Rheumatology L7
Vasculitides constitute a spectrum of diseases characterized by inflammation & necrosis of blood vessels with resulting ischemia of those tissues supplied by the affected vessels. These are rare diseases & have late diagnosis.
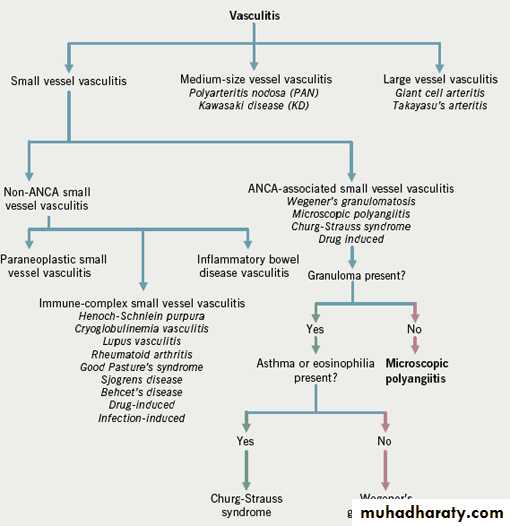
Chipell Hill Consensus Conference ((CHCC) Classification of Vasculitides 1994
Names for Vasculitides adopted by the 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitides. The items highlighted in red are changes or additions compared to the 1994 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitides..
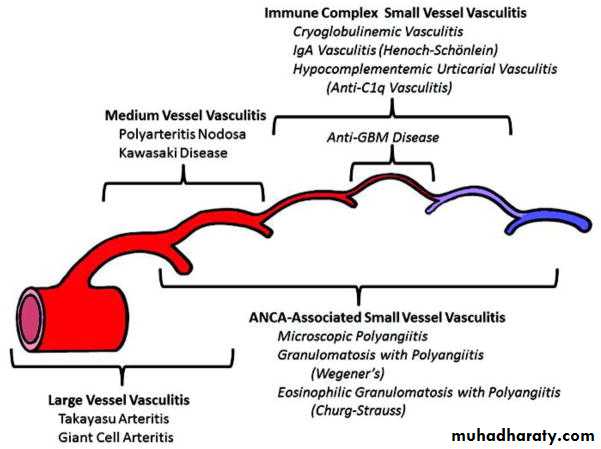
Large vessel vasculitis (LVV)
Takayasu arteritis (TAK)Giant cell arteritis (GCA)
Medium vessel vasculitis (MVV)
Polyarteritis nodosa (PAN)
Kawasaki disease (KD)
Small vessel vasculitis (SVV)
Antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV)
Microscopic polyangiitis (MPA)
Granulomatosis with polyangiitis (Wegener’s) (GPA)
Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) (EGPA)
Immune complex SVV
Anti-glomerular basement membrane (anti-GBM) disease
Cryoglobulinemic vasculitis (CV)
IgA vasculitis (Henoch-Schönlein) (IgAV)
Hypocomplementemic urticarial vasculitis (HUV) (anti-C1q vasculitis)
Variable vessel vasculitis (VVV)
Behcet’s disease (BD)
Cogan’s syndrome (CS)
Single-organ vasculitis (SOV)
Cutaneous leukocytoclastic angiitis
Cutaneous arteritis
Primary central nervous system vasculitis Isolated aortitis
Others
Vasculitis associated with systemic disease
Lupus vasculitis
Rheumatoid vasculitis
Sarcoid vasculitis
Others
Vasculitis associated with probable etiology
Hepatitis C virus–associated cryoglobulinemic vasculitis
Hepatitis B virus–associated vasculitis
Syphilis-associated aortitis
Drug-associated immune complex vasculitis
Drug-associated ANCA-associated vasculitis
Cancer-associated vasculitis
Others
Clinical classification of vasculitis: :
1- purpuric disorders= HSP, leukocytic vasculitis
2- microscopic polyarteritis= Polyarteritis nodosa
3- aortic type= Takayosu disease, polyarteritis nodosa(in the latter, the subclavian artery is spared ).
4- pulmonary type= Wegener's granulomatous, Churg- Strauss syndrome
GIANT CELL ARTERITIS(GCA)/ POLYMYALGIA RHEUMATICA
GCA also called temporal arteritis or cranial arteritis & this is the most common type of systemic vasculitis.GIANT CELL ARTERITIS(GCA)/ POLYMYALGIA RHEUMATICA
It especially involve branches of carotid artery of patients over the age of 50, often female patients.C/F : headache not responding to analgesia, scalp tenderness, visual disturbances, jaw claudication, arthralgia& monocular blindness which is irreversible. 90% of patients have high ESR.
