Small and large intestine
ANATOMY OF THE SMALL AND LARGEINTESTINESSmall intestineThe small intestine starts at the pylorus and extends to the ileocaecal valve. It is approximately 7 m in length and is divided into the duodenum, jejunum and ileum. Its main function is in thebreakdown and absorption of food products. The small bowel ispresent in the central and lower portion of the abdominal cavity.Its relations consist of the greater omentum and abdominal wallanteriorly. Posteriorly, it is fixed to the vertebral column by way ofits mesentery.The duodenum is present proximally and is about 25 cm inlength. It has no mesentery and, therefore, is the most fixed partof the small bowel.It merges into the jejunum at the duodenojejunalflexure. The remainder of the small bowel is made up ofthe jejunum and ileum. The jejunum makes up the proximal twofifths and is wider, thicker and more vascular than the ileum. It consists of circular folds of mucous membrane (valvulae conniventes) that can be used to distinguish it from the ileum. The ileum contains larger lymph node aggregates (Peyer’s patches and these can sometimes be lead points in cases of intussusception in the young.
The arterial supply of the duodenum consists of the right gastric,the superior pancreaticoduodenal branch of the hepatic artery and the inferior pancreaticoduodenal branch of the superior mesenteric artery. The veins drain into the superior mesenteric. The nerves are supplied from the coeliac plexus. The jejunum and ileum are vascularised by the superior mesenteric artery through a rich plexus of vessels. The veins run a similar course. The nerve supply to the small intestines arises from sympathetic nerves around the superior mesenteric artery. Pathology such as obstruction causes visceral pain, which is felt in the peri-umbilical region.
Large intestineThe large intestine extends from the ileum to the anus. The colon is approximately 1.5 m in length. It is relatively more fixed than the small bowel It also differs in that it possesses appendices epiploicae on its surface, which are peritoneal folds containing fat, and the presence of taenia, which consist of longitudinal bands of the outer muscle coat. It can be divided into the caecal, ascending, transverse, descending and sigmoid colonic segments.
The blood supply of the colon is derived from ileocolic, rightcolic and middle colic branches of the superior mesenteric vessels.The descending colon receives its blood supply from the leftcolic branch from the inferior mesenteric but also communicateswith the superior mesenteric system via the marginal artery ofDrummond. The veins run in a similar distribution. The nervesupply is derived from the sympathetic plexus surrounding thesuperior and inferior mesenteric arteries. Visceral pain is felt inthe peri-umbilical region in the proximal colon and in thehypogastric region in the distal colon.
FUNCTIONAL ABNORMALITIESMegacolon and non-megacolon constipationThere is no single definition of constipation; however, a bowelfrequency of less than one every 3 days would be consider abnormal by some. This group of conditions can be dividedinto:1 megacolon:a Hirschsprung’s disease;b non-Hirschsprung’s megarectum and megacolon;2 non-megacolon:a slow transit;b normal transit.
Idiopathic megarectum and megacolonThis is a rare condition and the cause is not known, although insome it may result from poor toilet training during infancy and inothers from a congenital abnormality of the intestinal myentericplexus.Clinical featuresIt presents usually in the first 20 years with severe constipation.Patients with idiopathic megarectum often present with faecalincontinence due to rectal faecal loading that requires manualevacuation. Patients with megacolon are more likely to presentwith abdominal distension and pain. On clinical examination,there may be a hard faecal mass arising out of the pelvis and, onrectal examination, there is a large faecaloma in the lumen. Theanus is usually patulous, perianal soiling is common, and sigmoidoscopy is usually impossible.
