CROHN’S DISEASE (REGIONAL ENTERITIS) It can affect any part of the gastrointestinal tract from the lips to the anal margin, but ileocolonic disease is the most common presentation.
EpidemiologyIt is most common in North America and northern Europe withan incidence of 5 per 100 000. It is slightly more common in women than in men, but is most commonly diagnosed in young patients between the ages of 25 and 40 years.
AetiologyAlthough CD has some features suggesting chronic infection, nocausative organism has ever been found; similarities between CDand tuberculosis have focused attention on mycobacteria. Studieshave found DNA of Mycobacterium paratuberculosis in the intestinesof 60% of patients with CD . However, no immunology reaction has been detected against this organism, and anti-tuberculosis treatment has no effect. Focal ischaemia has also been postulated as a causative factor, possibly originating from a vasculitis arising through an immunological process. Smoking increases the risk.
Genetic factors are thought to play a part. About 10% ofpatients have a first-degree relative with the disease. There is an association with ankylosing spondylitis. As withUC, it is now believed that CD can predispose to cancer .
PathogenesisAs in UC, there is thought to be an increased permeability of themucous membrane. This leads to increased passage of antigens,which are thought to induce a cell-mediated inflammatoryresponse. This results in the release of cytokines, such as interleukin- 2 and tumour necrosis factor, which coordinate local and systemic responses. In CD, there is thought to be a defect in suppressor T cells.
PathologyIleal disease is the most common, accounting for 60% of cases;30% of cases are limited to the large intestine, and the remainderare in patients with ileal disease alone or more proximal smallbowel involvement. Anal lesions are common. CD of the mouth,oesophagus, stomach and duodenum is uncommon.
Resection specimens show a fibrotic thickening of the intestinal wall with a narrow lumen. There is usually dilated gut just proximal to the stricture and, in the strictured area, there are deep mucosal ulcerations with linear or snake-like patterns. Oedema in the mucosa between the ulcers gives rise to a cobblestone appearance.
The transmural inflammation leads to adhesions,inflammatory masses with mesenteric abscesses and fistulae intoadjacent organs.
mesenteric lymph nodes are enlarged. The condition is discontinuous, with inflamed areas separated fromnormal intestine, so called skip lesions. There are non-caseating giant cell granulomas, but these are only found in 60% of patients.
Clinical featuresPresentation depends upon the area of involvement.Acute Crohn’s diseaseAcute CD occurs in only 5% of cases. Symptoms and signs resemblethose of acute appendicitis, but there is usually diarrhoea preceding the attack. Acute colitis with or without toxic megacolon can occur in CD but is less common than in UC.
Chronic Crohn’s diseaseThere is often a history of mild diarrhoea extending over manymonths, occurring in bouts accompanied by intestinal colic.Patients may complain of pain, particularly in the right iliac fossa,and a tender mass may be palpable. Intermittent fevers, secondaryanaemia and weight loss are common. A perianal abscess orfissure may be the first presenting feature of CD.After months of repeated attacks with acute inflammation,the affected area of intestine begins to narrow with fibrosis,causing obstructive symptoms.With progression of the disease, adhesions and transmural fissuring,intra-abdominal abscesses and fistula tracts can develop.1 Enteroenteric fistulae can occur into adjacent small bowel loopsor the pelvic colon, and enterovesical fistulae may causerepeated urinary tract infections and pneumaturia.2 Enterocutaneous fistulae rarely occur spontaneously andusually follow previous surgery.
InvestigationLaboratoryA full blood count needs to be performed to exclude anaemia.There is usually a fall in albumin, magnesium, zinc and selenium,especially in active disease. Protein levels that correspondto disease activity include C-reactive protein.
