Anatomy of the thorax
Chest wall and pleura:the chest wall is covered by the pectoralis muscles anteriorly and the latissimus dorsi and serratus anterior muscles posterolaterally. In an anterior thoracotomy, the fibers of the pectoralis major are split, exposing the intercostal muscles. In the standard posterolateral thoracotomy, the latissimus dorsi is divided, and then the serratus anterior is divided . From the standpoint of preservation of normal chest wall mechanics, an anterior thoracotomy is usually better tolerated; however, exposure and control of intrathoracic structures are often better accomplished through the posterolateral approach, which is the standard thoracotomy incision.
There are 12 pairs of ribs, 7 of which are true ribs and 5 of which are false ribs. True ribs have costal cartilage that directly articulates with the sternum. False ribs do not. The eleventh and twelfth ribs are called floating ribs because they are not attached anteriorly
The sternum is divided into the manubrium, the body, and the xiphoid. The clavicle articulates with the sternum and the first costal cartilage.
Muscles of the intercostal space are the external, internal, and transversus thoracic muscles. There are 11 intercostal spaces. Each intercostal space contains a vein, an artery, and a nerve, which course along the lower edge of the rib. All the intercostal spaces are wider anteriorly than posteriorly, the widest being the third.
The lower border of the pectoralis major muscle forms the anterior axillary fold. The tendon of the latissimus dorsi forms the posterior axillary fold .
The parietal pleura is divided into four parts: costal, cervical, diaphragmatic, and mediastinal. The costal pleura lines the ribs, cartilages, and vertebral bodies and is the thickest portion of the parietal pleura.
The visceral pleura covers the lungs so firmly
The intercostal neurovascular bundle:
In the plane between the innermost intercostal muscle and outer two layers (external and internal intercostal muscles) runs the neurovascular bundle. From above downward the order is vein, artery, and nerve (VAN). They are protected by the downward projection of the lower border of the ribThe intercostal nerves:
Are mixed spinal nerves formed from a dorsal and a ventral root, the dorsal root being sensory and the ventral root containing somatic motor neurons
The intercostal arteries:
Two sets of intercostal arteries, the posterior and the anterior, are responsible for supplying the intercostal spaces
The posterior intercostal arteries are branches of the descending thoracic aorta except in the first two spaces where they are branches of the supreme intercostal artery, given off by the costocervical trunk of the second part of the subclavian artery.
The anterior intercostal arteries are branches of the internal thoracic arteries from the first part of the subclavian artery
The anterior intercostal arteries are smaller than the posterior intercostal arteries with which they anastomose
The intercostal veins:
In each space there is one posterior and two anterior intercostal veins
The anterior veins drain into the musculophrenic and internal thoracic veins.
The vein of the first space (called supreme intercostal vein), posteriorly, drains to the brachiocephalic, vertebral, or superior intercostal vein.
The superior intercostal vein is formed by the posterior intercostal veins of the second, third, and sometimes the fourth spaces. This drains into the azygos vein on the right side and on the left side open into the left brachiocephalic veins
Lymphatic drainage of the chest wall:
There are three upgoing lymph channels on each side of the thoracic cavity, and they freely communicate with each other.