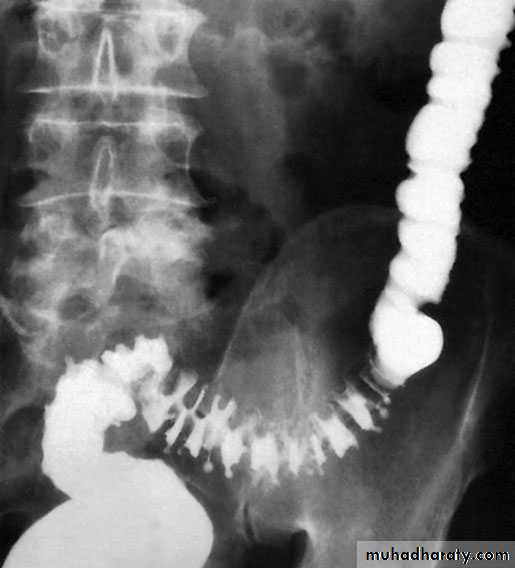
InvestigationImagingAs there is an enlarged rectum, often with distension of the colon over a variable length, a radiograph should be taken without prior bowel preparation, using a small quantity of water-soluble contrast to prevent barium impaction. There is usually gross faecal loading of the enlarged rectum and colon and, when a contrast examination is carried out, the width of the colon measured at the pelvic brim is usually more than 6.5 cm.
Anorectal physiology testsAnorectal physiology tests demonstrate delayed first sensationand raised maximum tolerated volume. Full-thickness rectal biopsy shows normal ganglion cells, a finding that definitively distinguishes this condition from Hirschsprung’s disease.
Medical treatmentThis is directed at emptying the rectum and keeping it emptywith enemas, washouts and sometimes manual evacuation under anaesthesia. Thereafter, the patient is encouraged to develop a regular daily bowel habit, with the use of osmotic laxatives to help the passage of semiformed stool.
Surgical treatmentSurgical treatment is sometimes necessary if medical therapy fails.Options that are available include:1 resection of the dilated rectum and colon back tonormal-diameter colon with normal ganglion cells confirmedby frozen section at the time of surgery, which is followed byreconstruction with a coloanal anastomosis;2 colectomy with the formation of an ileorectal anastomosis;3 restorative proctocolectomy;4 vertical reduction rectoplasty, which is a new procedure designed to reduce the volume of the rectum by at least 50%.5 stoma formation, which may be used either as a salvage operation for failure of previous surgery or as a primary intervention.
Non-megacolon constipation These are usually otherwise healthy individuals who seek help for constipation but eat a normal diet and have a normal colon on endoscopy and barium enema.Its cause is thought to involve slow whole-gut transit or arectal evacuation problem. Factors influencing bowel transit timeinclude:• drugs: opiates, anti-cholinergics and ferrous sulphate;• diseases: neurological conditions (Parkinson’s disease, multiplesclerosis and diabetic nephropathy):– hypothyroidism;– hypercalcaemia.
InvestigationWhole-gut transit time can be measured by asking the patient tostop all laxatives and take a capsule containing radio-opaquemarkers . Retention of more than 80% of the shapes,120 hours after ingestion, is abnormal.
TreatmentThis can be done in several ways:1 Dietary fibre. This is the first-line treatment for people withmild constipation. Constipation only resolves after severalweeks of therapy .2 Laxatives. It is important that patients do not fall into a cycleof laxative abuse. A number of types are available whichinclude bulk, osmotic and stimulant agents.3 Biofeedback. This involves conditioning and coordination ofthe abdominal and pelvic compartments. It has been shown tobe effective in those with a rectal evacuation problem.
VASCULAR ANOMALIES(ANGIODYSPLASIA)Capillary or cavernous haemangiomas are a cause of haemorrhagefrom the colon at any age. In the middle-aged or elderlypatient, haemangioma needs to be distinguished from other causes of sudden massive haemorrhage, such as diverticulitis, ulcerative colitis (UC) or ischaemic colitis. Angiodysplasia is a vascular malformation associated with ageing. Its true incidence is from 5 to 25% over the age of 60 years. Angiodysplasias occur particularly in the ascending colon and caecum of elderly patients. The malformations consist of dilated tortuous submucosal veins and, in severe cases, the mucosa is replaced by massive dilated deformed vessels.
Clinical featuresIn the majority, the symptoms are subtle and patients can present with anaemia. About 10–15% can have brisk bleeds, which may present as melaena or significant per rectum bleeding that is often intermittent.There is an association with aortic stenosis. Heyde’s syndrome describes the association of aortic valve stenosis with gastrointestinal bleeding from colonic angiodysplasia. A mild form of von Willebrand’s disease has been thought to be involved.
