THYROID GLAND DISORDER L2
Etiological classification of congenital hypothyroidism:Primary hypothyroidism :
Defect of fetal thyroid development (dysgenesis )
Defect in thyroid hormones synthesis
Defect in thyroid hormones transport
Resistance to thyroid hormones
Maternal antibodies
Iodine deficiency
Maternal medication (iodides .amiodarone . methimazole ,radioiodide )
Central hypo pituitary hypothyroidism
TSH deficiency
Isolated TRH deficiency
Multiple congenital pituitary hormones deficiencies
Clinical features of congenital hypothyroidism
Most cases of congenital hypothyroidism are asymptomatic because partial trans placental passage of maternal T4.
S of cong.hypothyroidsm &s
Normal weight & length at birth
Slight enlargement of head because myxedema
Wide anterior &posterior fontanel
Prolonged physiological jaundice (early sign)
Feeding difficulties& choking &delayed teeth eruption
Cry little &sleep much poor appetite
Constipation not respond to treatment with umbilical hernia
Genital edema ,slow pulse ,cardiac murmur with macrocytic anemia
Broad hands &short fingers
Dry scaly skin &little perspiration
Developmental delay ,hoarse voice &they don’t learn to talk
Physical &intellectual impairment increase with age with delayed sexual maturation
Laboratory finding:
Heal prick between 2-5 days of age ( filter paper ).
Serum level of T4 & free T4 usually low …..T3 may be normal & usually not helpful in diagnosis. ECG show slow voltage ,echo may show pericardial effusion.
Radiological finding :
retarded osseous maturation at birth in 60 % of cases .
Distal femoral &proximal tibial epiphyses normally present at birth are often absent.
Deformity( beaking )of the 12th thoracic or 1st or 2nd lumber vertebra is common , skull show wide sutures ,enlarge and round sella turcica
Treatment :
1)Levothyroxine (L-T4)given orally at morning.
2)Recommended initial starting dose is 10-20 µg/kg/day [ serum T4 &freeT4 ,TSH ]should be checked every 1-2 mo.in 1st 6 mo. Of life .then every 2-4 mo.
From 6mo. -3 yrs. Of age
3)T4 . Take a week to be normal & TSH need 3-6 mo.to come back to normal
Prognosis :
Early diagnosis and adequate treatment from 1st wk.of life result in normal linear growth &development . variable degree of brain damage may contribute to [delay diagnosis, inadequate treatment &poor compliance in first 2-3 years of life )
Follow up
TSH. Monthly in 1st 6 months then every 2-3 month between 6m-2 yrs . Of age
Follow up include :
1- growth
2- development
3-radiological assessment
4-lab.assessment
5-psychometric assessment
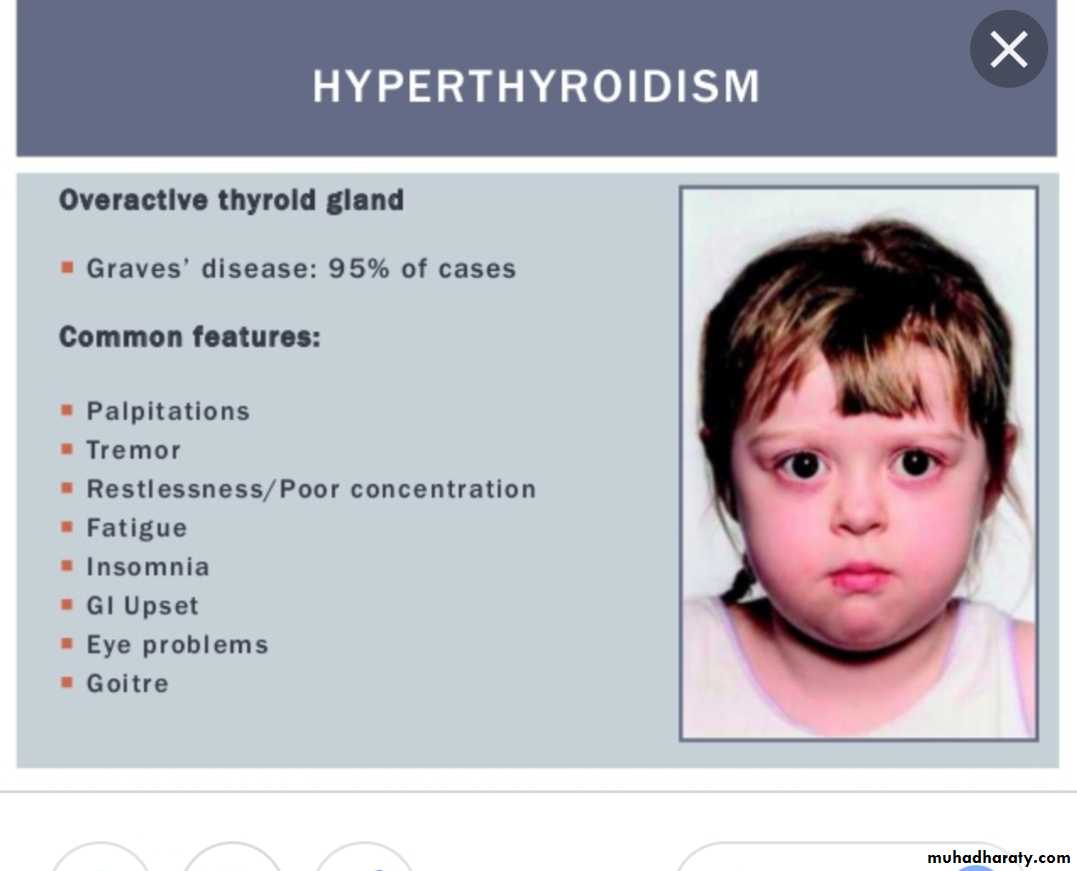
HYPERTHYROIDISM : Excessive secretion of thyroid hormones it is caused by Graves disease
Clinical features of hyperthyroidism :
Symptoms :
Hyperactivity .irritability ,altered mood, insomnia poor concentration
Heat intolerance
Fatigue ,weakness ,palpitation
Dyspnea ,weight loss ,thirst &polyuria with loose stool
Signs :
Sinus tachycardiaFine tremor , hyperreflexia moist &worm skin
Palmer erythema ,
Hair loss or thinning
Chorea
Osteoporosis ,hypokalemic periodic paralysis
Psychosis
LAB. Finding :
High T3--T4 &free T4and low TSH and T3 usually elevated more than T4
Treatment :
Medical treatment is recommended rather than radioiodine or surgery (1)Propylthiouracil(PTU) &methimazole[Tapazole ]( potent 10 time than PTU)
(2)Initial dose of Methimazole :0.25mg-1mg /kg /24hr once or twice daily
(3)Clinical response appear after 3-6 wks and adequate control evident in3-4 months
(4) Beta blocker like propranolol in dose 0.5-2 mg/kg/day orally useful in toxic patients
Disorder of parathyroid gland:
Parathyroid hormones: PTH also called parathemone secreted by parathyroid gland which is important in bone remodeling .PTH secreted in response to low blood serum calcium level .calcitonin : also called thyrocalcitonin it is hormone produced primarily by Para follicular cell in thyroid gland and act to reduce level of calcium and opposing the effect of PTH hormone .
HYPORARATHYROIDISM :Etiology: A: congenital
Transient neonatal
Familial isolated hypopara .(AR,AD.Xlinked )
Di George syndrome & sanjad –sakati syndrome (short stature, retardation .dysmorphism )
Barakat syndrome (sensorineural hearing loss with renal dysplasia )
B :acquired (autoimmune ,infiltrative ,maternal hyperparathyroidism ,hypomagnesemia)
Clinical features:
Vary from asymptomatic to sever form of hypocalcemia
Muscular pain &cramps are early signs
Numbness stiffness &tingling of hands and feet
Chevostek or trousseau sign or carpopedal spasm may be only signs
Convulsion with or without loss of consciousness (mistaken as epilepsy )
Headache & vomiting because raised ICP
Delayed teeth eruption &dry scaly skin
Mucocutaneous candidiasis
Cataract .addison disease pernicius anemia ,alopecia
Lab. Finding :
serum calcium is low
5-7mg/dl
phosphorus level is elevated
(7-12mg/dl)
Ionized Ca which reflect 45% of the total
Low
Alkaline phosphatase
normal or
low
1,25(OH)2D3
Usually low& high in sever hypocalcemia
Magnesium
Normal
PTH
Low
Treatment :
Emergency treatment of neonatal tetany consist of injection of 5-10 ml or 1-3 mg/kg of 10%solution calcium gluconate (elemental 9.3 mg/ml )
D3 (active form calcitriole ): also should be given (initial dose 0.25µg/24 hr .with maintenance dose 0.01-0.1 µg/kg/24hr
Supplemental calcium in form of calcium gluconate provide 800 mg elemental calcium daily or ca++ carbonate
PSUODOHYPOPARATHYROIDSM( PHP)
(1){Albright hereditary osteodystrophy )(2)Parathyroid hormone here are normal and serum level of PTH are elevated even when patient is hypocalcemic(peripheral resistance to PTH rather than deficiency ) .we have type 1A (common ) &type 1B less common & type 2.(tissue specific resistant to PTH)
Hypocalcemia ,high PTH, hyperphosphotemia =psudohypoparathyroidism (PSHPT)
Type 1A : account for majority of cases
Tetany is often presenting sign
Short stocky build &round face
Brachydactyly with dimpling dorsum of the hand
2nd metacarpal bone involve result in index finger longer than middle
Short and wide phalanges .bowing ,exostoses &thickening of calvaria
Moderate degree of cognitive impairment
Calcification of basal ganglia with lenticular cataract
Pseudopseudohypoparathyroidism PPHP(Albright hereditary osteodystrophy AHO )
Inherited disorder ,it is similar to pseudohypoparathyroidism (PHP) in presentation
serum level of calcium and phosphorus usually normal with PTH hormone slightly elevated & no resistant to PTH
Clinical features :
short stature . Round face .brachydactyly.ectopic ossification of soft tissue. Shortining of 4th metacarbal bone
DX: exclusion of other causes of HPT, and genetic study GNAS mutation
Condition
AppearancePTH
Calcium
Phosphates
Hypoparathyroidism
Normal
Low
Low
High
Pseudohypoparathyroidism type 1A
Skeletal defect
High
Low
High
Pseudohypoparathyroidism type 1B
Normal
High
Low
High
Pseudohypoparathyroidism type 2
Normal
High
Low
High
Pseudopseudohypoparathyroidism
Skeletal defect
Normal
Normal
Normal
Regarding thyroid ¶thyroid disorder
Thyroxin hormone given at meal time twice daily in hypothyroidism
Phosphorus is low in pseudopseudohypopara
PTU is more potent than methimazole
Normal T3 level in cong . Hypothyroidism
D3 should be given in hypoparathyroidism