They are the right and left parasternal, and bronchomediastinal trunks (alongside the trachea),
the thoracic duct, and
the right lymphatic duct
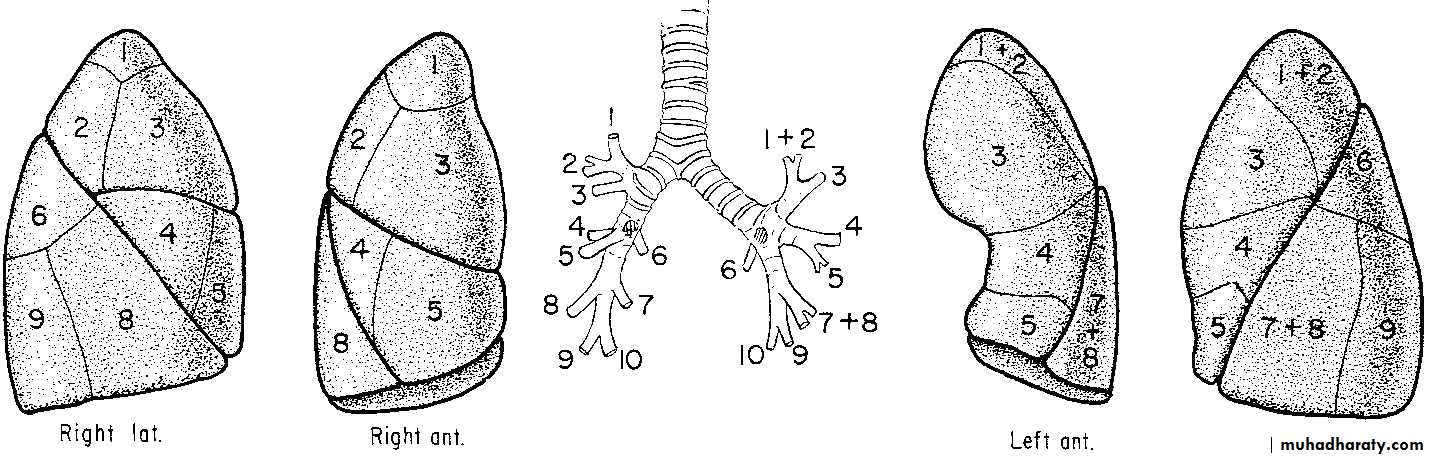
Lung Lobes And Fissures And Bronchopulmonary Segment Anatomy:
With the bronchus at the center, each bronchopulmonary segment functions as an individual unit with its own pulmonary arterial and venous supply.
The larger right lung has three lobes—upper, middle, and lower—and is composed of 10 bronchopulmonary segments. The left lung has two lobes and 8 segments
Left
RightUpper lobe
Upper lobe
1 and 2. Apical posterior
1. Apical
3. Anterior
2. Posterior
3. Anterior
Lingula
Middle lobe
4. Superior lingula
4. Lateral
5. Inferior lingula
5. Medial
Lower lobe
Lower lobe
6. Superior
6. Superior
7 and 8. Anteromedial basal
7. Medial basal
8. Anterior basal
9. Lateral basal9. Lateral basal
10. Posterior basal
10. Posterior basal
Chest Trauma
The chest contains the two most vital of the life sustaining organs; the heart and the lung. Therefore any injury to the lung that seriously compromise the function of these organs is threat to life. Many of these injuries are lethal (on spot) or within a short period of time, death often occurs rapidly. Yet even in this critical situation the lives of over 80% of patients can be saved with the prompt application of possible measures.Types of trauma:
Non penetrating trauma
Blunt trauma
Crushing injury
Compression injuries: e.g.:
Crushing the chest wall between two blunt objects
The impaction of the driver against his steering wheel
Fall of a heavy object on the chest
Penetrating and perforating injuries
penetrating wound is a wound with site of entry and no site of exit
perforating wound is a wound with an entry and exit
A- War injuries: like pistol bullet, riffle bullet and fragments from bombs or shells
B- Civilian injuries: like knives and sharp instruments
Potentially Acutely Lethal Injuries of the Chest and Their Management
ManagementInjury
Tube thoracostomy
• Tension pneumothorax
Tube thoracostomy, operative repair
• Massive hemothorax
Pericardiocentesis, operative repair
• Cardiac tamponade
Operative repair
• Deceleration aortic injury
Intubation, pain control, fluid restriction
• Massive flail chest with pulmonary contusion
Intubation, airway, bronchoscopy
• Upper and lower airway obstruction
Bronchoscopy, operative repair
• Tracheobronchial rupture
Diagnostic tests:
This should be present in the ER of most hospitals
Chest Imaging:
CXR:
Fractures of the bony thorax,
Pneumothorax, hemothorax, or pulmonary contusion.
Mediastinum widening, pneumomediastinum, or shifting.
Subcutaneous air or foreign bodies.
width of the cardiac silhouette tamponade.
CT scan: should not be performed in the severely hemodynamically unstable patient or in the presence of life-threatening injuries. However,
It may reveal injuries not seen clearly on plain radiographs, such as aortic disruption, pneumothorax, pneumomediastinum, and hemothorax.
It may be useful to screen all patients with blunt trauma and
Evaluate unusual or abnormal findings on initial chest X-ray (e.g., diaphragmatic injuries).