Biopsy of a segment of temporal artery; reveals characteristic findings of inflammation & destruction of internal elastic lamina with GIANT cells present.
POLYMYALGIA RHEUMATICA(PMR)
Characterized by pain, stiffness of shoulders& hip girdles & proximal extremities. It also associated with high ESR& anemia.
It commonly occurs in female over 50 years.
Diagnosis is made on clinical grounds& rapid response to steroids.
PMR& GCA are likely part of same disease spectrum & some patients may have symptoms of both diseases.In GCA, corticosteroids treatment is obligatory because they significantly reduce the irreversible visual loss and other focal ischemic lesions, but much higher doses are needed than in PMR.
Treatment should not be delayed, especially if there have already been episodes of visual loss or stroke.
Starting doses of prednisolone are:-
PMR: 10-15 mg as a single dose in the morning.GCA: 60-100 mg, usually in divided doses.
The dose should be reduced gradually in weekly or monthly steps.
Calcium and vitamin D supplement and sometimes bisphosphonates are necessarily needed to prevent osteoporosis while high dose of steroids are given. In PMR, the response appears in a matter of few days.
The outcome of both disease is excellent , but relapse may occur during treatment or years after cessation of treatment.
TAKAYASU'S ARTERITIS is a large vessel disease that affect young female but can be seen in both male & female up to the age of 50. It also known as pulseless disease.
TA results in stenosis of aorta & its branches like cerebral , brachiocephalic, renal , mesenteric , femoral & coronary arteries.
Stenosis of proximal aorta& its proximal branches is the most common finding.
Clinically limb claudication , lightheadedness, malaise, fever & arthralgia , all are experienced by such patients. There was a delay in diagnosis for years even if the stenosis is sever because most patients are asymptomatic.
Diagnosis is made by angiography. Treatment includes chronic steroids. Some patients may respond to immunosuppressive drugs like methotrexate& cyclophosphamide. Some patients require corrective vascular angioplasty.
POLYARTERITIS NODOSA(PAN) is a medium vessel inflammatory vasculitis involving segmental necrotizing lesions often at arterial branch points leading to stenosis, thrombosis, hemorrhage or infarction of the involved artery.
Classical PAN is rare condition which, unlike other vasculitic diseases, usually occurs in middle-age men. It is accompanied by sever systemic manifestations, and its occasional association with hepatitis B antigenaemia suggest a vasculitis secondary to the deposition of immune complexes.
Pathologically, there is fibrinoid necrosis of vessel walls with microaneurysm formation, thrombosis and infarction.
CLINICAL FEATURES::
These include fever, malaise, weight loss and myalgia. These initial symptoms are fallowed by dramatic acute features that are due to organs infarction.* Neurological features- mononeuritis multiplex
* Abdominal pain due to arterial involvement of abdominal viscera, mimicking acute cholecystitis, pancreatitis and appendicitis.* Renal- presents with hematuria and proteinuria. Hypertension and acute /chronic renal failure occur.
* Cardiac- Coronary arteritis causes myocardial infarction and heart failure.
* Skin –subcutaneous hemorrhage and gangrene occur.* Lung involvement is rare.
INVESTIGATIONS::
-blood count. Anemia, leukocytosis and high ESR.* biopsy of involved artery.
-angiography. Demonstrate microaneurysms in hepatic, intestinal or renal vessels.
Most patients are undiagnosed until postoperatively for ischemic events.
TREATMENT::-
Corticosteroid usually in combination with immunosuppressive drugs such as azathioprine. The use of antiviral drugs in patients with positive serology of hepatitis B&C is promising.
Churg-Strauss syndrome also known as allergic granulomatosis& agiitis& this is a medium & small vessel vasculitis that has extravascular manifestations which can distinguish it from other types of vasculitis.
The typical presentation is a middle age person with chronic asthma who develops pulmonary infiltrates, vasculitis& eosinophilia. The vasculitis involves the skin, peripheral nerves& GIT, but other organs may be affected.
Biopsy shows microgranulomas& eosinophilic deposits. The pulmonary infiltrates are patchy but rapidly resolve with steroid treatment.
