
1
Pathology of the urinary system
The pathology of the kidney
Introduction:
Disease of the kidney are divided into four categories depending on which component of the
kidney is primarily affected; these are
a. Glomerular
b. Tubular
c. Interstitial
d. Vascular
This division is useful because:-
a. The early manifestations of each group of diseases tend to be distinctive
b. These groups differ in their pathogenesis for e.g. glomerular disease are often
immunologically mediated, whereas tubular and interstitial disorders are more likely to
be caused by toxic or infectious agents, however it should be noted that
1.
The interdependence of renal components translated into that damage to one
component is almost always affects secondarily the others
2.
All form of chronic renal disease tend ultimately to damage all four components of
the kidney thus eventuates in chronic renal failure (end stage kidney disease).
Glomerular diseases
:-
The glomerulus consist of an anastomosing network of capillaries invested by two layers of
epithelium; visceral and parietal . the visceral epithelium (podocytes) is an intrinsic part of the
capillary wall, whereas the parietal epithelium lines the Bowmans space (urinary space), the
cavity in which plasma ultrafiltrate first collects. The glomerular capillary wall is the filtration
unite and consists of the following structures:-
1. A thin layer of fenestrated endothelial cells (each hole is about 100 nm in diameter ).
2. Glomerular basement membrane (GBM), ultrastructurally made up of a thick, dense
central layer (lamina densa), and thinner, lucent peripheral layers (lamina rara interna &
externa)
3. The visceral epithelial cells (podocytes) that possess foot processes adherent to the
lamina rara externa of the basement membrane. Adjacent foot processes are separated
by 25- nm wide filtration slits bridged by a thin slit diaphragm composed in largely of
nephrin.
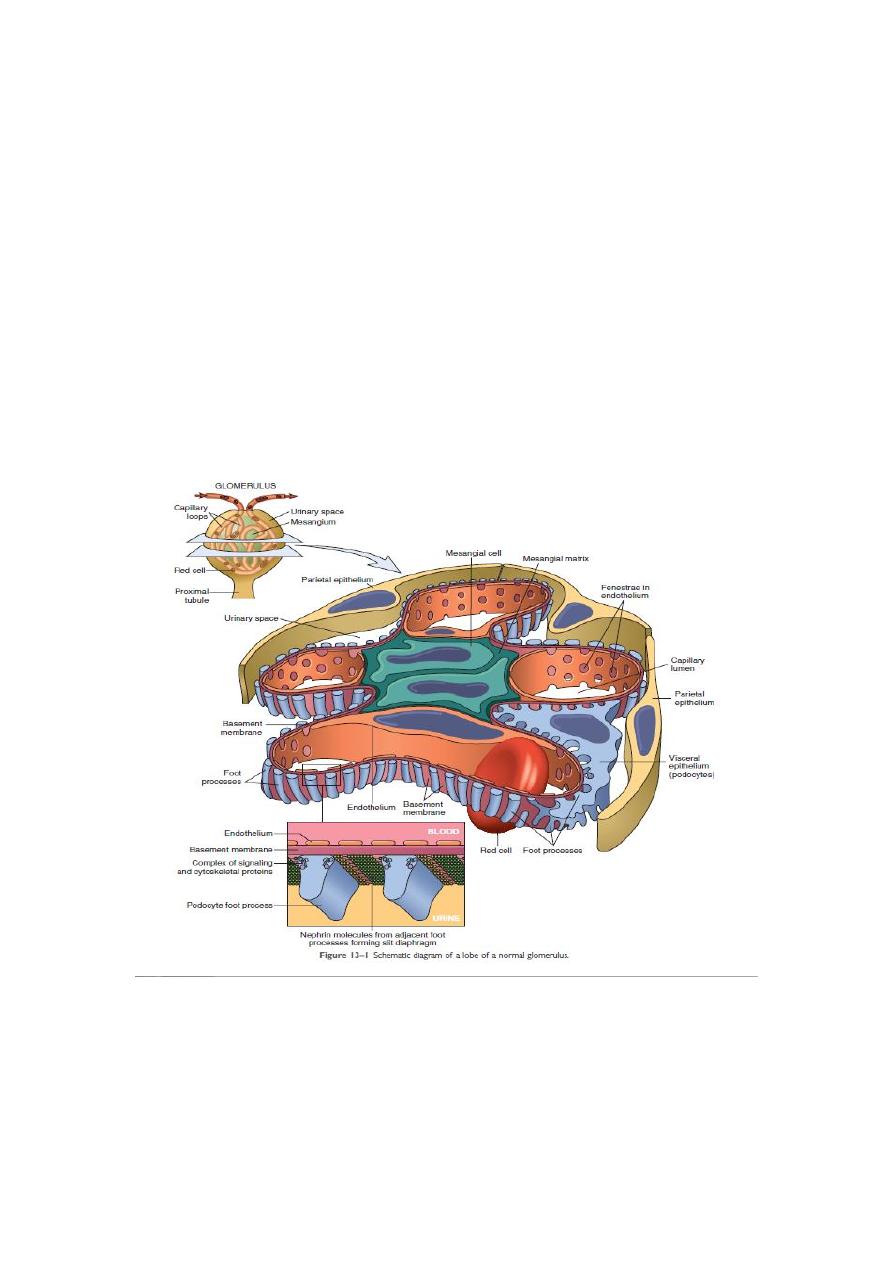
2
4. The entire glomerular tuft is supported by mesangial cells lying between the capillaries.
Basement membrane- like mechanical matrix forms a meshwork through which the
mesangial cells are scattered.
The glomerular basement membrane shows selective permeability, which is size dependent
and charge dependent. The major characteristics of glomerular filtration are:
1. A high permeability to water and small solutes
2. Almost complete impermeability to molecules of the size and molecular charge of
albumin.
3. More permeability to cation than anions
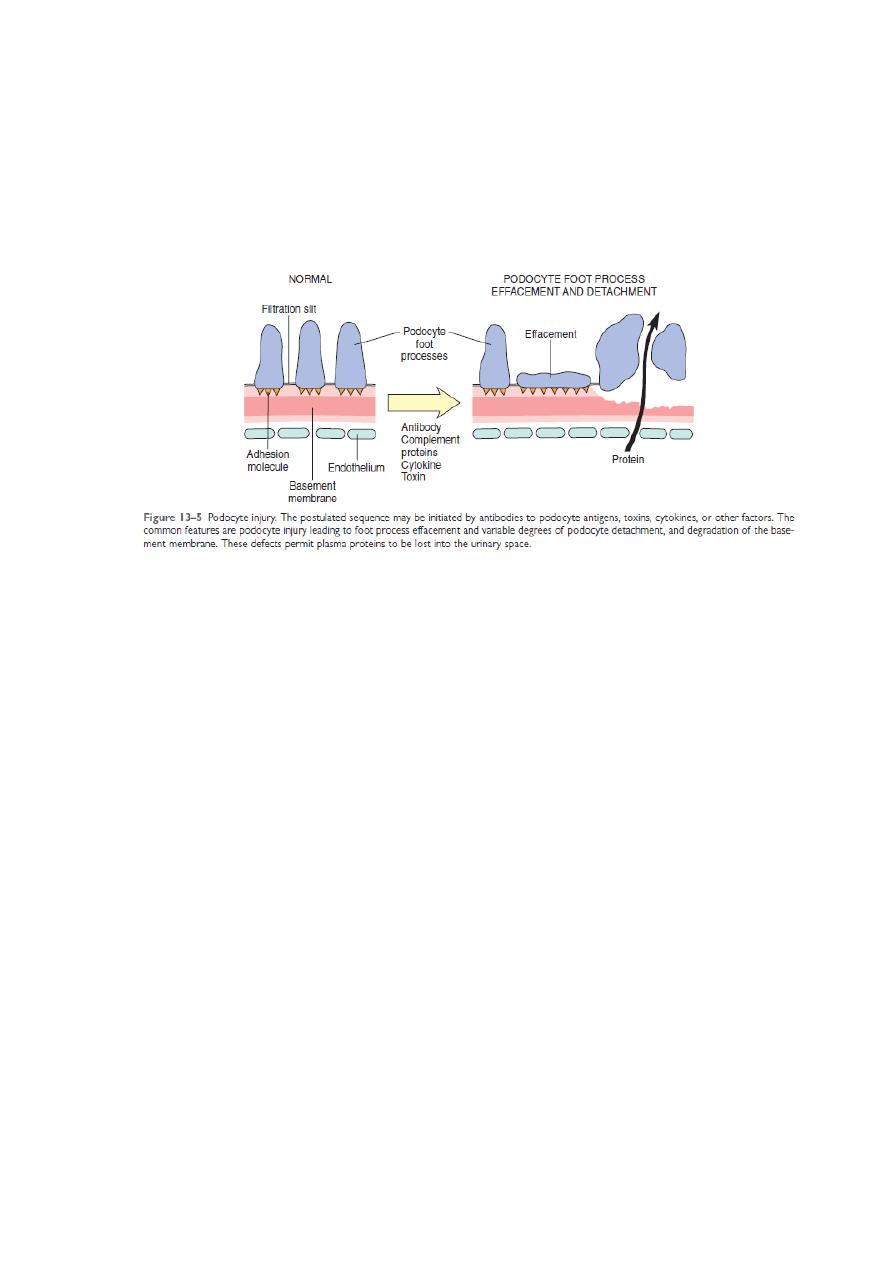
The podocyte is decisive(important) to the glomerular barrier function by providing a distal
resistance to the flow of water and a barrier to the filtration of proteins. It is also largely
responsible for synthesis of GBM component..