Echocardiography:
Focused Assessment for the Sonographic evaluation of the Trauma patient, or FAST examination
Angiography:
Angiography remains the gold standard in the diagnosis of aortic transection or injuries to the great vesselsIndications for angiographic studies for potential thoracic injuries:
High-speed deceleration injuries
Chest X-ray findings :
Widened mediastinum
Loss of aortic knob shadow
Tracheal or esophageal deviation to the right
Downward displacement of left mainstem bronchus
Fractured first rib, sternum, or scapula Multiple rib fractures or flail chest
Massive hemothorax
Upper extremity hypertension
Unexplained hypotension
Pulse deficits
Systolic murmur
Conditions demanding early thoracotomy
are less than 10%:
1-Continuing intrathoracic hemorrhage
2-Uncontrollable air leak
3-Wounds of the heart
4-Widening of the mediastinum
5-Large chest wall defects
6-Esophageal injuries
7-Massive hemoptysis
8-Cardiac tamponade
9-Ruptured diaphragm
10-Gross pleural contamination with foreign body
Thoracic injuries
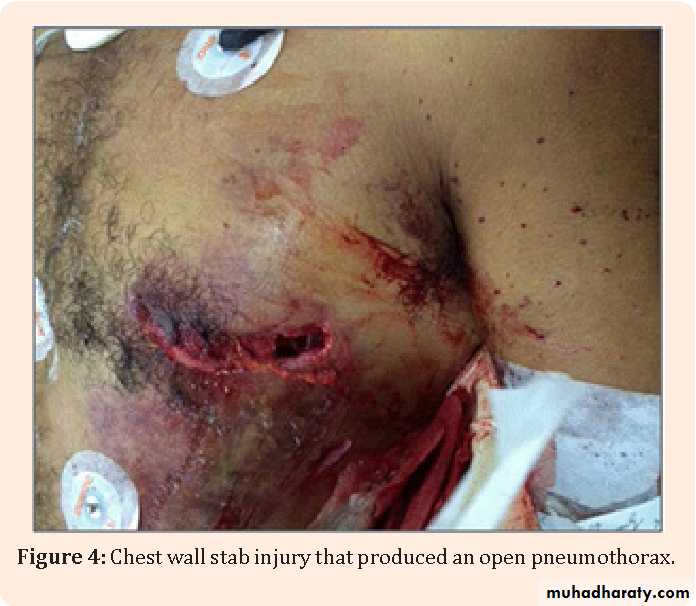
Chest wall injuryOpen sucking wound (open pneumothorax)
Fracture rib
Simple fracture
Multiple fractures
Stove in chest
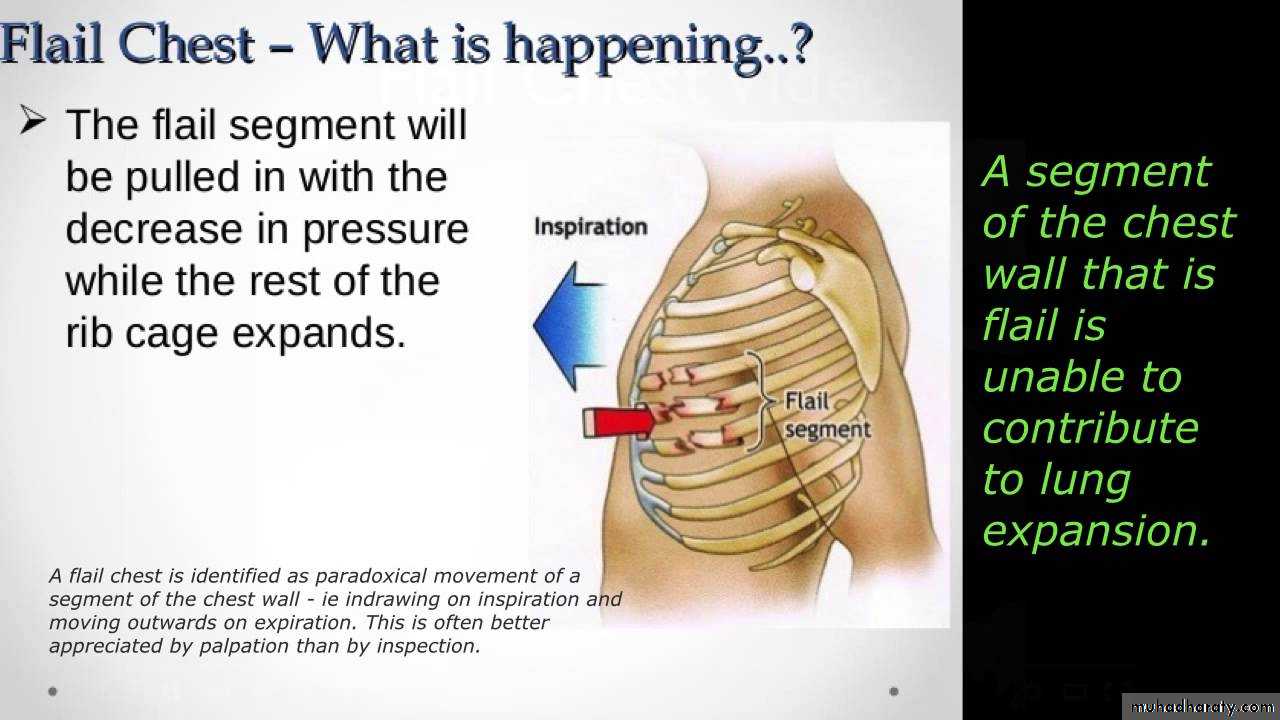
Flail chest
Pleural injuries:
Pneumothorax
Hemothorax
Empyema
Lung injuries:
Lacerations
Wet lung
Stiff lung
Shocked lung
:
Cardiac injury:
Cardiac tamponade
Aortic injury
Traumatic rupture
Traumatic aneurysm
Esophageal injury.