EndoscopySigmoidoscopic examination may be normal or show minimalinvolvement. However, ulceration in the anal canal will bereadily seen. As a result of the discontinuous nature of CD, there will beareas of normal colon or rectum. In between these, there areareas of inflamed mucosa that are irregular and ulcerated, with amucopurulent exudate
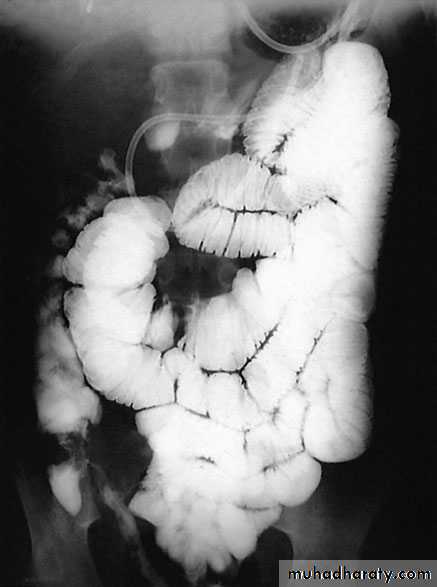
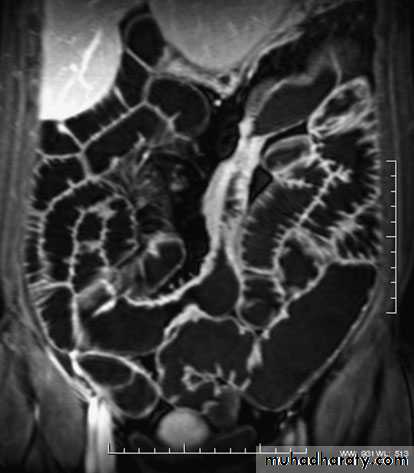
ImagingBarium enema will show similar features to those of colonoscopyin the colon. The best investigation of the small intestine is smallbowel enema . This will show up areas of delay anddilatation. The involved areas tend to be narrowed, irregular and,sometimes, when a length of terminal ileum is involved, theremay be the string sign of Kantor. Sinograms are useful in patientswith enterocutaneous fistulae. CT scans are used in patients withfistulae and those with intra-abdominal abscesses and complexinvolvement .Magnetic resonance imaging (MRI) has been shown to be usefulin assessing perianal disease.
TreatmentMedical therapySteroidsSteroids are the mainstay of treatment. These are effective ininducing remission in moderate to severe disease in 70–80% ofcases. Steroids can also be used as topical agents in the rectumwith reduced systemic bioavailability, but long-term use causesadrenal suppression. They are better at inducing remission thanmesalamine but has no role in maintenance. Patients suffering arelapse are treated with up to 40 mg of prednisolone orally daily,supplemented by 5-ASA compounds in those patients withcolonic involvement.
AntibioticsThose who have symptoms and signs of a mass or an abscessare also treated with antibiotics. Metronidazole is used,especially in perianal disease.Immunomodulatory agentsAzathioprine is used for its additive and steroid-sparing effectand is now standard maintenance therapy. It is a purine analogueCiclosporin acts by inhibiting cell-mediatedimmunity. Short-course intravenous treatment is associated with80% remission
Monoclonal antibodyInfliximab, the monoclonal antibody directedtowards tumour necrosis factor alpha, given to the patients withsevere, active disease who are refractory to ‘conventional’ treatments
Indications for surgerySurgical resection will not cure CD. Surgery is therefore focusedon the complications of the disease. These complications include:• recurrent intestinal obstruction;• bleeding;• perforation;• failure of medical therapy;• intestinal fistula;• fulminant colitis;• malignant change;• perianal disease.
SurgeryThe course of the disease after surgery is unpredictable, butrecurrence is common.1 Ileocaecal resection is the usual procedure for ileocaecal diseasewith a primary anastomosis between the ileum and theascending or transverse colon2 Segmental resection. Short segments of small or large bowelinvolvement can be treated by segmental resection3 Colectomy and ileorectal anastomosis4 Emergency colectomy5 Laparoscopic surgery.6 Temporary loop ileostomy.7 Proctocolectomy8 Strictureplasty9 Anal disease
Differences between UC and CD■ UC affects the colon; CD can affect any part of thegastrointestinal tract, but particularly the small and largebowel■ UC is a mucosal disease whereas CD affects the fullthickness of the bowel wall■ UC produces confluent disease in the colon and rectumwhereas CD is characterised by skip lesions■ CD more commonly causes stricturing and fistulation■ Granulomas may be found on histology in CD but not in UC■ CD is often associated with perianal disease whereas this isunusual in UC■ CD affecting the terminal ileum may produce symptomsmimicking appendicitis, but this does not occur in UC■ Resection of the colon and rectum cures the patient withUC, whereas recurrence is common after resection in CD
INFECTIONSIntestinal amoebiasisAmoebiasis is an infestation with Entamoeba histolytica. This parasitehas a worldwide distribution and is transmitted mainly incontaminated drinking water.PathologyThe ulcers, which have been described as ‘bottlenecked’ becauseof their considerably undermined edges, have a yellow necroticfloor, from which blood and pus exude. BiopsyEndoscopic biopsies or fresh hot stools are examined carefully tolook for the presence of amoebae.