The pathogenesis of the glomerular diseases:-
Immune mechanisms (antibody – associated & cellular) underlie most primary and many
secondary glomerular diseases:
Circulating immune complex- mediated nephritis (type III hypersensitivity reactions)

3
With circulating immune complex- mediated disease, the glomerulus is an,, innocent
bystander,, because it is not responsible for their formation. The antigen in these complexes
may be:
a. Endogenous as in SLE or
b. Exogenous as in bacterial (streptococcal), viral (hepatitis B), parasitic (plasmodium
falciparum malaria), and spirocheatal ( Treponema Pallidum) infections.
c. Unknown as often the case in membranous nephropathy.
The antigen- antibody complexes are trapped in the glomeruli, where they produce injury
mainly through the activation of complement and the recruitment of the leukocytes. E.M
reveals the immune complexes as electron dense granular deposits in the glomerulus.
Mediators of immune injury:-
A major pathway of antibody initiated injury is activation of the complement that lead to
generation of chemotactic agents (mainlyC5a) and thus recruitment of the neutrophils and
monocytes . neutrophils in turn release.
1. Proteases, which cause GBM degradation
2. Oxygen- derived free radicals, which cause cell damage and
3. Arachidonic acid metabolites, which contribute to reduction in GFR.
In some cases however complement – dependent (but not neutrophil- dependent) injury occurs
through the effect of the C5-C9 lytic component (membrane attack complex) of complement
which causes
1. Epithelial cell detachment and
2. Stimulation of the mesangial and epithelial cells to secrete various mediators of cell
injury.
3. Up- regulation of transforming growth factor-β (TGF- β) receptors on podocytes; TGF-β
stimulates synthesis of extracellular matrix, thus giving rise to altered GBM composition
and thickening
Nephritis caused by in situ immune complexes:-
Antibodies in this form of injury react directly with planted antigens in the glomerulus:-
The best –characterized disease in this group is anti-GBM antibodies. It results from the
formation of autoantibodies directed against the GBM. Deposition of these antibodies creates a
linear pattern of staining when visualized by I.F.M . this is in contrast with granular pattern
described for other forms of immune complex-mediated nephritis. Sometimes the anti- GBM
antibodies cross react with the basement membranes of the lung alveoli, result in combined
lung and kidney lesions (Goodpasture syndrome).
4
Planted antigens also include DNA bacterial products, aggregated IgG which deposit in the
mesangium because of their size. Most of these planted Ags induce a granular pattern of
immunoglobulin deposition as seen by I.F.M
Cell mediated immune GN:-
T cell- mediated injury may account for some cases of GN in which either there are no deposits
of Ab or immune complexes or the deposits do not correlate with the severity of damage
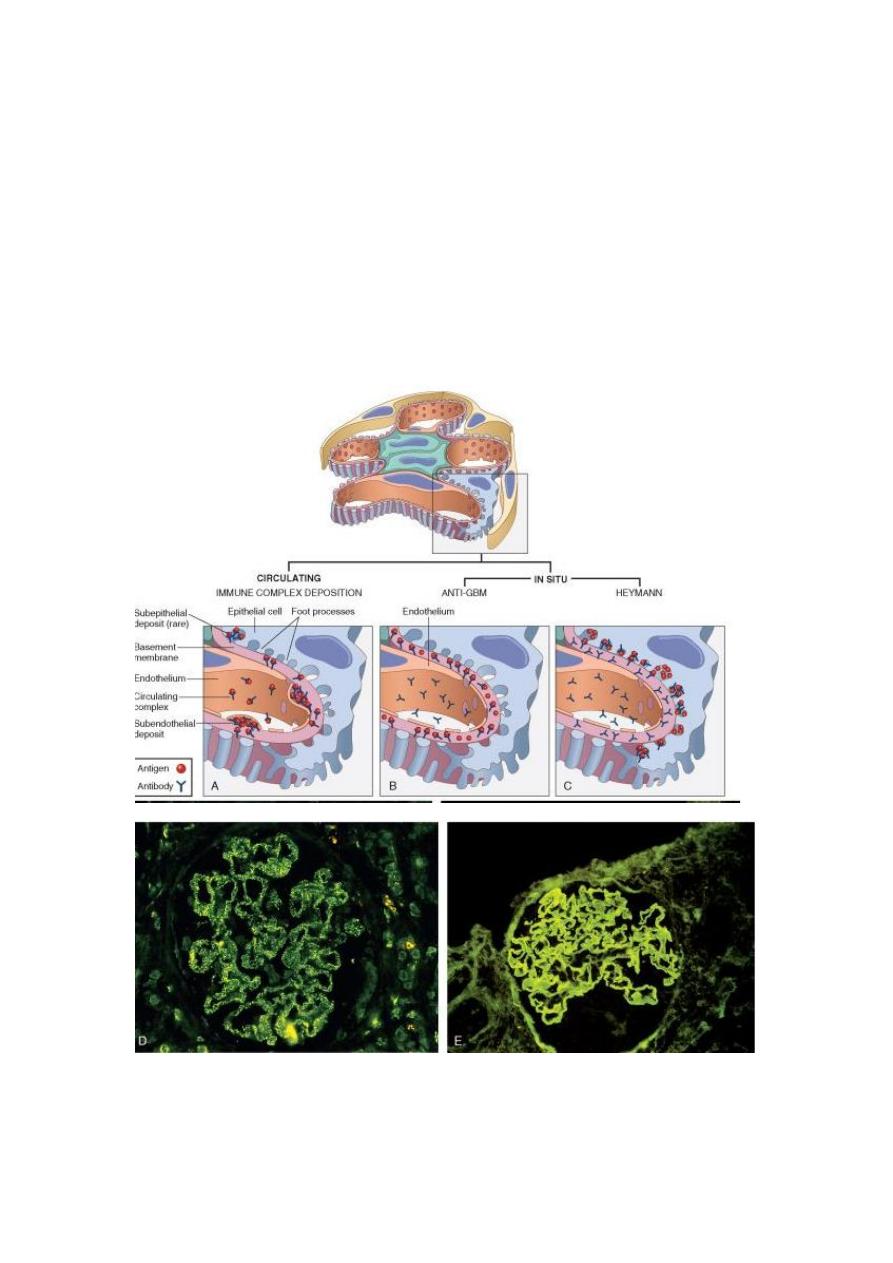
FIGURE 20-4 Antibody-mediated glomerular injury can result either from the deposition of
circulating immune complexes (A) or, more commonly, from in situ formation of complexes
exemplified by anti-GBM disease (B) or Heymann nephritis (C). D and E, Two patterns of
deposition of immune complexes as seen by immunofluorescence microscopy: granular,

5
characteristic of circulating and in situ immune complex nephritis (D), and linear, characteristic
of classic anti-GBM disease (E).
