage.
Several potential methods exist.
Widespread screening by regular FOB testing in those > 50
increases early detection and reduces colorectal cancer mortality, and has
been adopted in a number of countries.
Colonoscopy remains the gold standard but requires expertise, is
expensive and carries risks
.
Flexible sigmoidoscopy has been shown to reduce overall colorectal
cancer mortality by ~35% (70% for cases arising in the recto sigmoid). It is
recommended in the USA every 5 yrs in all persons over the age of 50.

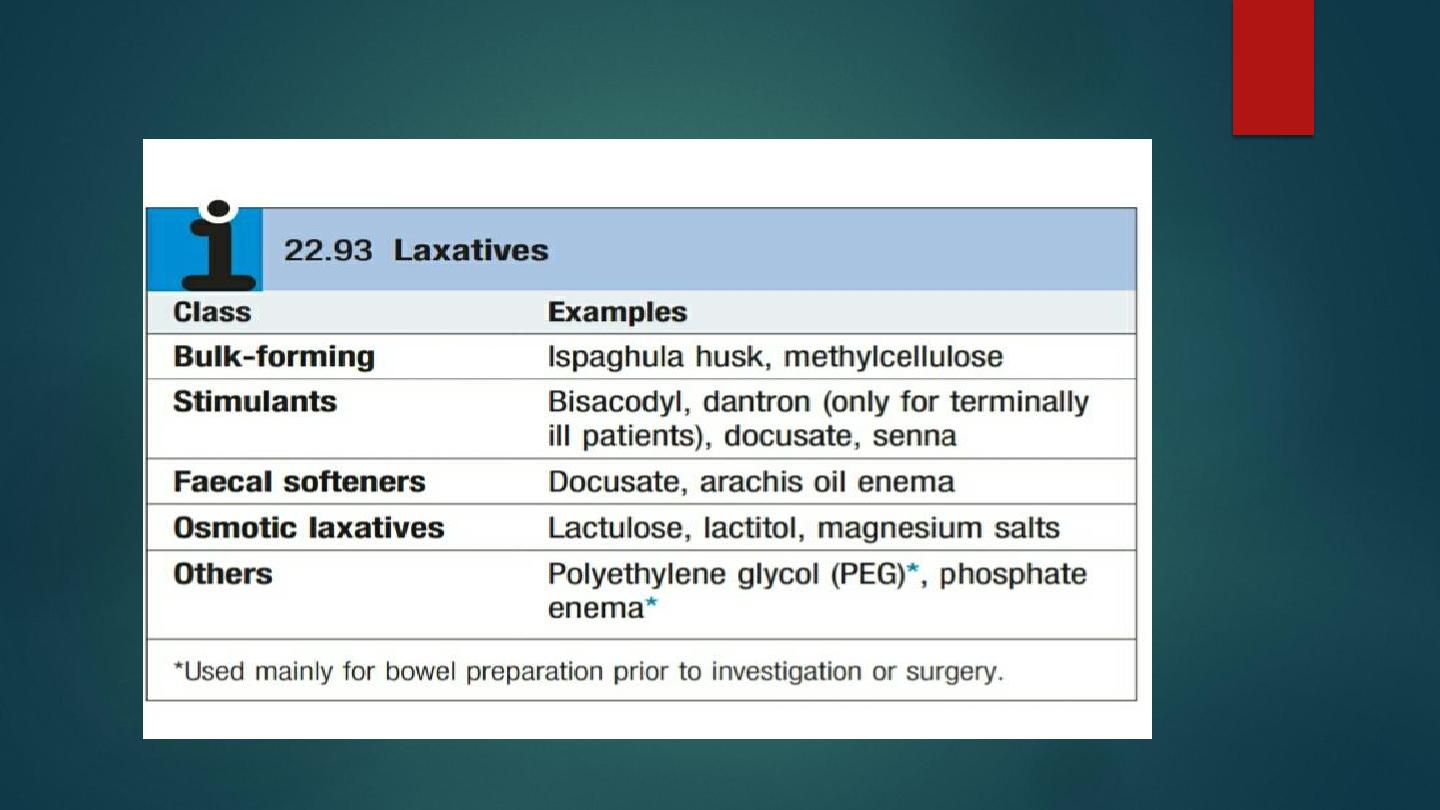
Constipation and disorders of defecation
Simple constipation
: Constipation is extremely common and usually responds
to increased dietary fibre or bulking agents with an adequate fluid intake.
Severe idiopathic constipation
: This occurs almost exclusively in young
women and often begins in childhood or adolescence. The cause is unknown
and the condition is often resistant to treatment. Bulking agents may exacerbate
symptoms but prokinetic agents or balanced solutions of polyethylene glycol
3350 benefit some patients with slow transit

Faecal impaction
: Impaction tends to occur in frail, disabled, immobile or
institutionalised patients. Drugs, autonomic neuropathy and painful anal
conditions also contribute. Obstruction, perforation and bleeding may
supervene. Treatment involves softening the stool with arachis oil enemas,
hydration and careful digital disimpaction.
Melanosis coli and laxative misuse syndromes
:
Long-term stimulant laxative use causes brown discoloration of the colonic
mucosa (
‘tiger skin’), which is benign and resolves with laxative withdrawal.
Surreptitious laxative misuse is a psychiatric condition seen in young women,
who may have a history of bulimia or anorexia nervosa. They complain of
refractory watery diarrhoea and deny laxative use. Screening of urine for
laxatives may be helpful.