Clinical featuresDysentery is the principal manifestation of the disease, but it maycome in various other presentations include =Appendicitis or amoebic caecal mass.. to operate on a patient with amoebic dysentery without precautions may prove fatal=Perforation.. the most common sites are the caecum and rectosigmoid.=Severe rectal haemorrhage as a result of separation of theslough is liable to occur.=Granuloma.. progressive amoebic invasion of the wall of the rectum or colon,with secondary inflammation, can produce a granulomatous massindistinguishable from a carcinoma.=Ulcerative colitis .. search for amoebae should always be made in the stools ofpatients believed to have UC.=Fibrous stricture may follow the healing of extensive amoebic ulcers.= Intestinal obstruction is a common complication of amoebiasis.= Paracolic abscess, ischiorectal abscess and fistula occur fromperforation by amoebae of the intestinal wall followed by secondaryinfection.
TreatmentMetronidazole (Flagyl) is the first-line drug, 800 mgthree times daily for 7–10 days. Diloxanide furoate is best forchronic infections associated with the passage of cysts in stools.Intestinal antibiotics improve the results of the chronic stages,probably by coping with superadded infection.
Typhoid and paratyphoidTyphoidParalytic ileus is the most common complication of typhoid.Intestinal haemorrhage may be the leading symptom. Othersurgical complications of typhoid and parathyroid include:• haemorrhage;• perforation;• cholecystitis;• phlebitis;• genitourinary inflammation;• arthritis;• osteomyelitis.Typhoid ulcerPerforation of a typhoid ulcer usually occurs during the thirdweek . The ulcer is parallel to the long axis of the gut and is usually situated in thelower ileum.Paratyphoid BPerforation of the large intestine sometimes occurs in paratyphoidB infection;
Tuberculosis of the intestineTuberculosis can affect any part of the gastrointestinal tract fromthe mouth to the anus. The sites affected most often are theileum, proximal colon and peritoneum. There are two principaltypes.Ulcerative tuberculosisUlcerative tuberculosis is secondary to pulmonary tuberculosisand arises as a result of swallowing tubercle bacilli. There aremultiple ulcers in the terminal ileum, lying transversely, and theoverlying serosa is thickened, reddened and covered in tubercles.Clinical featuresDiarrhoea and weight loss are the predominant symptoms, andthe patient will usually be receiving treatment for pulmonarytuberculosis.
RadiologyA barium meal and follow-through or small bowel enema willshow the absence of filling of the lower ileum, caecum and mostof the ascending colon as a result of narrowing.TreatmentA course of chemotherapy is given. Healing often occursprovided the pulmonary tuberculosis is adequately treated. Anoperation is only required in the rare event of a perforation orintestinal obstruction.
Hyperplastic tuberculosisThis usually occurs in the ileocaecal region, although solitary andmultiple lesions in the lower ileum are sometimes seen. This iscaused by the ingestion of Mycobacterium tuberculosis by patients.
Clinical featuresAttacks of abdominal pain with intermittent diarrhoea are theusual symptoms. The ileum above the partial obstruction is distended,and the stasis and consequent infection lead to steatorrhoea,anaemia and loss of weight. Sometimes, the presentingpicture is of a mass in the right iliac fossa in a patent with vagueill health. The differential diagnosis is that of an appendix mass,carcinoma of the caecum, CD, tuberculosis or actinomycosis ofthe caecum.
RadiologyA barium follow-through or small bowel enema will show a longnarrow filling defect in the terminal ileum.TreatmentWhen the diagnosis is certain and the patient has not yet developedobstructive symptoms, treatment with chemotherapy isadvised and may cure the condition. Where obstruction is present,operative treatment is required and ileocaecal resection is indicated .