The nephrotic syndrome
:-
This refers to a clinical complex that is includes:-
1. Massive proteinuria ( daily protein loss of 3.5 gm or more in adults)
2. Hypoalbuminemia ( plasma albumin level less than 3 gm)
3. Generalized edema
4. Hyperlipidemia and lipiduria
The initial event is the derangement of the capillary walls that leads to increased permeability
of plasma protein into the glomerular filtrate. With long standing or extremely heavy
proteinuria, serum albumin is decreased resulting in hypoalbuminemia.
The generalized edema is in turn, a consequence of the drop in the plasma colloid osmotic
pressure as a result of hypoalbuminemia and retention of salt and water by the kidney.
As the fluid escape from the vascular tree into the tissues, there is concomitant drop in plasma
volume, with diminished glomerular filtration. Compensatory secretion of aldosterone along
with the reduced GFR and reduction of secretion of natriuretic peptides, promotes retention
salt and water by the kidneys, thus further aggravating the edema. By repetition of this chain of
events, generalized edema (anasarca) may develop.
It is possible that hypoalbuminemia triggers increased synthesis of lipoproteins in the liver and
thus hyperlipidemia. the lipiduria reflects the increased permeability of the GBM to
lipoproteins.
The relative frequencies of the several causes of the nephrotic syndrome is almost always
caused by a primary kidney disease, whereas among adults it is often due to renal
manifestations of a systemic disease. The most frequent systemic causes of the nephrotic
syndrome in adults are (DM, amyloidosis, SLE)
The most primary glomerular lesions that lead to the nephrotic syndrome are:
1. Focal and segmental glomeruloscrelrosis (FSGS), which is more important in adult
2. Minimal changes disease (MCD), which is more important in children.
3. Membranous nephropathy
4. Membanoproliferative GN
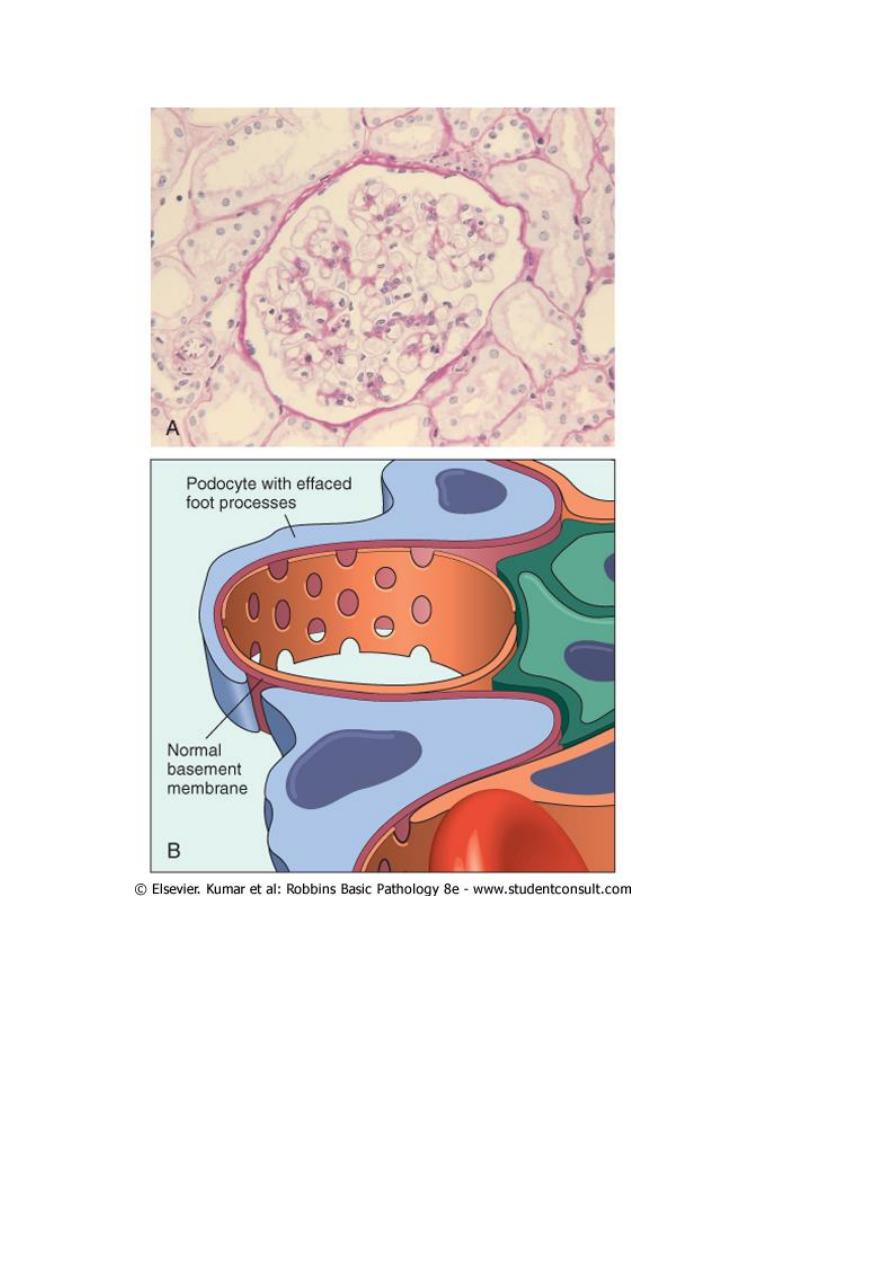
Minimal change disease (MCD) (lipoid nephrosis):-
This is the most frequent cause of nephrotic syndrome in children mostly between ages 1 and 7
years (65%). The glomeruli have normal appearance under L.M. however E.M. shows diffuse
6
effacement of podocyte damage. The cells of the proximal convoluted tubules are often heavily
loaded with protein droplets and lipids secondary to tubular reabsorption of the leaking
lipoproteins. The renal function is preserved in most individual . the protein loss is confined to
the smaller serum proteins, chiefly albumin (selective proteinuria). The prognosis in children
with the disorder is generally good, more than 90% of cases respond to a short course of
corticosteroid
therapy.
7
Minimal change disease. A, Under the light microscope the PAS-stained glomerulus appears normal,
with a delicate basement membrane. B, Schematic diagram illustrating diffuse effacement of foot
processes of podocytes with no immune deposits.