Diaphragmatic injury:
Rupture
tear.
Blast injuries.
Chest wall injuries:
Open pneumothorax:Causes: gun fire, blast, explosion
Manifestations: this will result in sucking wound of the chest wall and there may or may not be associated injury to the intrathoracic structures. The defect in the chest wall allows air to enter the pleural space during inspiration causing collapse of the lung and the process is reversed in expiration.
Treatment:
First aid station: the aim is to convert open Pneumothorax to a close one. This is done by:
Covering the wound with gauze and elastic adhesives
Insertion of intercostals tube attached to underwater seal.
In hospital: after relieving respiratory distress and treating shock. The following lines of treatment should be followed:
General anesthesia
Limited thoracotomy
Debridement
Control bleeding
Deal with other injuries
Chest drain and closure.
Minimal Pneumothorax:
This requires no active treatment. The air will be absorbed and the lung re-expand fully in days – weeks providing that contamination and lung injury are minimal.Massive Pneumothorax:
This is treated by tube thoracostomy
Occasionally one find evidence of continuous leakage of large volume of air with failure of the lung to remain expanded despite adequate pleural decompression by suction. In this situation one should think of ruptured bronchus or injury to trachea. This can be confirmed by bronchoscopy and immediate thoracotomy is essential
Tension Pneumothorax:
Massive pneumothorax may become tension pneumothorax, shock usually follows. The large intrapleural pressure does not only collapse the ipsilateral lung and obstruct venous return to the heart but also partially compress the contralateral lung.Decompression of pleura for pneumothorax can be done by:
insertion of a wide bore needle into the pleural space. (The practice of attaching intrapleural wide bore needles to under water seal should not be done because the needle itself will cause more damage when the lung expands.)
Tube thoracostomy connected to underwater seal is the best effectively remove blood and air.
If despite efficient large volume suction the lung fail to reexpand or the patient is losing more air from his chest with every breath. A large air leak from ruptured bronchus should be suspected.
In spontaneously ventilating patients, the chest tube may be removed when:
Lung fully expanded
No air leak
Any sudden change in cardiovascular or respiratory status in a previously stable patient is in most cases due to tension pneumothorax secondary to blocked tubes
Fracture of ribs:
Causes: usually blunt non penetrating injury.
Types:
Simple fracture: this is an isolated fracture usually occurring at the outer convexity. As the fracture is not displaced, so there is no lung injury.
Multiple rib fractures: the ribs fracture at site of maximal curvature i.e., at the posterior and anterior angles. Tear in the lung lead to hemo or pneumothorax.
Stove in chest: when multiple or single rib fracture produce a segment in the chest wall that is permanently indented, i.e., portion of the thoracic cage is depressed.
Flail chest: when the multiple ribs fractured produce a flaccid unstable segment exhibiting paradoxical movement in which the flail area is sucked inwards during inspiration and pushed out in expiration
Clinical manifestations:
pain, local tenderness, paradoxical movement, sputum reduction, and pneumothorax or hemothorax or both.Treatment:
Simple fracture: a. analgesia, b. intercostal nerve block, c. strapping, d. encourage cough.
Multiple fractures: a. analgesia, b. O2, c. blood, d. tube thoracostomy, e. relieve airway obstruction, f. stabilization of chest wall.