Actinomycosis of the ileocaecal regionAbdominal actinomycosis is rare. Unlike intestinal tuberculosis,narrowing of the lumen of the intestine does not occur andmesenteric nodes do not become involved. However, a localabscess spreads to the retroperitoneal tissues and the adjacentabdominal wall, becoming the seat of multiple indurated discharging sinuses.
Clinical featuresThe usual history is that appendicectomy has been carried out foran appendicitis. Some 3 weeks after surgery, a mass is palpable inthe right iliac fossa and, soon afterwards, the wound begins to discharge.At first, the discharge is thin and watery, but later itbecomes thicker and malodorous. Pus should be sent for bacteriologicalexamination, which will reveal the characteristic sulphurgranules.TreatmentPenicillin or cotrimoxazole treatment should be prolonged and inhigh dosage.
TUMOURS OF THE SMALL INTESTINECompared with the large intestine, the small intestine is rarelyBenignAdenomas, submucous lipomas and gastrointestinal stromaltumours (GISTs) occur from time to time, and sometimes revealthemselves by causing an intussusception. The second most commoncomplication is intestinal bleeding from an adenoma, inwhich event the diagnosis is frequently long delayed because thetumour is overlooked at barium radiology, endoscopy and evensurgery.Peutz–Jeghers syndromeThis is an autosomal dominant disease. This consists of:• intestinal hamartomatosis is a polyposis affecting the whole ofthe small bowel and colon, where it is a cause of haemorrhageand often intussusception;• melanosis of the oral mucous membrane and the lips.
Long-term follow-up of patients with Peutz–Jeghers syndromehas shown reduced survival secondary to complications of recurrentbowel cancer and the development of a wide range of cancers.These include colorectal, gastric, breast, cervical, ovarian,
HistologyThe polyps can be likened to trees. The trunk and branches aresmooth muscle fibres and the foliage is virtually normal mucosa.TreatmentAs malignant change rarely occurs, resection is only necessary forserious bleeding or intussusception. Large single polyps can beremoved by enterotomy, or short lengths of heavily involvedintestine can be resected. The incidence of further lesions developing problems in the future can be reduced by thorough intraoperative examination at the time of the first laparotomy. Using on-table enteroscopy, polyps suitable for removal can be identified.Those lesions within reach can be snared by colonoscopy.
Malignant--LymphomaThere are three main types, as follows:1 Western-type lymphoma.They are now thought to benon-Hodgkin’s B-cell lymphoma in origin. They may presentwith obstruction and bleeding, perforation, anorexia andweight loss.2 Primary lymphoma associated with coeliac disease.this is now regarded as a T-cell lymphoma. Worsening ofthe patient’s diarrhoea, with pyrexia of unknown origintogether with local obstructive symptoms.3 Mediterranean lymphoma. This is found mostly in North Africaand the Middle East and is associated with α-chain disease.Unless there are particular surgical complications these conditionsare usually treated with chemotherapy.--CarcinomaLike small bowel tumours, these can present with obstruction,bleeding or diarrhoea. Complete resection offers the only hope of cure
Carcinoid tumourThese tumours occur throughout the gastrointestinal tract, mostcommonly in the appendix, ileum and rectum in decreasing orderof frequency. They arise from neuroendocrine cells at the base ofintestinal crypts. The primary is usually small but, when theymetastasise, the liver is usually involved; when this has occurred, the carcinoid syndrome will become evident.The tumours can produce a number of vasoactive peptides, mostcommonly 5-hydroxytryptamine (serotonin), which may be presentas 5-hydroxyindoleacetic acid (5-HIAA) in the urine duringattacks.
The clinical syndrome itself consists of reddish-blue cyanosis,flushing attacks, diarrhoea, borborygmi, asthmatic attacks and,eventually, sometimes pulmonary and tricuspid stenosis.Classically, the flushing attacks are induced by alcohol.