Focal and segmental glomerulosclerosis:-
Is characterized histologically by sclerosis (fibrosis) affecting some but not all the glomeruli
(focal) and involving only segments of each glomerulus (segmental).FSGS is either primary or
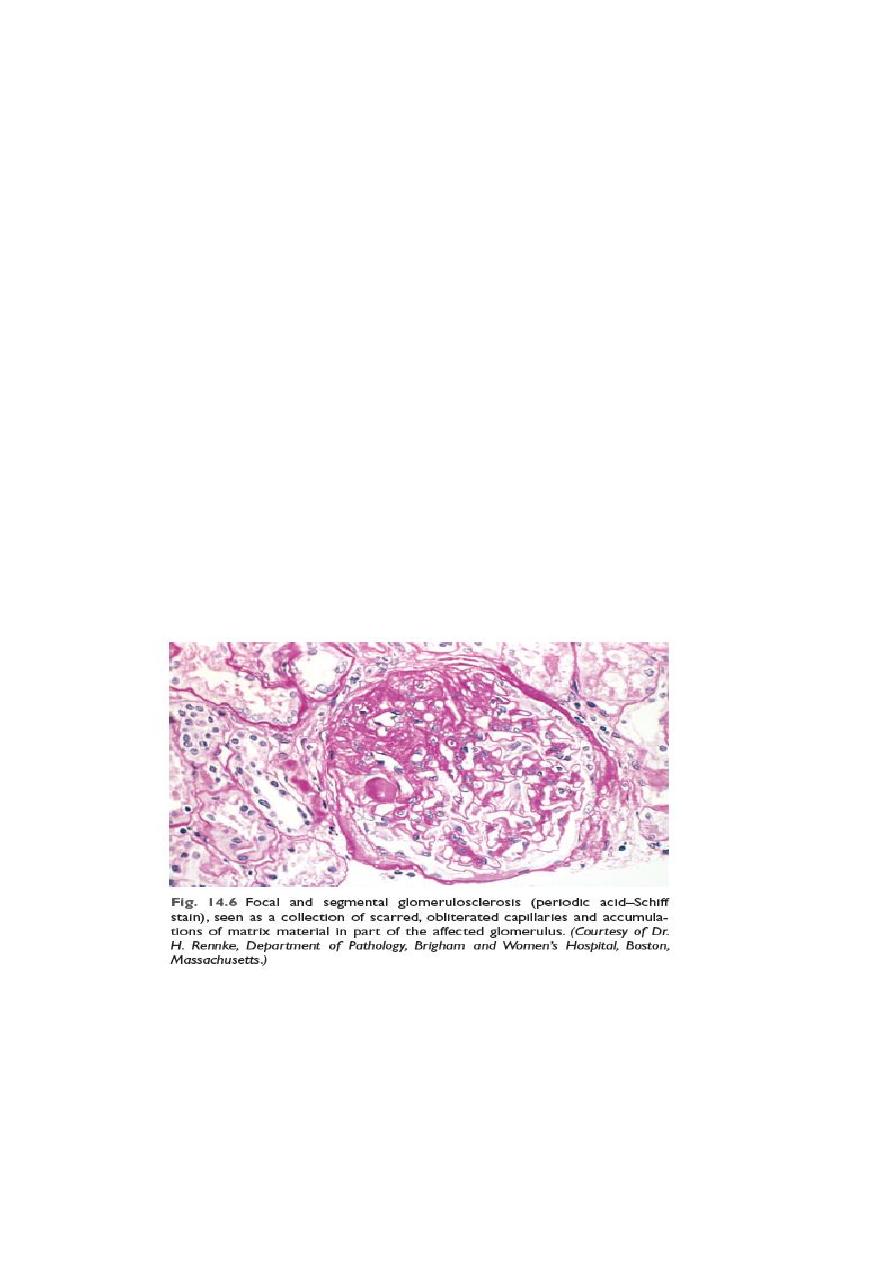
8
secondary. The former is the common cause of nephrotic syndrome in adults (30%) and
frequent cause in children (10%). The secondary form is seen with :
1. HIV immunodeficiency or heroin abuse (HIV nephropathy , heroin nephropathy)
2. IgA nephropathy
3. Maladaptation after nephron loss
4. Mutation affecting cytoskeletal proteins of podocytes (e.g. nephrin) (inherited form).
Unlike MCD there is higher incidence of hematuria and hypertension; the proteinuria is
nonselective and the response to the corticosteroid therapy is poor. At least 50% of individuals
with FSGS develop end stage renal failure with 20 years of diagnosis. The pathogenesis of
primary FSGS is unknown.
As with MCD, permeability – increasing factors produced by lymphocytes have been proposed.
The entrapment of plasma proteins and lipids occur in foci of injury where the sclerosis occur .
FSGS initially affects focally the juxtamedullary glomeruli. With progression eventually all level
of the cortex are affected.
The affected segment of the glomerulus shows increased mesangial matrix , obliterated
capillary lumens and deposition of the hyaline masses . in time progression of the disease lead
to global sclerosis of the glomeruli with secondary tubular atrophy and interstitial fibrosis.
About 50% of individuals suffer renal failure after 10 years.
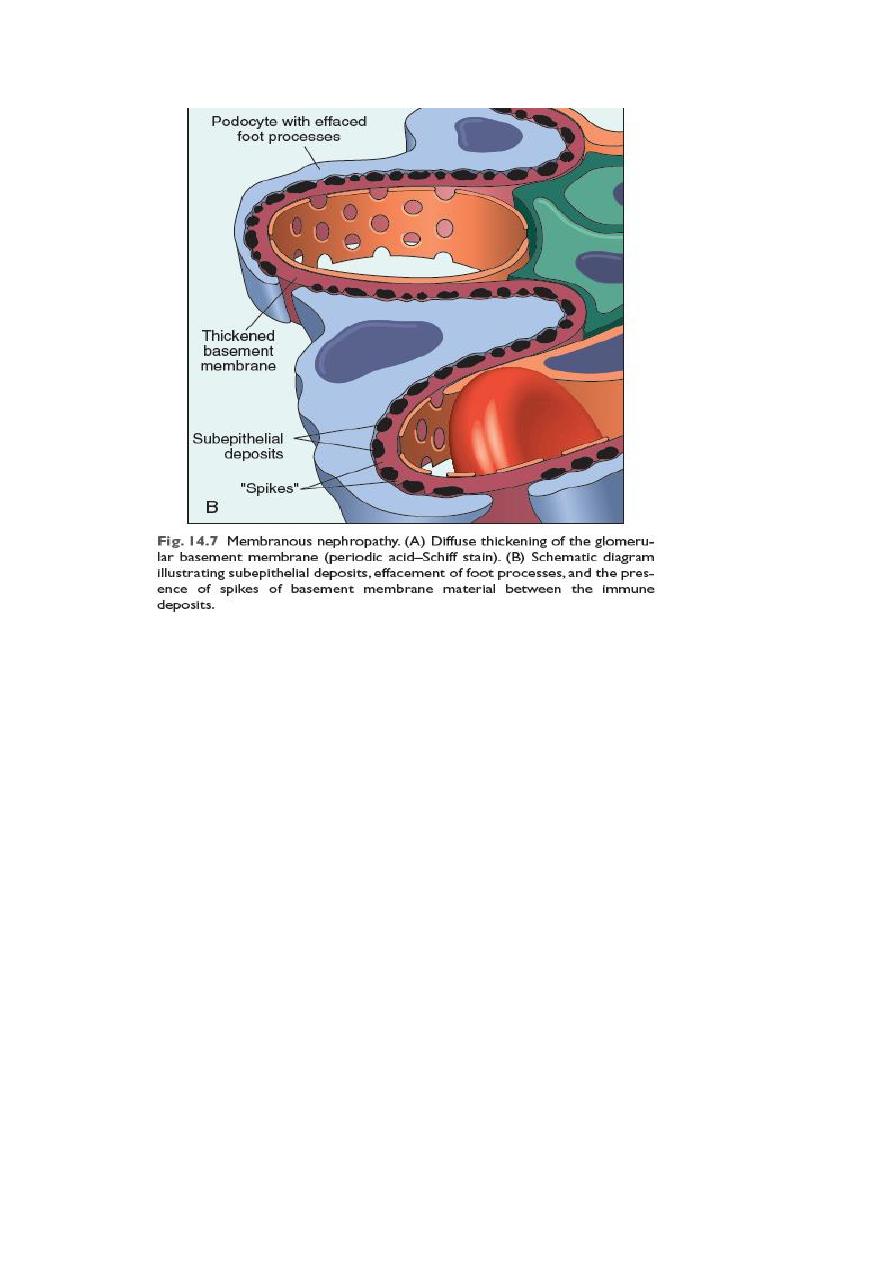
Membranous nephropathy (membranous glomerulonephritis, MGN):-
This slowly progressive disease most commonly in adults 30 -50 years of age the disease is of
idiopathic (primary in about 85%) of cases. In the remainder it may be secondary to other
disorders, including :-

9
1. Infections(chronic hepatitis B, syphilis, malaria, schistosomiasis)
2. Malignancy especially lung , colonic carcinoma and melanoma
3. Autoimmune disease e.g. SLE
4. Exposure to inorganic salts (gold, mercury)
5. Drugs (penicillamin, captopril, NSAID)
MGN is a chronic immune complex nephritis, most idiopathic form are considered autoimmune
diseases caused by antibodies to renal GBM autoantigen. There seem to be a direct action of
the C5b-C9 (the membrane attack complex) on the podocytes and mesangial cells, inducing
them to liberates protease and oxidants that can cause the damage .