Treatment of flail chest:
Aim of treatment:
Establishing and maintaining a clear airway (endotracheal tube or tracheostomy).
Restoring and maintaining a stabilized chest wall by:
External immobilization
Traction
Internal fixation
IPPV
Drainage of pleural cavity and maintaining an expanded lung by tube thoracostomy.
Conservative treatment (External immobilization):
Pain relief, with close observation and hourly blood gas analysis.Stabilization of the fractured segment by
Applying stabilizing pressure dressing over the involved segment of the chest wall as adhesive tape strapping
Turning the patient on the injured side.
Placing a sand bag on the injured site.
Holding palm of hand on the injured site.
Advantages: Can be done at accident site and during hospitalization.
Disadvantages: impair ventilation and impair cough mechanism pneumonia due lower airway obstruction and atelectasis.
Surgical treatment: fixation
Mechanical ventilator
Hemothorax:
Hemothorax and pneumo-hemothorax suggest far more serious situation than pneumothorax :Causes: may be due to injury to the heart, great vessels, intercostal vessels and internal mammary vessels.
Treatment:
Minimal hemothorax (blood in the pleural cavity is less than 300 cc) can be left without drainage (observation only) and will be absorbed in about 10 days.
Moderate hemothorax can be treated by thoracocenthesis but if pneumothorax is also present tube thoracostomy is needed.
Massive hemothorax treated by restoration of the circulation volume, tube thoracostomy, and then thoracotomy
Tracheobronchial injuries:
Mainly due to penetrating injuries and rarely due to blunt ones.
It leads to:
Tracheal laceration.
Tracheal rupture.
Bronchial rupture.
Mechanism of blunt injury:
Forceful antero-posterior compression of the thoracic cage (dashboard injury)
A consequence of high airway pressures
Rapid deceleration.
Manifestations:
respiratory distress,
dyspnea,
hemoptysis
air leak pneumothorax, mediastinal emphysema... etc.
Hoarseness or dysphonia
Cardiac Tamponade: (a two edged sword)
The victim who lives long enough to reach the hospital is frequently alive because of cardiac tamponade which prevent hemorrhage. Were if not for the pericardial sac, practically all wounds of the heart would present a hopeless situation because of blood loss. Tamponade is therefore both lethal and life saving up to a point. It contributes to the reduction of hemorrhage from the cardiac wounds but beyond that point a continuation of its action produces profound shock which prove fatal unless promptly relieved.The two major immediate cause of death following knife or bullet wounds of the heart were either bleeding or cardiac tamponade or combination of both.
Acute cardiac tamponade result in three physiological effects:
On the venous side:
The increased intrapericardial pressure restricts venous return to the heart resulting in an elevated central venous pressure.
On the arterial side:
The resultant cardiac compression reduces cardiac output, BP, and coronary blood flow myocardial hypoxia and failure.
On the systemic side:
The reduced cardiac output initially leads to generalized vasoconstriction peripheral vascular resistance maintenance of normal BP during the early stage of the tamponade despite a progressively falling cardiac output and a progressively rising venous pressure
Presentation:
Shock
heart sounds
BP
Venous distention
CXR: wide mediastinum (large heart )
Treatment:
Airway management with endotracheal intubation,
Establishment of intravenous access capable of massive volume resuscitation,
Immediate thoracotomy through a left anterolateral approach using a fourth interspace incision with extension across the sternum to the right side of the chest, if necessary. This approach allows rapid exposure of the heart and the ability to relieve tamponade from hemorrhage. In addition, it allows the surgeon the ability to perform open heart massage, control cardiac injuries, cross-clamp the descending aorta to preferentially perfuse the brain and coronary arteries, and allow volume resuscitation in the setting of shock.
Diaphragmatic injuries:
Causes: both penetrating and blunt trauma. The diaphragm may burst without any obvious external wound like crushing between a wall and a car, compression of the abdomen, compression of the lower costal cartilage…etc. mostly seen in the left diaphragm as the right is protected by the liver.Resulting in: diaphragmatic hernia
Manifestations:
Penetrating injuries: the injury to the abdomen or chest predominate and the diaphragm should always be checked during laparotomy or thoracotomy.
Blunt trauma: diaphragmatic injury may be over looked especially when not associated with other injuries and the patient may be presented late with diaphragmatic hernia.
Investigations:
CXR _ chest CT
Ba – swallow
Treatment:
Thoracotomy
Reduction of abdominal contents
Closure of diaphragm
THANKS FOR YOUR PATIENCY