Recent reports showed that anti-leukotriene drugs used in treatment of asthma may cause CSS.
Diagnosis is made depending on clinical findings but biopsy is often needed. Eosinophilia is present in almost all patients but rapidly returns to normal on giving steroids. Anti-neuotrophil cytoplasmic auto antibodies(P-ANCA) are positive in most patients.
Treatment is based on steroids, but immunosuppressive drugs may be needed in some patients. The prognosis is fairly good but relapse rate is common.
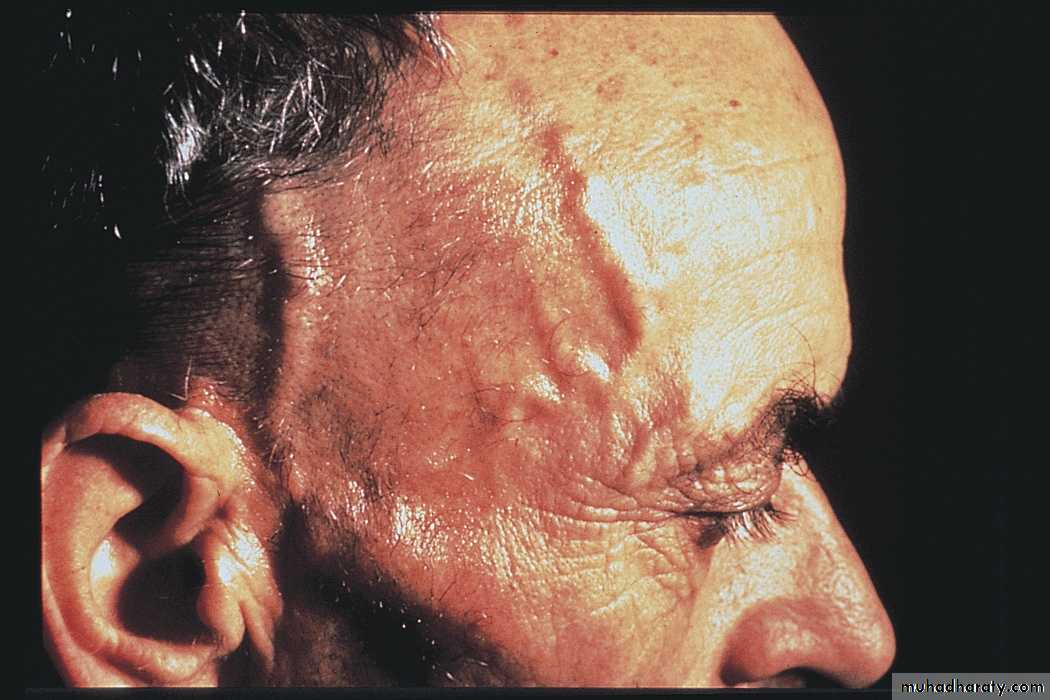
WEGENER'S GRANULOMATOSIS(WG)
small& medium vessel vasculitis with many extra vascular manifestations. Although any anatomic area can be affected, the three most common sites of involvement are : the sinuses& upper airways, the lungs, & the kidneys.Face Involvement
The patients may only diagnosed after months or years of subtle symptoms. However WG can be presented with alveolar hemorrhage & or rapidly progressive GN, both of which account for much of the mortality from the disease.Destruction of nasal sinus tissues may result in facial deformities. Pseudo tumor can occur everywhere but commonly in lungs & retro orbital spaces. Skin , peripheral nerves & eye involvement are common.
Diagnosis is made on tissue biopsy. ANCA of C-ANCA(cytoplasmic) is positive in 90% of patients with renal disease&70% without renal disease. P-ANCA also can be found.
The mortality of untreated WG approaches 100%.
Treatment is steroids, but this is inadequate. Therefore combination with immunosuppressive drugs cyclophosphamide & methotrexate is helpful. Relapse is common.