The basic changecs microscopically is the diffuse thickening of the GBM. By E.M. this thickening
is caused by subepithelial deposits that are separated from each other by small spike like
protrusions of GBM matrix (spike and dome pattern ); these can be highlighted by silver stains.
With progression these spikes close over the deposits, to incorporate them into the GMB.
Podocytes show effacement of foot processes. Eventually the glomeruli become gradually
sclerosed.
IFM shows typical graunular depositis of immunoglobulin and complement along the GBM
nonselective, involving globulins and albumin molecule . overall only 40% suffer progressive
disease terminating in renal failure after 2- 20 years.
10
Membranoproliferative glomerulonephritis:-
This is manifested histologically not only by GBM thickening but also by proliferation of the
glomerular cells.
It account for up to 10% of cases of primary nephrotic syndrome in children and adults .
some individual present only with hematuria or subnephrotic proteinuria; other have
combined nephrotic-nephritic picture.
Two major types of MPGN (I and II) are recognized; type I is far more common (80% of cases).
Different pathogenic mechanisms are involved in the development of type I and type II disease .
most cases of type I MPGN seem to be caused by circulating immunocomplexes. But the
inciting antigen is not known (primary); it also occur as a secondary form in association of
hepatitis B and C antigenemia ,SLE, and extra renal infections.
The fundamental abnormality in type II appears to be excessive complement activation .
by light microscopy both types of MPGN are similar. The glomeruli are large with an
accentuated lobular appearance, and proliferation of mesangial and endothelial cells as well as
leukocytic infiltration.
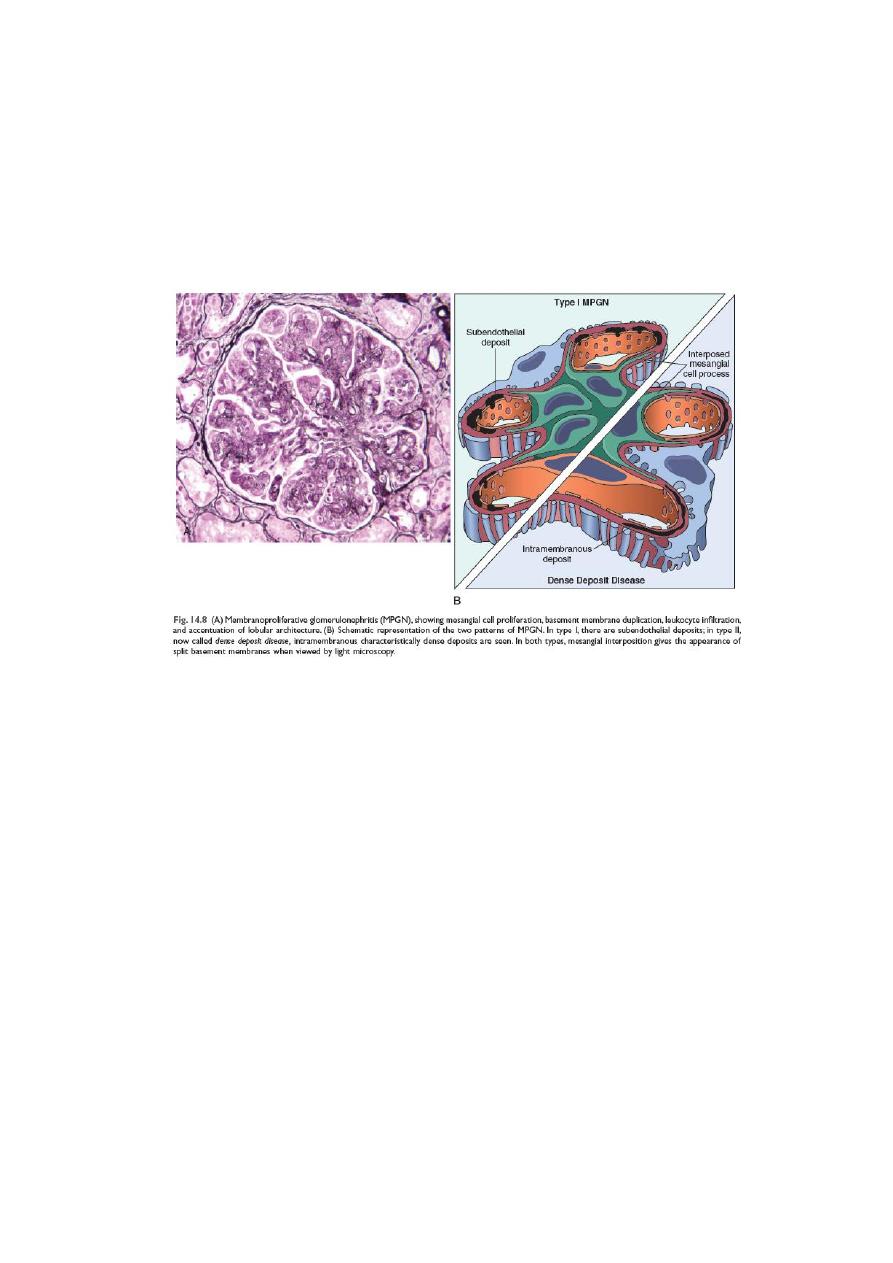
11
The GBM is thickened and the glomerular capillary wall often shows a double contour or ''tram
track'' appearance especially evident in silver or periodic acid Schiff (PAS) stains. This is caused
by ''splitting of the GBM '' due to inclusion(insertion) within it of processes of mesangial and
inflammatory cells . type I AND type II have different ultrastructural and I.F.M features.
The prognosis of MPGN is generally poor in that 40 % of the cases progressed to end stage
renal failure. Type II MPGN (also caused dense- deposit disease ) has a worse prognosis.
The nephritic syndrome
:-
This is a clinical complex, usually of acute onset characterized by
1. Hematuria
2. Oliguria with azotemia
3. Hypertension
The lesions that cause nephritic syndrome have in common proliferation of the cells within the
glomeruli, accompanied by leukocytic infiltration.
This inflammatory reaction injures the capillary walls permitting escape of the red cell into the
urine and induces hemodynamic changes that lead to reduction in the GFR .
the reduced GFR is manifested clinically by oliguria, fluid retention, and azotemia. Hypertension
is the result of both the fliud retention and excessive renin release.
The acute nephritic syndrome may be secondary to systemic disorders such as SLE or it may be
the result of primary glomerular disease e.g. acute postinfectious GN.