Investigation-Barium enema is usually unhelpful and should be avoided, because it may mask the lesion at subsequent endoscopy. -colonoscopy may show the characteristic lesion in the right colon. The lesions are only a few millimetres in size and appear as reddish, raised areas at endoscopy. ‘Pill’ endoscopy is a relatively new technology that may detect small bowel lesions. -Selective superior and inferior mesenteric angiography shows the site and extent of the lesion - a radioactive test using technetium-99m(99mTc)-labelled red cells may confirm and localise the source ofhaemorrhage.
TreatmentThe first principle is to stabilise an unstable patient. Followingthis, the bleeding needs to be localised by colonoscopy. Thisallows simple therapeutic procedures such as cauterisation to becarried out. In severe uncontrolled bleeding, surgery becomesnecessary. On-table colonoscopy is carried out to confirm the site of bleeding. Angiodysplastic lesions are sometimes demonstrated by transillumination through the caecum . If it is still not clear exactly which segment of the colon is involved, then a total abdominal colectomy with ileorectal anastomosis may be necessary.
BLIND LOOP SYNDROME if a blind loop of the small intestine is made referred to as the blind loop syndrome.Essentially, the stasis produces an abnormal bacterial flora,which prevents proper breakdown of the food (especially fat) and mops up the vitamins that are present. Sometimes, the only manifestation is anaemia, resulting from vitamin B12 deficiency but, if steatorrhoea occurs, other serious malabsorption features follow. In general, high loops produce steatorrhoea, whereas lowloops tend to produce anaemia.
Temporary improvement will follow the use of antibiotics todestroy the bacteria causing the trouble, but the main treatmentis surgical excision of the cause of the stasis where applicable.
DIVERTICULAR DISEASETypesDiverticula can occur in a wide number of positions in the gut,from the oesophagus to the rectosigmoid. There are two 1- Congenital. All three coats of the bowel are present in the wall of the diverticulum, e.g. Meckel’s diverticulum.2- Acquired. The wall of the diverticulum lacks a propermuscular coat. Most alimentary diverticula are thought tobe acquired.varieties:
Duodenal diverticulaThere are two types:1 Primary. Mostly occurring in older patients on the inner wallof the second and third parts , these diverticulaare found incidentally on barium meal and are usuallyasymptomatic.2 Secondary. Diverticula of the duodenal cap result from longstanding duodenal ulceration .
Jejunal diverticulaThese are usually of variable size and multiple (Fig. 65.8).Clinically, they may (1) be symptomless, (2) give rise to abdominalpain, (3) produce a malabsorption syndrome or (4) presentas an acute abdomen with acute inflammation and occasionallyperforation. In patients with major malabsorption problemsgiving rise to anaemia, steatorrhoea, hypoproteinaemia orvitamin B12 deficiency, resection of the affected segment withend-to-end anastomosis can be effective.
Meckel’s diverticulumMeckel’s diverticulum is present in 2% of the population; it issituated on the anti-mesenteric border of the small intestine,commonly 60 cm from the ileocaecal valve, and is usually3–5 cm long. Many variations occur (2% – 2 feet – 2 inches is auseful aide-mémoire) . It represents the patent intestinal end of the vitellointestinal duct
A Meckel’s diverticulum possesses all three coats of the intestinal wall and has its own blood supply. It is therefore vulnerable to infection and obstruction in the same way as the appendix. indeed, when a normal appendix is found at surgery for suspected appendicitis, a Meckel’s diverticulum should be sought by inspection of an appropriate length of terminal ileum. In 20% of cases, the mucosa contains heterotopic epithelium, namely gastric, colonic or sometimes pancreatic tissue. In order of frequency, these symptoms are as follows:
1 Severe haemorrhage, caused by peptic ulceration. Painlessbleeding occurs per rectum and is maroon in colour.2 Intussusception.In most cases, the apex of the intussusceptionis the swollen, inflamed, heterotopic epithelium at the mouthof the diverticulum.3 Meckel’s diverticulitis may be difficult to distinguish from thesymptoms of acute appendicitis. When a diverticulum perforates, the symptoms may simulate those of a perforated duodenal ulcer. At operation, an inflamed diverticulum should besought as soon as it has been demonstrated that the appendixand fallopian tubes are not involved.
