Major manifestations of hepatobiliary diseases.
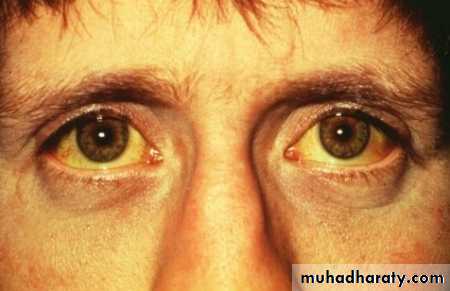
JaundiceJaundice, or icterus, is a yellowish discoloration of tissue(skin and m.m) resulting from the deposition of bilirubin due to hyperbilirubinemia. Total serum bilirubin is normally 0.2–1.2 mg/dL .and jaundice may not be recognizable until levels are about 3 mg/dL.
Subclinical hyperbilirubinemia when serum bilirubin increased more than normal (between 1.2 -3mg/dl) with undetected jaundice clinically .
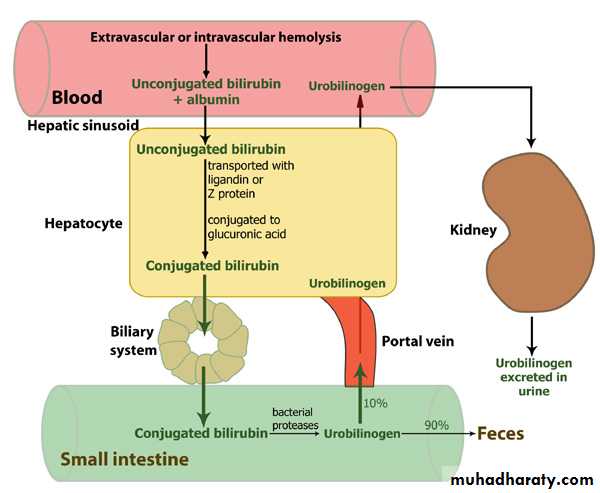
Production and Metabolism of Bilirubin
Bilirubin is the end product of haem degradation. Some 70–90% of bilirubin is derived from degradation of the hemoglobin of senescent red blood cells and the reminder from hemeprotein such as mygloblin and cytochromes enzyme .Unconjegated bilirubin is water-insoluble ,it is bound to albumin and does not pass into urine .it is transported to the liver by carrier mediated kinetic .within the hepatocyte .bilirubin is conjugated with one or two glucuronic acid by specific glucuronyl transferase to form bilirubin mono- and di- glucuronid, respectively, these conjugated bilirubin are water-soluble and exported into the bile by specific carrier on the hepatocyte membrane.
Conjugated bilirubin is metabolized by colonic bacteria to form stercobilinogen, which may be further oxidized to stercobilin. Both stercobilinogen and stercobilin are excreted in the stool.
A small amount of stercobilinogen ((4 mg/dl))is absorbed from the bowl passes through the liver and is in excreted the urine .where it is known as urobilinogen or following further oxidization to urobilin.
Production and Metabolism of Bilirubin
History
-duration of jaundice.-use or exposure to medication-OTC, physicion prescribed.
-complementary or alternative medicine-herbal or vitamin preparation or steroid.
-parenteral exposures-transfusion, iv abuse.
-tattoos, sexual activity and alcohol history.
-Loss of weight or appetitte.
-bleeding diathesis.
-Recent travel exposure.
-exposure to patients with jaundice.
-Occupational history-contact with rats.
-exposure to contaminated food or water.
-Family history of haemolytic anaemia ,congenital hyperbilirubinemia and hepatitis.
-Dyspepsia, fat intolerance or biliary colic.
-Accompanying symptoms-arthralgia, rash, anorexia, weight loss, abdominal pain-choledocholithiasis and ascending cholangitis.
-Fever .
-Pruritis.
-changes in colour of urine and stools.
Physical examination
-Assessment of nutritional status.-Temporal and proximal muscle wasting –cirrhosis.
-Scratch marks, purpura, fetor hepaticas.
-stigmata of chronic liver disease-spider nevi.
-Palmar erythema.
-gynecomastia.
-Caput medusa.
-Duputrens contracture,
-Parroted enlargement , testicular atrophy –advance alcoholic cirrhosis.
Enlarged left supraclavicular lymph nodes.