12
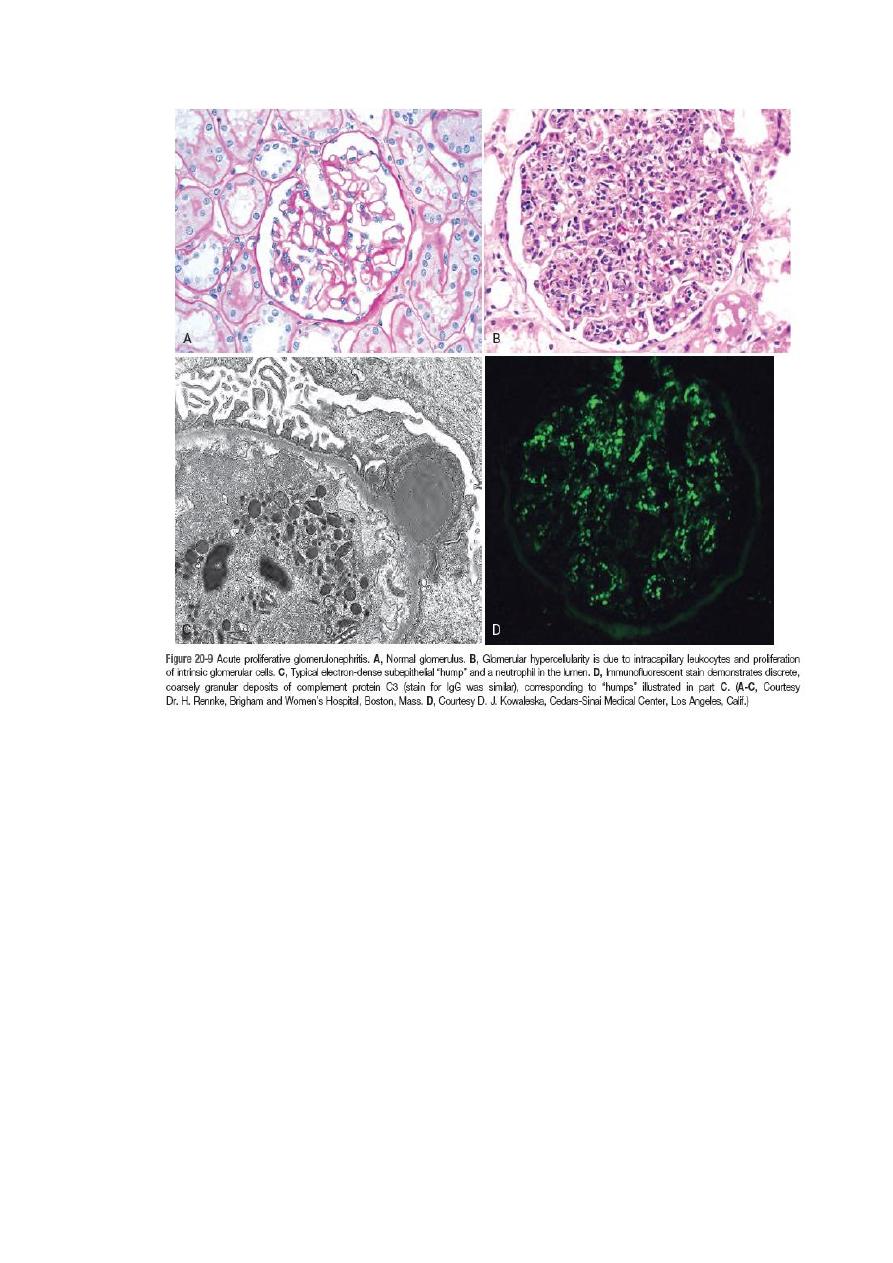
Acute postinfectious (post streptococcal) GN :-
This is typically associated with streptococcal infection, but other infectious agents may be
responsible. The latter include certain pneumococcal and staphylococcal infections, as well as
common viral diseases such as mumps, measles, chichenpox and hepatitis B and C .
The classic case of PSGN develops in children 1-4 weeks after recovery from nephritogenic
''strain of β- hemolytic group A streptococcal infection usually of the pharynx or skin.
Immune complex deposition is involved in the pathogenesis.
The relavent Ag are probably streptococcal proteins. Serum complement level are low and
serum anti streptolysin O antibodies titers are elevated.
Characteristically the histology shows a uniform increased cellularity of the glomerular tufts .
that affect nearly all glomeruli. This increases cellularity is caused both by proliferation and
swelling of both endothelial and mesangial cells as well as by a neutrophilic and monocytic
infiltrate .
E.M show subepithelial humps.
IFM display these immune complexes as scattered granular deposits of IGg and complement
within the capillary walls.
Recovery occur in most children . (conversely up to 50% of adult develop end stage renal failure
.
13
IgA nephropathy (Berger disease)
:-
Usually affects children and young adults as episodes of gross hematuria occurring within 1 to 2
days of nonspecific upper respiratory tract infections to last several days and then subsides only
to recur every few months.
IgA nephropathy is the most common cause of recurrent microscopically and gross hematuria
and is the most common glomerular disease revealed by renal biopsies worldwide .
the pathogenic hallmark is the deposition of the IgA in the mesangium. IgA may be viewed as a
localized renal variant of Henoch – Schonlein purpura, which is also characterized by IgA
deposition in the masangium but it is a systemic syndrome characterized by purpuric rash,
abdominal pain and arithritis. Microscopically, the glomeruli may be normal or show one of the
following:
1. Focal proliferative GN

14
2. Diffuse mesangioproliferative GN
3. Crescentic GN (rare)
The characteristic IFM picture is of mesangial deposition of IgA. Electron microscopy shows
mesangial electron – dense deposits.
Serum IgA is increased in 50% of patients due to its increased production in the marrow
presumably in response to respiratory or GIT exposure to viruses, bacteria, or food proteins.
The deposition of IgA and IgA- immune complexes in the mesangium activate the alternative
complement pathway and initiate glomerular injury. Slow progression to chronic renal failure
occurs in up to 50% of cases.
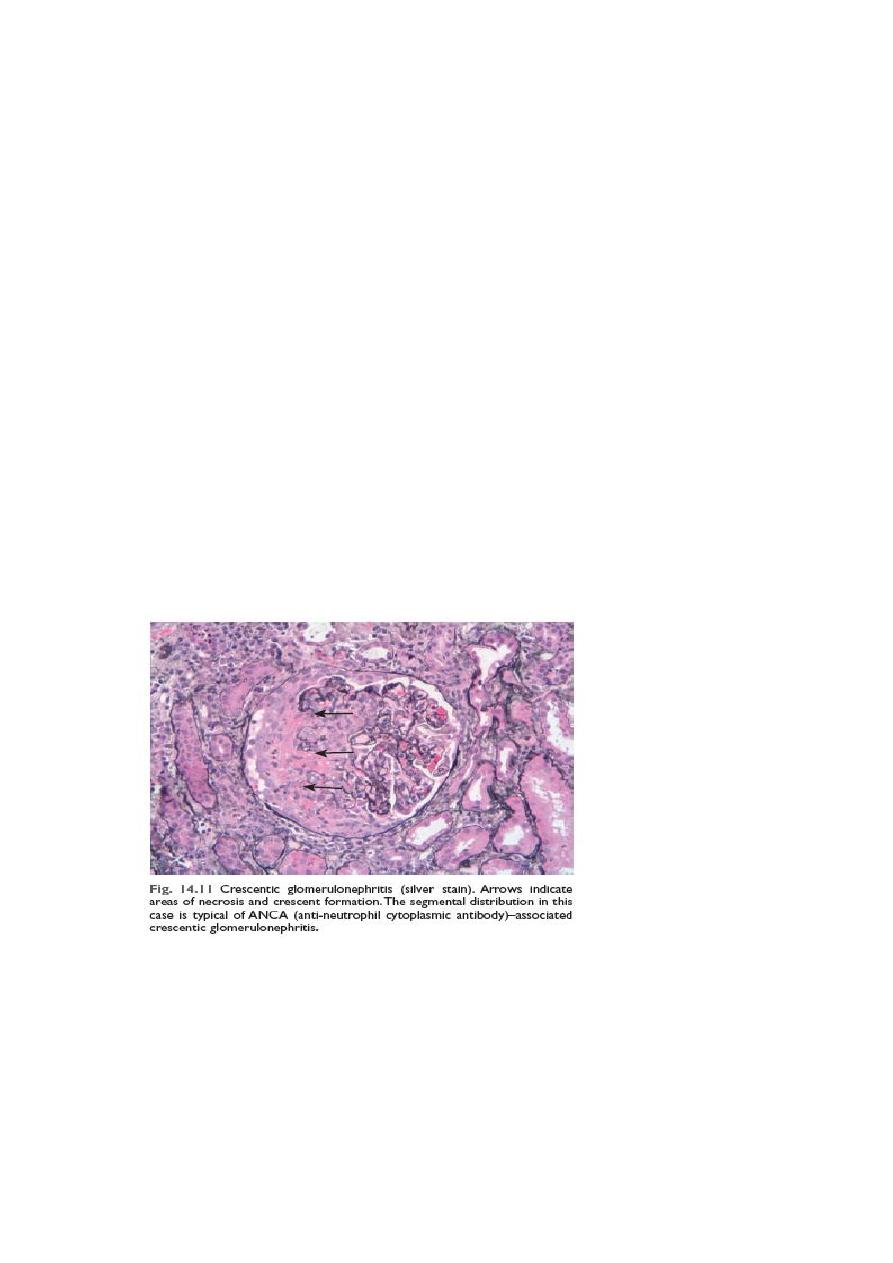
Rapidly progressive (Crescent) glomerulonephritis (RPGN; Cr GN):-
This is a clinical syndrome associated, irrespective of the etiology, with glomerular crescents;
these are produce by proliferation of the parietal epithelial cells associated with infiltration by
monocytes and macrophages. Cr GN is characterized clinically by:-
1. Rapidly progressive loss of renal function
2. Nephritic syndrome AND Severe oliguria (often)
3. Death from renal failure within weeks to months (if untreated)
A practical classification divide Cr GN into three groups on the basis of immunoglobuline
findings. In each group the disease may associated with a known disorder or it may be
idiopathic.