4 Chronic peptic ulceration. As the diverticulum is part of themid-gut, the pain, although related to meals, is felt around theumbilicus.5 Intestinal obstruction. The presence of a band between the apex of the diverticulum and the umbilicus may cause obstruction either by the band itself or by a volvulus around it.
ImagingMeckel’s diverticulum can be very difficult to demonstrate bycontrast radiology; small bowel enema would be the most accurate investigation. Technetium-99m scanning may be useful in identifying Meckel’s diverticulum as a source of gastrointestinal bleeding.
‘Silent’ Meckel’s diverticulum.A Meckel’s diverticulum usually remains symptomless throughout life and is found only at necropsy. When a silent Meckel’s diverticulum is encountered in the course of an abdominal operation,it can be left provided it is wide mouthed and the wall ofthe diverticulum does not feel thickened. Where there is doubtand it can be removed without appreciable additional risk, itshould be resected.Exceptionally, a Meckel’s diverticulum is found in an inguinalor a femoral hernia sac – Littre’s hernia.
Meckel’s diverticulectomyA Meckel’s diverticulum that is broad based should not be amputated at its base and invaginated in the same way as a vermiform appendix due to risk of stricture
diverticular disease of Colon IntroductionThe prevalence of diverticular disease in the western world is60% over the age of 60 years. The condition is found in thesigmoid colon in 90% of cases, but the caecum can also beinvolved and, on occasion, the entire large bowel can be affected. The main morbidity of the disease is due to sepsis.AetiologyDiverticula of the colon are acquired herniations of colonicmucosa, protruding through the circular muscle at the pointswhere the blood vessels penetrate the colonic wall. They tend tooccur in rows between the strips of longitudinal muscle, sometimespartly covered by appendices epiploicae. The rectum withits complete muscle layers is not affected. It is thought to berelated to reduced fibre in the western diet. This results in lowstool bulk with resulting segmentation and hypertrophy of thecolonic wall musculature, thus causing increased intraluminalpressure. Diverticular disease is rare in Africans and Asians, whoeat a diet that is rich in natural fibre.
DiverticulosisIt is important to distinguish between diverticulosis, which maybe asymptomatic, and clinical diverticular disease in which thediverticula are causing symptoms. On histological investigation,the diverticulum consists of a protrusion of mucous membranescovered with peritoneum. There is thickening of the circularmuscle fibres of the intestine, which develops saw-tooth appearance on barium enema
DiverticulitisDiverticulitis is the result of inflammation of one or more diverticula,usually with some pericolitis. It is not a premalignant condition, but cancer may coexist
The complications of diverticular disease are the following:1 Recurrent periodic inflammation and pain .2 Perforation leading to general peritonitis or local (pericolic)abscess formation.3 Intestinal obstruction:a in the sigmoid as a result of progressive fibrosis causingstenosis;b in the small intestine caused by adherent loops of smallintestine on the pericolitis.4 Haemorrhage: diverticulitis may present with profuse colonichaemorrhage in 17% of cases, often requiring blood transfusions.5 Fistula formation (vesicocolic, vaginocolic, enterocolic, colocutaneous)occurs in 5% of cases, with vesicocolic being the most common.
Clinical featuresElectiveIn mild cases, symptoms such as distension, flatulence and a sensationof heaviness in the lower abdomen may be indistinguishablefrom those of irritable bowel syndrome.EmergencyPersistent lower abdominal pain, usually in the left iliac fossa,with or without peritonitis, could be caused by diverticulitis.Fever, malaise and leucocytosis can differentiate diverticulitisfrom painful diverticulosis. The patient may pass loose stools ormay be constipated; the lower abdomen is tender, especially onthe left, but occasionally also in the right iliac fossa if the sigmoidloop lies across the midline. The sigmoid colon is often palpable,tender and thickened. Rectal examination may, but does not usually,reveal a tender mass. Any urinary symptoms may herald theformation of a vesicocolic fistula, which leads to pneumaturia(flatus in the urine) and even faeces in the urine.