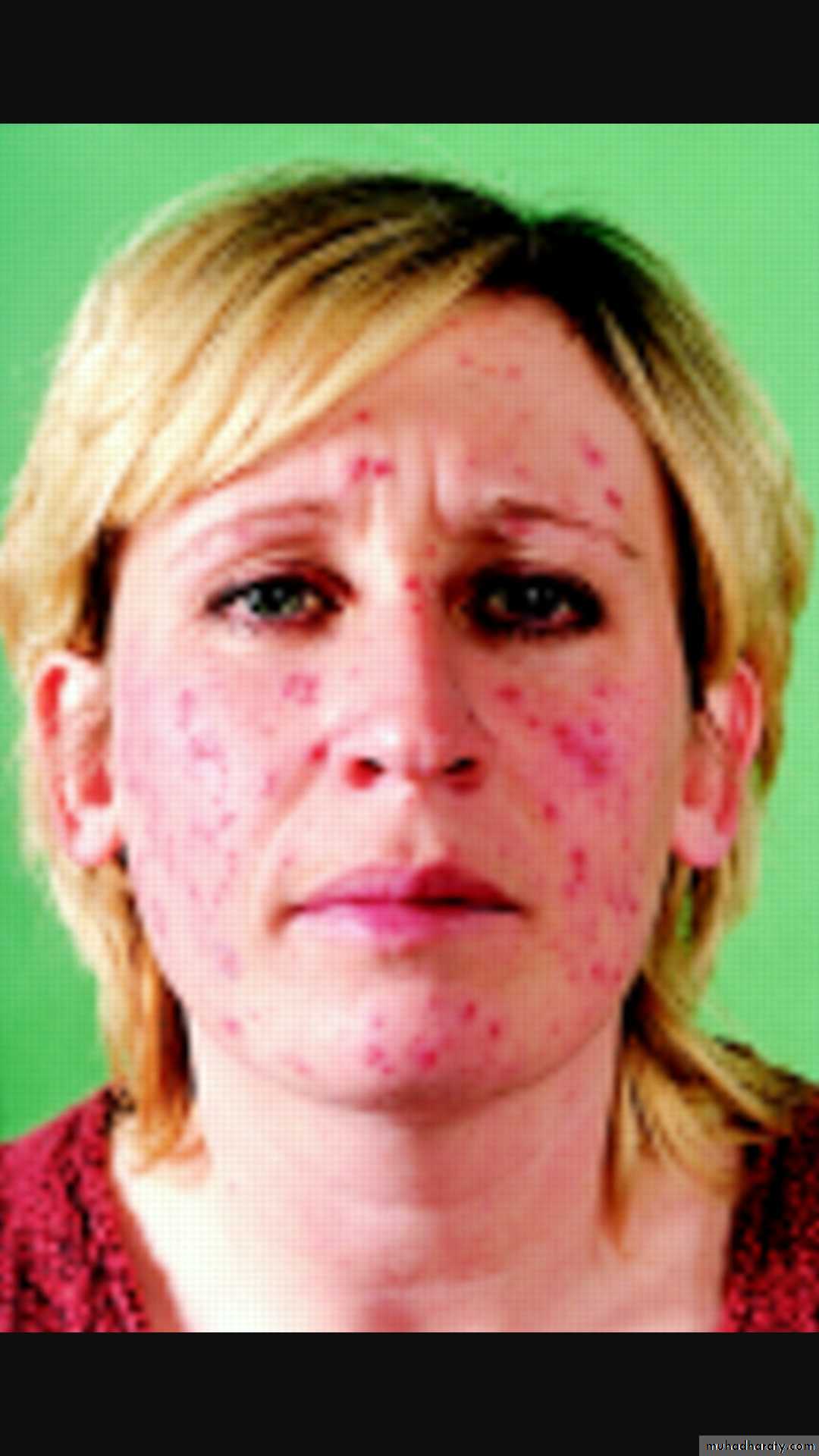
HENOCH SCHONLEIN PURPURA(HSP)
is a small vessel vasculitis affecting children & young adults. Classical clinical triad of palpable purpura at buttocks, arthritis& abdominal pain is found in 80% of patients.HENOCH SCHONLEIN PURPURA(HSP)
Fever & glomerulonephritis are also common. Affected vessels have IG &complement deposition& serum IgA is often elevated. IgA deposition in renal lesions is characteristic. Diagnosis is confirmed depending on clinical & laboratory findings.Although patients with HSP may develop bowel perforation or significant renal disease, the majority improve without sequelae. Most patients improve within weeks or months.
Ddx: drug induced purpura, SLE, gonococcal arthralgia, keratoderma blennorhagica& secondary syphilis.
Treatment is supportive with NSAIDs & analgesia.
Steroids are kept for more symptomatic patients. Those with chronic renal diseases require steroids & immunosuppressive drugs.
***********