MINIMAL CHANGE NEPHROTIC SYNDROME
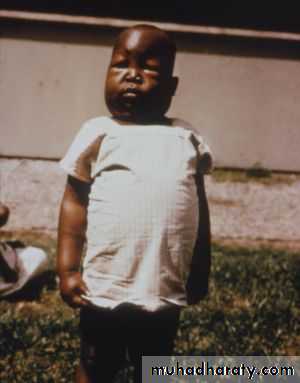
(MCNS)• It is idiopathic NS, more common in boys than in girls (2 : 1)
• Most commonly appears between the ages of 2 and 6 yr, but, it has been reported as early as 6 mo of age and throughout adulthood.• MCNS is present in 85-90% of patients <6 yr of age and only in 20-30% of adolescents.
Clinical features of MCNS:
• The initial episode and subsequent relapses, usually follows minor infections (commonly URTI) and, uncommonly, reactions to insect bites and beestings.• With time, the edema becomes generalized, causing ascites, pleural effusions, and genital edema.
• mild edema, which is initially periorbital and in the lower extremities decreases throughout the day.
اني عندي
Nephroticو خلي واحد بيكم ما
يفهمني زين.....اريد اشوف شلون ينجح؟؟
• Anorexia, irritability, abdominal pain, and diarrhea are common.
• Absence of hypertension and gross hematuria (the so-called nephritic features).Clinical features of MCNS:
• Acute or chronic renal insufficiency
A diagnosis other than MCNS should be considered in:• Children <1 yr or > 12 yr of age, with a positive family history of nephrotic syndrome
• And/or the presence of:
• Extrarenal findings (arthritis, rash, anemia)
• Hypertension or pulmonary edema
• Gross hematuria.
• Acute or chronic glomerulonephritis
Differential diagnosis of marked edema:
• Protein-losing enteropathy
• Hepatic failure
• Heart failure
• Protein malnutrition.
Investigations:
• Urinalysis: 3+ or 4+ proteinuriaMicroscopic hematuria in 20%.
• Spot urine protein : creatinine ratio>2.0.
• Normal Serum creatinine and BUN
• S. albumin <2.5 g/dL (Hypoalbuminemia)
• Increased S. cholesterol and triglyceride
• Normal S. complement levels (C3).
• Steroid resistance, steroid dependent or frequent relapsing NS.
• Renal biopsy indicated in:• Age <1 yr or >12 yr
• Gross hematuria
• Hypertension
• Renal insufficiency
• Hypocomplementemia (low C3 levels)
• Positive family history of NS
• Extrarenal findings (e.g. arthritis, rash, anemia)
• Tuberculosis must be excluded before C.s. therapy by a purified protein derivative (PPD) skin test.
Treatment MCNS:
A. General considerations:
• First episode with mild-moderate edema could be manage as outpatient at home.
• Child’s parents should learn about the signs and symptoms of the disease and its complications, how use the dipstick and interpretations the results for proteinuria.
• Started without need of renal biopsy in children with uncomplicated NS between 1 and 8 yr of age.
B. Corticosteroid (CS) therapy:
• Is the mainstay of MCNS therapy
• Approximately 80-90% of children respond to steroid therapy.
• Regimen:
• Prednisolone as single daily dose of 60 mg/m2/day or 2 mg/kg/day to a maximum of 60 mg daily for 4-6 wk• followed by alternate-day prednisone (starting at 40 mg/m2/d or 1.5 mg/kg/d) for a period ranging from 8 wk to 5 mo, with tapering of the dose.
B. Corticosteroid (CS) therapy:
• Remission consists of a urine protein : creatinine ratio of <0.2 or <1+ protein on urine dipstick for 3 consecutive days.
• Response is defined as the achievement of remission within the initial 4 wk of corticosteroid therapy.
• The vast majority of children who respond to prednisone therapy achieve remission within the first 5 wk of treatment.
B. Corticosteroid (CS) therapy:
C. Treatment of Edema:
• Children with severe symptomatic edema, including large pleural effusions, ascites, or severe genital edema, should be admitted to the hospital.
• A swollen scrotum may be elevated with pillows to enhance fluid removal by gravity.
• Sodium restriction (<1500 mg daily) and water/fluid restriction may be necessary.
• Loop diuretics (furosemide), 1-2 mg/kg/dose orally or intravenously, should be used with extreme caution because aggressive diuresis can lead to I.V volume depletion and an increased risk for acute renal failure and I.V thrombosis.
C. Treatment of Edema:
• Complications of IV albumin therapy: Symptomatic volume overload, hypertension, heart failure, and pulmonary edema.
• 25% albumin (0.5-1.0 g albumin/kg) as a slow infusion followed by furosemide (1-2 mg/kg/ dose IV) is indicated in severe generalized edema with evidence of I.V volume depletion (e.g. HT, tachycardia hemoconcentration).
C. Treatment of Edema:
• Defined as a urine protein : creatinine ratio of >2 or ≥3+ protein on urine dipstick testing for 3 consecutive days.