TreatmentMost patients with gastrointestinal carcinoids do not have carcinoid syndrome. Surgical resection is usually sufficient. In thecases found incidentally at appendicectomy, nothing further isrequired. In patients with metastatic disease, multiple enucleationsof hepatic metastases or even partial hepatectomy can becarried out. The treatment has been transformed by the use ofoctreotide (a somatostatin analogue)
Gastrointestinal stromal tumoursThese tumours can be either benign or malignant. Increasedsize is associated with malignant potential. GIST is a type ofsarcoma that develops from connective tissue cells. It is foundmost commonly in the stomach but can be found in other sitesof the gut. It occurs most commonly in the 50- to 70-year agegroup.
SymptomsPatients may be asymptomatic. Other symptoms include lethargy,pain, nausea, haematemesis or melaena.Treatment Surgery is the most effective way of removing GISTs as they are radioresistant
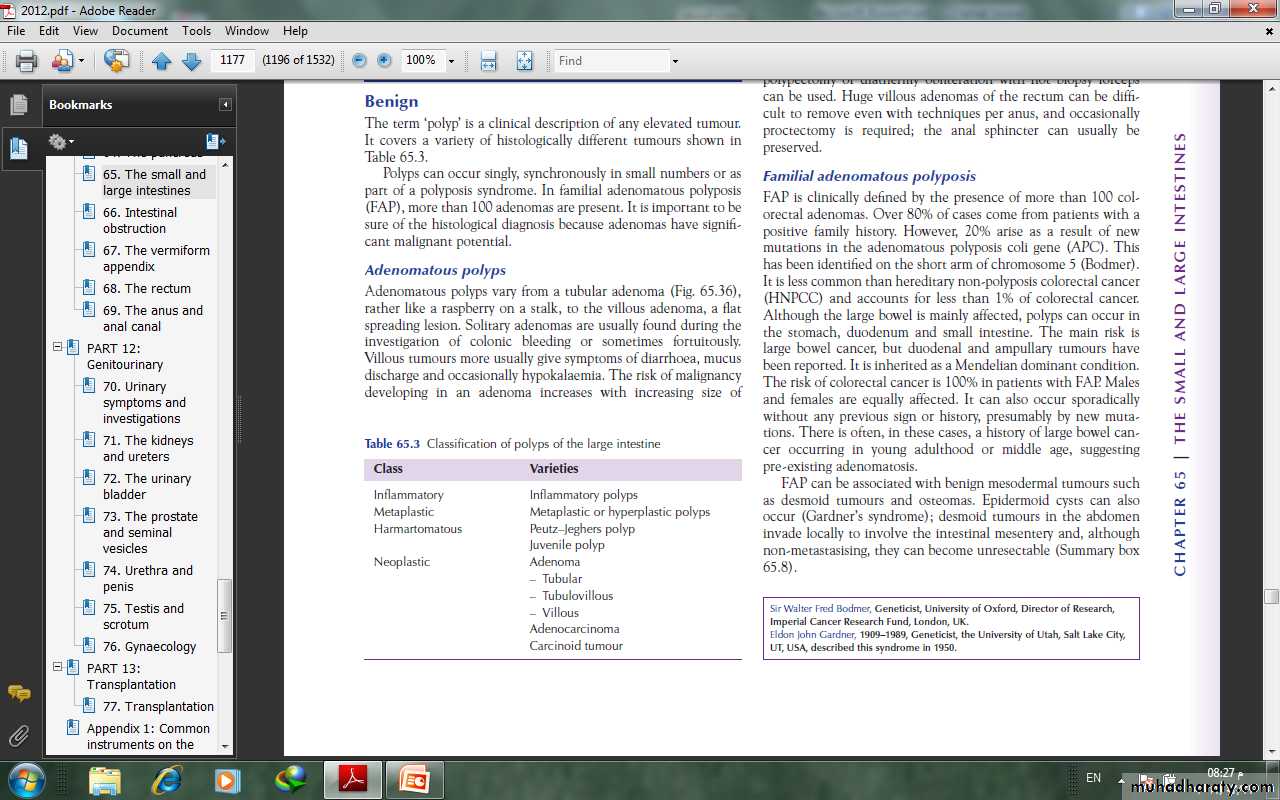
TUMOURS OF THE LARGE INTESTINEBenignThe term ‘polyp’ is a clinical description of any elevated tumour.Polyps can occur singly, synchronously in small numbers or aspart of a polyposis syndrome. In familial adenomatous polyposis(FAP), more than 100 adenomas are present. It is important to besure of the histological diagnosis because adenomas have significant malignant potential.
types of polyps--Adenomatous polypAdenomatous polyps vary from a tubular adenoma ,rather like a raspberry on a stalk, to the villous adenoma, a flatspreading lesion.Villous tumours more usually give symptoms of diarrhoea, mucusdischarge and occasionally hypokalaemia.