-Periumbilical nodule-sister marry josephs.-J VP-right heart failure.
-Right side pleural effusion.
-Leg oedema , nails- clubbing and white nails.
-Tremors or flap, KF ring.
-Abdominal examination
Size and consistency of liver and spleen.
-nodular liver – malignancy.
-Tender liver –alcoholic, viral, parasitic, amyloid, hepatic congestion.
Murphy sign- cholecystitis.
Palpable Gallbladder and Courvoisier sign.
-Ascites and jaundice –cirrhosis or malignancy with peritoneal spread.
-Abdominal veins
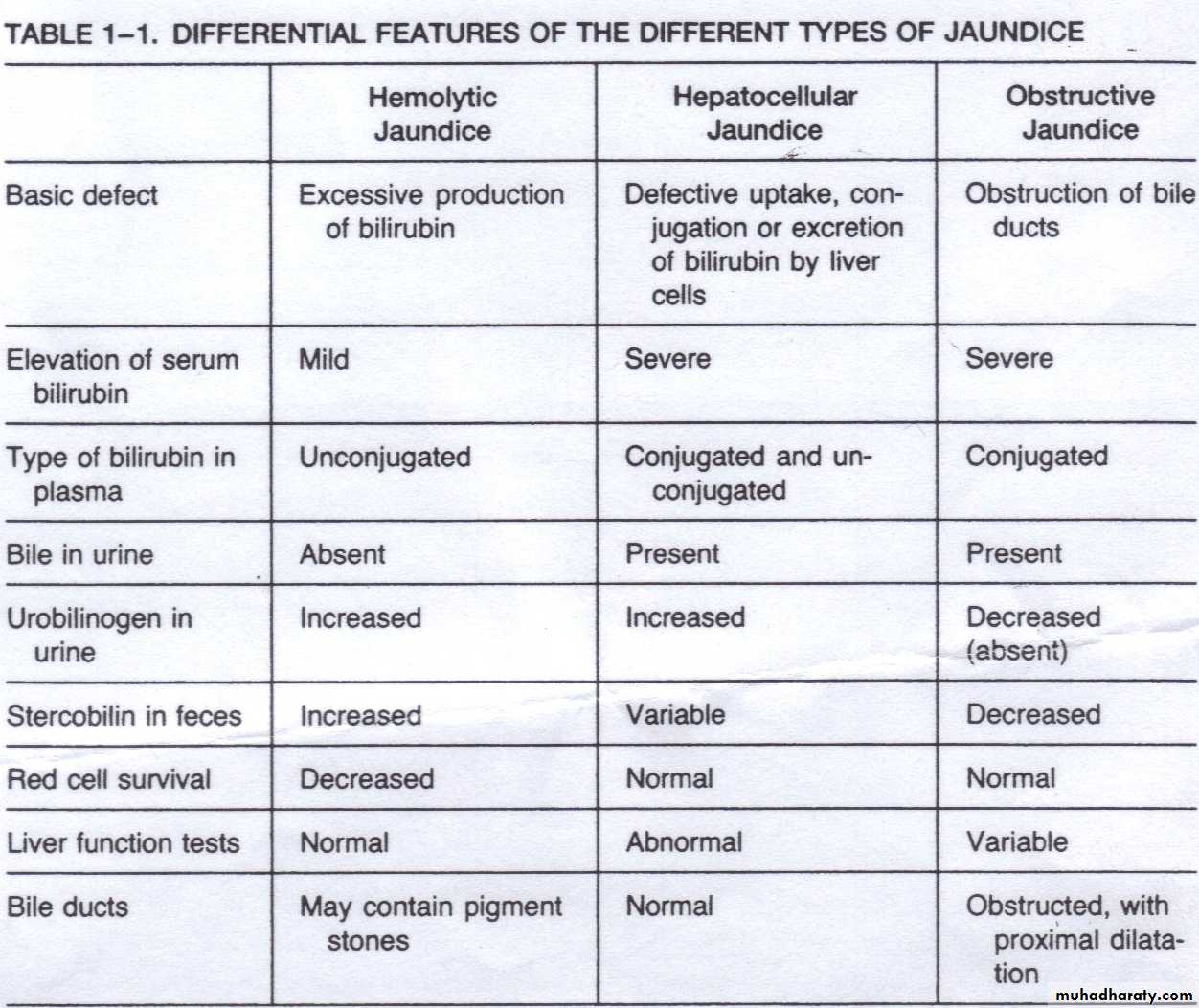
Mechanisms producing jaundice (types of jaundice)
Jaundice divided into three categories based on where they start before, in, or after the liver:-
1)-pre-hepatic.