Type I (anti-GBM antibody):
● Idiopathic
● Goodpasture syndrome
This group is characterized by linear IgG deposits along the GBM. In some of these individuals
the anti-GBM antibodies also bind to alveolar capillary basement membranes to produce the
clinical picture of pulmonary hemorrhage associated with renal failure ( Goodpasture
syndrome). In idiopathic cases the renal involvement occur in the absence of pulmonary
disease. Anti GBM antibodies are present in the serum and are helpful in diagnosis.
IFM is characteristics with strong linear staining of deposited IgG and C3 along the GBM; these
deposits are not visualized by E.M
Type II (immune complex):-
1. Idiopathic
2. Postinfectious
3. SLE
4. Henoch –Schonlien purpura/ IgA nephropathy
15
In all of these cases, IFM shows the characteristic granular pattern of staining of the GBM and
or mesangium for immunoglobulin and or complement.
Type III (pauci-immune) ANCA associated:-
● Idiopathic
● Wegener granulomatosis
● Microscopic angitis
This group is defined by the lack morphologically of both anti-GBM antibodies and immune
complexes deposition. Most of these individuals have antinutrophil cytoplasmic antibodies
(ANCA) in the serum.
IF studies for immunoglobulin and complement are negative (cf of type I and II) and there are
no ultrastructural deposits.
The onset of RPGN is much like that of the nephritic syndrome. proteinuria sometimes
approaching nephrotic range may occur.
The prognosis can be related to the number of crescents; those with crescents in less than 80%
of the glomeruli have a better prognosis than those with higher percentage of crescents.
Chronic glomerulonephritis:-
Is one of the outcomes of the various glomerular diseases already discussed. It is an important
cause of end stage renal disease.
Among all individuals who require chronic hemodialysis or renal transplantation, 30-50% have
the diagnosis of chronic GN. By the time chronic GN is discovered, the glomerular changes are
so advanced that it is difficult to detect the nature of the original lesion.
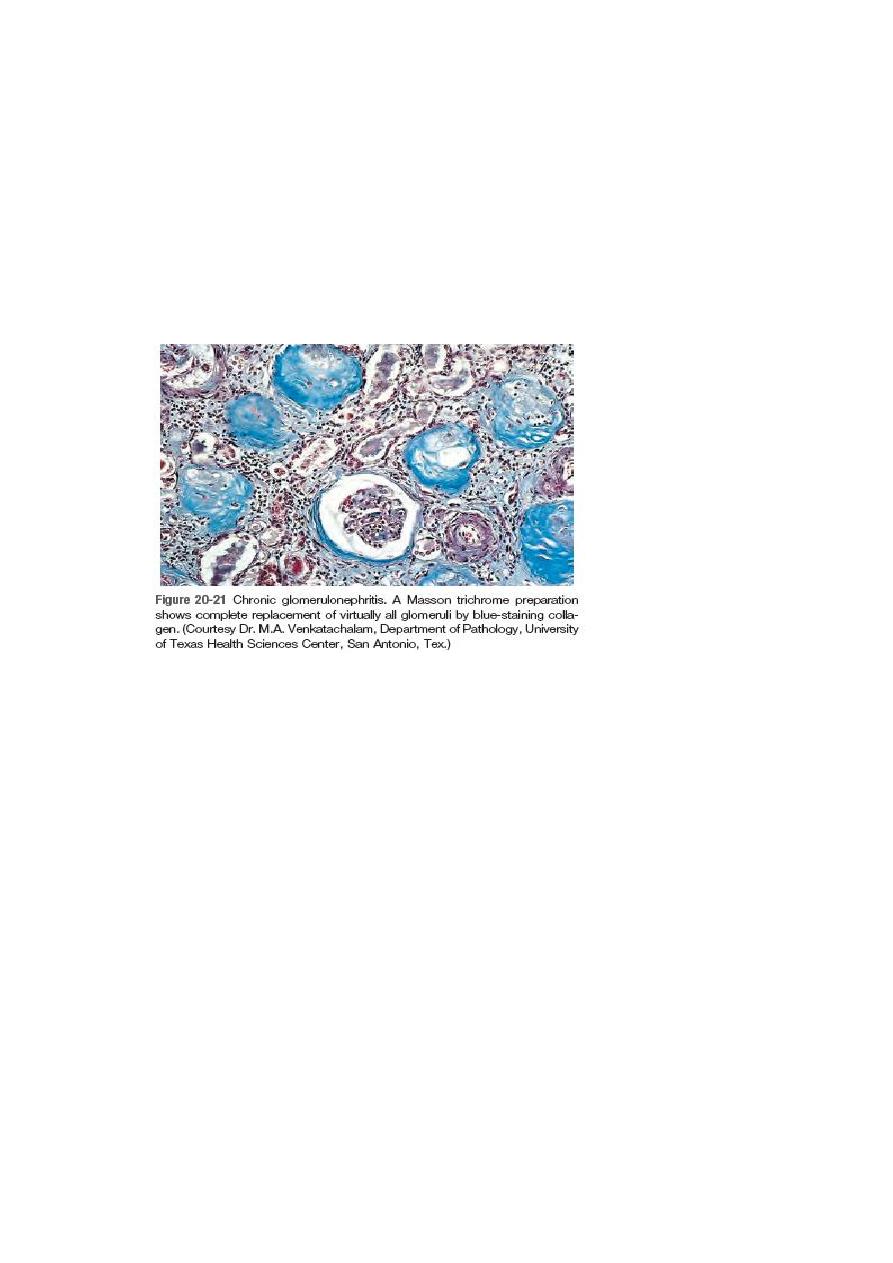
16
Classically the kidneys are symmetrically contracted with red brown surface.
Microscopically the feature common to all cases is advanced scaring of the glomeruli.
Sometimes to in the point of complete sclerosis.
There is relentless progression to uremia and death. The rate of the progression is extremely
variable. Renal dialysis and kidney transplantation alter this course and allow long term
survival.