The risk of malignancy developing in an adenoma increases with increasing size of tumour; for example, in 1-cm-diameter tubular adenomas there is a 10% risk of cancer, whereas with villous adenomas over 2 cm in diameter, there may be a 15% chance of carcinoma.Adenomas larger than 5 mm in diameter are usually treatedbecause of their malignant potential.
Colonoscopic snare polypectomy or diathermy obliteration with biopsy forceps can be used. Huge villous adenomas of the rectum can be difficult to remove even with techniques per anus, and occasionally proctectomy is required.
Familial adenomatous polyposisFAP is clinically defined by the presence of more than 100 colorectal adenomas. Over 80% of cases come from patients with apositive family history. 20% arise as a result of newmutations in the adenomatous polyposis coli gene (APC). Thishas been identified on the short arm of chromosome 5
Although the large bowel is mainly affected, polyps can occur inthe stomach, duodenum and small intestine. The main risk islarge bowel cancer, but duodenal and ampullary tumours havebeen reported. It is inherited as a Mendelian dominant condition.The risk of colorectal cancer is 100% in patients with FAP. Malesand females are equally affected.
FAP can be associated with benign mesodermal tumours suchas desmoid tumours and osteomas. Epidermoid cysts can alsooccur (Gardner’s syndrome .desmoid tumours in the abdomeninvade locally to involve the intestinal mesentery and, althoughnon-metastasising, they can become unresectable.
Clinical featuresPolyps are usually visible on sigmoidoscopy by the age of 15 yearsand will almost always be visible by the age of 30 years.Carcinoma of the large bowel occurs 10–20 years after the onsetof the polyposis.
Symptomatic patientsThese are either patients in whom a new mutation has occurredor those from an affected family who have not been screened.They may have loose stools, lower abdominal pain, weight loss,diarrhoea and the passage of blood and mucus
Polyps are seen on sigmoidoscopy and double contrast barium enema. If in doubt, colonoscopy is performed with biopsies to establish the number and histological type of polyps. If over 100 adenomas are present, the diagnosis can be made confidently..
Asymptomatic patientsDirect genetic testing will reveal mutations in 80% of cases. The site of the mutation within the gene has important effectson the phenotype.If there are no adenomas by the age of 30 years, FAP isunlikely. If the diagnosis is made during adolescence, operation isusually deferred to the age of 17 or 18 years or when symptoms ormultiple polyps develop.
Screening policy1 At-risk family members are offered genetic testing in theirearly teens.2 At-risk members of the family should be examined at the ageof 10–12 years, repeated every year.3 Most of those who are going to get polyps will have them at 20years, and these require operation.4 If there are no polyps at 20 years, continue with 5-yearlyexamination until age 50 years; if there are still no polyps,there is probably no inherited gene.
TreatmentColectomy with ileorectal anastomosis has in the past been theusual operation because it avoids an ileostomy in a young patientand the risks of pelvic dissection to nerve function.
The alternative is a restorative proctocolectomy with anileoanal anastomosis. This has a higher complication rate thanileorectal anastomosis. It is indicated in patients with serious rectalinvolvement with polyps.
Hereditary non-polyposis colorectal cancer (Lynch’ssyndrome)This syndrome is characterised by increased risk of colorectalcancer and also cancers of the endometrium, ovary, stomach andsmall intestines. It is an autosomal dominant condition that iscaused by a mutation in one of the DNA mismatch repair genes– MLH1, MSH2, MSH6, PMS and PMS2. The lifetime risk of developing colorectal cancer is 80%
DiagnosisHNPCC can be diagnosed by genetic testing or Amsterdamcriteria II:• three or more family members with a HNPCC-related cancer,one of whom is a first-degree relative of the other two;• two successive affected generations;• one or more of the HNPCC-related cancers diagnosed beforethe age of 50 years;• exclusion of FAP.