1 Pericolic abscess or phlegmon 2 Pelvic or intra-abdominal abscess 3 Non-faeculent peritonitis 4 Faeculent peritonitis
Classification of diverticulitis (Hinchey)
DiagnosisRadiologyAlthough the diagnosis of acute diverticulitis is made on clinicalgrounds, it can be confirmed during the acute phase by computerised tomography (CT). It is particularly good at identifyingbowel wall thickening, abscess formation and extraluminal disease., drainage may be carried out percutaneously. Such anoption may delay or postpone further operative procedures.
Barium enemas and sigmoidoscopy are usuallyreserved for patients who have recovered from an attack of acute diverticulitis, for fear of causing perforation or peritonitis. Watersoluble contrast enemas may, however, be helpful in sorting out patients with large bowel obstruction. In the acute situation, it is good at detecting intraluminal changes and leakage. The sensitivity for this is of the order of 90%. Barium radiology is carried out to exclude a carcinoma and to assess the extent of the disease.
Where the sigmoid colon is thickened and narrowed, a ‘sawtooth’ appearance may be seen. Some strictures can be very difficult to distinguish by radiology alone and, in those circumstances, colonoscopy will be necessary to rule out a carcinoma. Vesicocolic fistulae should be evaluated with cystoscopy and biopsy in addition to colonoscopy. Contrast examinations may show the fistula itself. The differential diagnosis for vesicocolic fistulae (and other fistulae) includes cancer, radiation damage, Crohn’s disease (CD), tuberculosis and actinomycosis.
ColonoscopyColonoscopy may reveal the necks of diverticula within the bowel lumen . The differential diagnosis from a carcinoma can beimpossible if a tight stenosis prevents colonoscopy. In equivocalcases, biopsies may be taken
ManagementNon-complicatedDiverticulosis should be treated with a high-residue diet containing bread, flour, fruit and vegetables. Bulkformers such as bran, Isogel and Fybogel may be given
until the stools are soft. Painful diverticular disease may requireantispasmodics.Acute diverticulitis is treated by bed rest and intravenousantibiotics (usually cefuroxime and metronidazole).
Operative procedures for diverticular diseaseThe aim of surgery is to control sepsis in the peritoneum and circulation.Indications for operation include general peritonitis andfailure to resolve on conservative treatment. Postoperative mortality and reoperation rate for elective resection are 5% and 12%, respectively
The ideal operation carried out as after careful preparation of the gut is a one-stage resection. This involves removal of the affected segment and restoration of continuity by end-to-end anastomosis
If there is obstruction, inflammatory oedema and adhesions orthe bowel is loaded with faeces, a Hartmann’s operation is theprocedure of choice
In acute perforation, peritonitis soon becomes general andmay be purulent, with a mortality rate of about 15%. Grossfaecal peritonitis carries a mortality rate of more than 50% andpneumoperitoneum is usually present; the diagnosis may notbe confirmed until emergency laparotomy. There is a choice ofprocedures:a primary resection and Hartmann’s procedure ;b primary resection and anastomosis after on-table lavage inselected cases;c exteriorisation of the affected bowel, which is then openedas a colostomy, a procedure now rarely used. Fistulae can be cured only by resection of the diseased boweland closure of the fistula. In the case of a colovesical fistula
Haemorrhage from diverticulitis must be distinguished fromangiodysplasia. It usually responds to conservative managementand occasionally requires resection On-table lavage andcolonoscopy may be necessary to localise the bleeding site. Ifthe source cannot be located, then subtotal colectomy andileostomy is the safest option..
Solitary diverticulum of the caecum and ascending colon is rareand congenital, and may present with symptoms and signs identical to those of acute appendicitis
Hirschsprung’s diseaseHirschsprung’s disease is characterised by the congenital absence of intramural ganglion cells and the presence of hypertrophicnerves in the distal large bowel. The affected gut is tonically contracted causing functional bowel obstruction. The aganglionosis is restricted to the rectum and sigmoid colon in 75% of patients (short segment), involves the proximal colon in 15% (long segment) and affects the entire colon