Hirschsprung
’s disease:
Congenital absence of ganglion cells causes the internal
anal sphincter to fail to relax, leading to constipation and colonic dilatation
(megacolon). Constipation, abdominal distension and vomiting usually develop
immediately after birth but occasionally in childhood or adolescence.
A family history is present in one-third. The rectum is empty on digital examination.
Barium enema shows a small rectum and colonic dilatation above the narrowed
segment.
Full-thickness biopsies confirm the absence of ganglion cells. Treatment involves
resection of the affected segment
.
Acquired megacolon
: In childhood, this is a result of voluntary withholding of stool
during toilet training. It presents after the first year and is distinguished from
Hirschsprung
’s disease by the urge to defecate and the presence of stool in the
rectum. It usually responds to osmotic laxatives.
In adults, acquired megacolon may occur in depressed or demented patients, either
as part of the condition or as a side-effect of antidepressant drugs. Prolonged misuse
of stimulant laxatives may cause megacolon, as may neurological disorders,
scleroderma, hypothyroidism and opioid abuse.
Patients are managed by treating the underlying cause, and with high-residue diets,
laxatives and enemas.

Acute colonic pseudo-obstruction (Ogilvie
’s syndrome):
This can be caused by
trauma, surgery, respiratory or renal failure, or diabetes
mellitus
. There is sudden, painless, massive enlargement of the proximal colon
without features of mechanical obstruction.
Bowel sounds are normal or high-pitched rather than absent. The condition
may progress to perforation and peritonitis.
X-rays show colonic dilatation with air extending to the rectum.
A caecal diameter > 10
–12 cm
is associated with a high risk of perforation.
Barium enemas demonstrate the absence of mechanical obstruction.
Management consists of treating the underlying disorder and correcting any
biochemical abnormalities.
Neostigmine is used to enhance gut motility.
Decompression either with a rectal tube or by careful colonoscopy may be
effective

ISCHAEMIC GUT INJURY
Acute small bowel ischaemia
Superior mesenteric blood flow may be compromised by embolism from the
heart or aorta (40
–50%), thrombosis on underlying atheroma (25%), or
hypotension (25%). Vasculitis and venous occlusion are rare causes. Patients
usually have evidence of cardiac disease and arrhythmia.
Abdominal pain develops, which is more impressive than the physical findings.
In the early stages, the abdomen may be distended, with absent or diminished
bowel sounds, and peritonitis is a later feature.
Investigations reveal:
●
Leucocytosis.
●
Metabolic acidosis.
●
Raised phosphate and amylase.
●
‘Thumb-printing’ on AXR due to mucosal oedema.
●
An occluded or narrowed major artery on mesenteric or CT angiography
.

Management
Resuscitation, management of cardiac disease and IV antibiotic therapy
should be followed by laparotomy, embolectomy and vascular reconstruction.
In patients at high surgical risk, thrombolysis may sometimes be effective.
Survivors often develop short bowel syndrome requiring nutritional support,
sometimes including home parenteral nutrition, as well as anticoagulation.
Small bowel transplantation is promising in selected patients

Acute colonic ischaemia
The splenic flexure and descending colon lie in
‘watershed’ areas of
arterial supply. Arterial thromboembolism is usually responsible but colonic
ischaemia can also follow severe hypotension, colonic volvulus,
strangulated hernia, systemic vasculitis, aortic aneurysm
surgery or hypercoagulable states.
The patient is usually elderly and presents with sudden cramping left-
sided lower abdominal pain and rectal bleeding.
The diagnosis is established by colonoscopy within 48 hrs of onset.
Symptoms usually resolve spontaneously over 24
–48 hrs and healing
occurs within 2 wks.
Some have a residual fibrous stricture or segment of colitis.

Chronic mesenteric ischaemia
This results from atherosclerotic stenosis affecting at least two of the coeliac
axis, superior mesenteric and inferior mesenteric arteries.
Patients present with dull but severe mid- or upper abdominal pain ~30 mins
after eating, with weight loss and sometimes with diarrhoea.
Examination reveals generalized arterial disease and sometimes an audible
abdominal bruit.
Mesenteric angiography confirms at least two affected arteries.
Vascular reconstruction or percutaneous angioplasty is sometimes possible.
Left untreated, many patients develop intestinal infarction