Relapse of nephrotic syndrome:
• Relapses are common, especially in younger children, and are often triggered by upper respiratory or gastrointestinal infections.
Treatment of Relapse:
• Daily high-dose prednisone is given until the child has achieved remission (urine protein : creatinine ratio of <0.2 or <1+ protein on urine dipstick for 3 consecutive days), and the regimen is then change to alternate-day therapy.• Similarly to the initial episode, except that daily prednisone courses are shortened.
اكعدووووووووا
• Steroid-resistant NS require further evaluation, including a diagnostic kidney biopsy, evaluation of kidney function, and quantitation of urine protein excretion (in addition to urine dipstick testing).• Defined as the failure to achieve remission after 8 wk of CS therapy.
• It usually caused by FSGS (80%), MCNS, or membranoproliferative GN.
Steroid Resistance NS:
It mean that the patient who responded to daily CS therapy have relapse shortly after switching to or after terminating the alternate-day therapy.
Steroid dependent NS:
Alternative Therapies to CS in the Treatment of NS:
1. Cyclophosphamide:• It prolongs the duration of remission and reduces the number of relapses.
• Indication:
• steroid-dependent NS
• Frequent relapses
• steroid-resistant NS
• Severe CS toxicity
• Increased risk of future malignancy
1. Cyclophosphamide:
• Side effects:
• Neutropenia
• Disseminated varicella
• Hemorrhagic cystitis
• Alopecia
• Sterility
1. Cyclophosphamide:
• WBC count must be monitored weekly and the drug should be stopped if the count < 5,000/mm3• Dose:
• 2 mg/kg as single oral dose for 8-12 wk
• Alternate-day prednisone therapy is continued during the course of cyclophosphamide therapy.
2. Calcineurin inhibitors (cyclosporine)
• Recommended as initial therapy for children with steroid-resistant NS.• Side effects:
• Hypertension
• Nephrotoxicity
• Hirsutism
• Gingival hyperplasia
• Maintain remission in steroid-dependent or frequently relapsing NS
3. Mycophenolate
• An antihelmintic agent with immunomodulating effects that reduce the risk of relapse in comparison to prednisone
4. Levamisole
5. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers:
• Use as adjunct therapy to reduce proteinuria in steroid-resistant patients.Immunizations of nephrotic children:
• Give full pneumococcal and influenza vaccination annually to the child and their household contacts• Live vaccines should postponed until the prednisone dose is below either 1 mg/kg daily or 2 mg/kg on alternate days.
• Live virus vaccines are contraindicated in children receiving CS sparing agents e.g. cyclophosphamide or cyclosporine.
• Following close contact with varicella infection, patients on immunosuppressive agents should receive VZIG and immunize healthy household contacts with live vaccines to minimize the risk of transfer of infection to the immunosuppressed child, but avoid direct exposure of the child to GIT or respiratory secretions of vaccinated contacts for 3-6 wk after vaccination.
Complications of NS:
• Infection is a major complication of NS.• The common infection is Spontaneous bacterial peritonitis, although sepsis, pneumonia, cellulitis, and UTI may be seen.
• The empirical antibiotic should cover Pneumococcus and Gram-negative bacteria. A 3rd-generation cephalosporin is a common choice of IV antibiotic.
• In the case of spontaneous bacterial peritonitis, peritoneal fluid should be collected and sent for cell count, Gram stain, and culture.
• If infection is suspected, a blood culture should be done prior to starting empiric antibiotic therapy.
• Management:
• To minimize the risk of thromboembolic complications, aggressive use of diuretics and the use of indwelling catheters should be avoided if possible.
Complications of NS:
• Increased risk of thromboembolic events (Both arterial and venous thrombosis)
• Anticoagulation therapy is effective including heparin and warfarin
Complications of NS:
• Cardiovascular disease:• It is due to hyperlipidemia, particularly in patients with complicated NS
• is a rare complication in children. e.g. myocardial infarction
Prognosis of NS:
• Most children with steroid-responsive NS have repeated relapses, which generally decrease in frequency with child age.• Children who respond rapidly to steroids and those who have no relapses during the first 6 mo after diagnosis are likely to follow an infrequently relapsing course.
Prognosis of NS:
• It is important to explain to the family that the child with steroid-responsive NS is unlikely to develop chronic kidney disease, that the disease is rarely hereditary, and that the child (in the absence of prolonged cyclophosphamide therapy) will remain fertile.Prognosis of NS:
• Children with idiopathic NS should not be considered chronically ill and should participate in all age-appropriate childhood activities and maintain an unrestricted diet when in remission.• Children with steroid-resistant NS, most often caused by FSGS, have poorer prognosis.
Prognosis of NS:These children develop progressive renal insufficiency, ultimately leading to end stage renal disease requiring dialysis or kidney transplantation
Recurrent nephrotic syndrome develops in 30-50% of transplant recipients with FSGS.
Thank you for your attention