2)-hepatic .
3)-post-hepatic.
1)-pre-hepatic or heamolytic jaundice (increased production of bilirubin)
Causes
1 jaundice caused by anything which causes an increased rate of hemolysis (breakdown of RBC).
2)- In tropical countries, malaria can cause jaundice in this manner.
3)- Certain genetic diseases(sickle cell anemia, thalassemia , and glucose 6-phosphate dehydrogenase deficiency) can lead to increased red cell lysis and therefore hemolytic jaundice.
4)-ineffective erythropoiesis.
Clinical features
1)-there are often no stigmata of chronic liver diseases other than jaundice.2)-normal coloured or dark stool due to stercobilinogen.
3)-dark coloured urine on standing due to urobilinogen.
4)signs and symptoms of hemolytic disorders e.g. pallor and splenomegaly due to hemolytic anemia.
Investigation
1)increased unconjugated bilirubin usually less than 6 mg/dl.
2)-normal liver function test.
3)-C.B.P. reviled evidence of hemolytic anemia.
2)- Hepatocellular jaundice( due to regurgitation of unconjugated and conjugated bilirubin from damage hepatocytes or bile ducts.
Causes
1)- acute parenchymal liver diseases .
e.g. viral hepatitis , alcoholic hepatitis, drugs induce hepatitis ,Wilson disease and autoimmune hepatitis.
2)-chronic parenchymal liver diseases .
e.g. chronic viral hepatitis, alcoholic hepatitis, and autoimmune hepatitis.
Clinical features
The clinical features of hepatocellular jaundice depend on the underlying diseases ,usually the patient have general feature of hepatitis like nausea ,vomiting ,abdominal pain ,arthralgia and dark colour of both stool and urine.Investigation
1)-increased both conjugated and unconjugated bilirubin.
2)-increased ALT/AST enzymes out of proportion to Alk. Phosphatise enzyme.
3)-Post-Hepatic or Cholestatic jaundice (impaired excretion of bilirubin)
causesThe pathology is located after the conjugation of bilirubin in the liver
obstructive jaundice, is caused by an interruption to the drainage of bile in the biliary system( either intrahepatic or extrahepatic causes) .
1)-intrahepatic causes
-primary biliary cirrhosis.-primary sclerosing cholengitis
-alcoholic liver diseases.
-drugs e.g. oral C.C.P .anabolic steroid.
- cholestasis of viral hepatitis.
-pregnancy induce cholestasis.
-post-op. Cholestasis.
2)- extrahepatic causes
-Gall-bladder diseases and C.B.D stones
-CA of pancrease , ampullary tumor -traumatic biliary obstruction.
Clinical features
The clinical features of cholestatic jaundice include these due to cholestasis itself and these due to the cholengitis1)features of cholestasis..
Early features
-jaundice is yellow-greenish colour due to deposition of Bilirubin mostly conjugated
-dark urine due to hyperbilirubinemia.
-pale stool due to loss of stercobilinogen.
-pruritis due to deposition of bile salt in skin
Late features
-xanthelasma and xanthomata due to hypercholesterolemia.
-maabsorption features e.g. weight loss, steatoria,Osteomalacia due to diffencincy Lipid-soluble vitamins ((D,E,A,K)).
.
2)-features of cholengitis .
-fever.-abdominal pain.
-rigor.
-hepatic absences.
Investigations
1)-increased conjugated fraction of bilirubin.
2)-increased Alk. Phosphatise and GGT enzymes compared with ALT and AST enzymes.
3)-U/S reviled intra- and/or extrahepatic duct dilation and found the cause of biliary obstruction.
Isolated hyperbilirubinemia.
When there is increase serum bilirubin (conjugated or unconjugated )) with normal liver enzymes .Causes
1)- unconjugated -inherited diseases A)-Gilbart,s syndrome
B)-Criglar-Najar syndrome .
-heamolytic disorders.
-drugs e.g. rifampecin .
2)- conjugated -Dobin –johnson syndrome.
-Rotor,s disease.