Tubulointerstitial diseases:-
Most form of tubular diseases also involve the interstitium , so the two are discuss together.
Under this heading are two categories:-
1. Inflammatory involvement of the tubules and the interstitium (tubule-interstitial
nephritis)
2. Ischemic or toxic tubular necrosis (ATN) leading to acute renal failure.
Tubulointerstitial nephritis (TIN):- is a group of inflammatory disease of the kidneys primarily
involve the interstitium and tubules. The glomeruli are spared or affected late in the course .
TIN is subdivided into:-
1. Bacterial TIN : the renal pelvis is prominently involved (pyelonephritis)
2. Nonbacterial TIN these include tubular injury resulting from drugs, metabolic disorders
(hypokalemia), physical injury (irradiation), viral infection, immune reactions.
Pyelonephritis:- this divided into acute and chronic form.
17
Acute pyelonephritis:- is a common bacterial suppurative inflammation of the kidney and the
renal pelvis, and an important manifestation of the UTI . the great majority of cases of
pyelonephritis are associated with lower UTI (cystitis, prostitis, urethritis). Ecoli. Is by far the
most common offender. Other important organisms are proteus , kelbsiela, enterobacter and
pseudomonas. These are usually associated with recurrent infections, especially due to urinary
tract manipulations or congenital or acquired anomalies
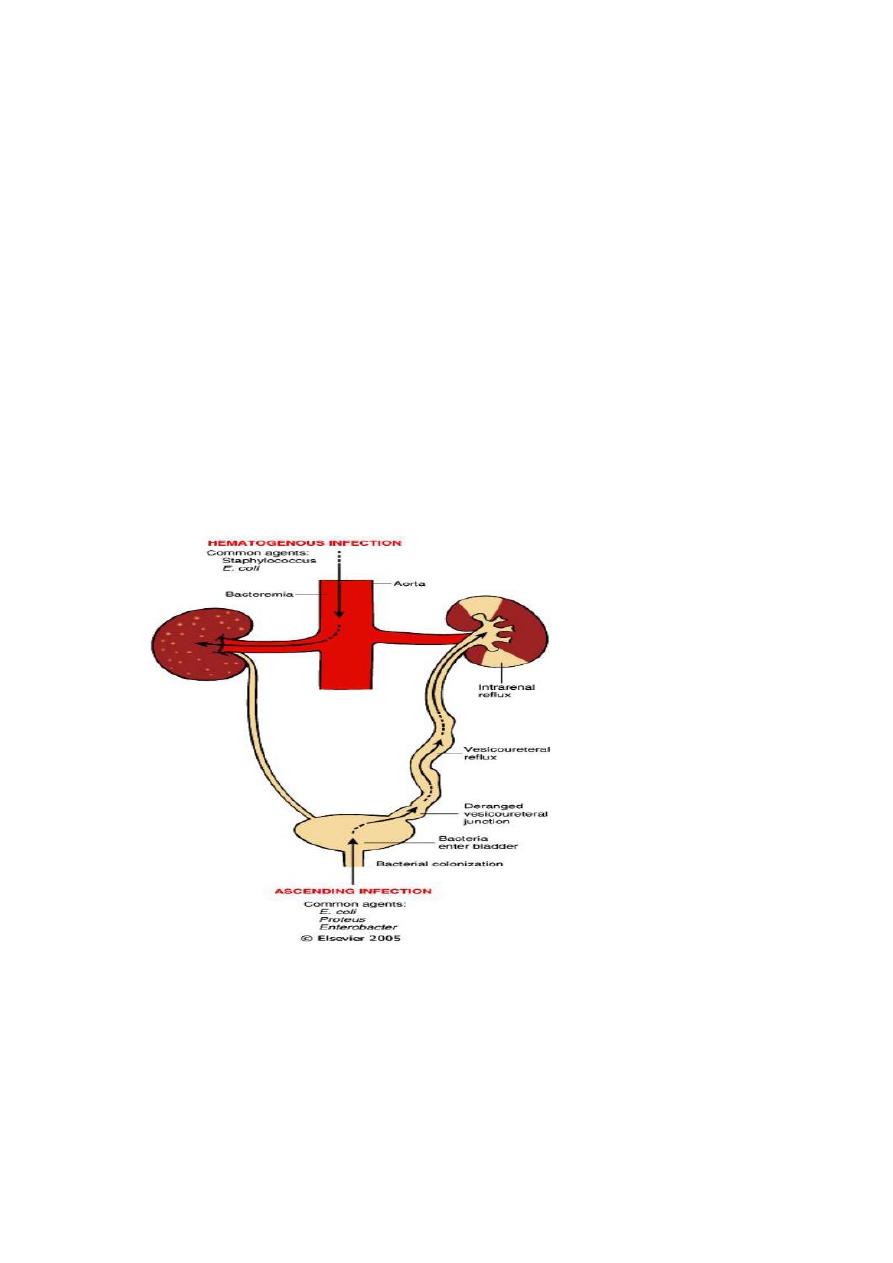
Pathogenesis:-
Bacteria can reach the kidneys either through the blood stream (hematogenous)(descending
infection) or from the lower urinary tract (ascending infection). The former is exemplified by
acute pyelonephritis complicating septicemia or infective endocarditis. Ascending infection
from the lower urinary tract is the most common & is an important rout by which bacteria
reach the kidney. The evolution of acute pyelonephritis occur through the following steps:
1. Bacterial adhesion to urethral urothelium is influenced by genetically determined
propertitis of both urothelium and the offending bacterial facilitate
2. Gaining access to the bladder is by growth expansion of the colonies and by moving
against the urine out flow, the latter is overcome by urethral instrumentation including

18
catheterization and cystoscopy. In the absence of instrumentation, UTI most commonly
affects females because of factors that facilitate entry of bacteria to the bladder these
are:
a) The close proximity of the urethra to the enteric bacteria loaded rectum favoring
colonization
b) The short urethra
c) Trauma to the urethra during sexual intercourse (honeymoon cystitis).
3. Outflow obstruction: normally bladder urine is sterile as a result of the antimicrobial
properties of the bladder mucosa and the flushing action of periodic voiding of urine.
With outflow obstruction or bladder dysfunction, these natural defenses are
overwhelmed, setting the stage for the UTI . obstruction at the level of the urinary
bladder result in incomplete emptying and increase residual volume of the urine . in the
presence of the stasis , bacteria introduce into the bladder can multiply freely , without
being flushed out or destroyed by the bladder mucosa. From the contaminated bladder
urine , the bacteria ascend along the ureter to infect the renal pelvis and paranchyma .
thus UTI is also frequently in DM because of the increased the susceptibility to infection
and neurogenic bladder which in turn predisposes to urine stasis
4. Vesicoureteral reflux (VUR):- incompetence of the vesicouretral orifice is required to
allow bacterial ascent along the ureter and then into the pelvis . the normal ureteral
insertion into the bladder is a competent one way valve that prevent retrograde flow of
urine , especially during micturition, when the intravesical pressure rises. An
incompetent vesicoureteral orifice allow the reflux of the bladder urine into the ureter.
This is termed vesicoureteral reflux (VUR). This condition is present in 40% of young
children with UTI and is usually a congenital defect. VUR can also be acquired in
individual with flaccid bladder resulting from spinal cord injury and with neurogenic
bladder dysfunction secondary to DM.
the effect of VUR is similar to that of an obstruction in that after voiding there is residual urine
in the urinary tract, which favors bacterial growth . furthermore, VUR affords a ready
mechanism by which the infected bladder urine can be propelled up to the renal pelvis
and father into the renal parenchyma through open ducts at the tips of the papillae
(intrarenal reflux).
Gross features of acute pyelonephritis:-
● one or both kidneys may be involved. The affected kidney may be normal in size or
enlarged.
● Characteristically ,discrete, yellowish raised abscesses are grossly apparent on the
renal surface. They are variably scaterd and may coalesce to form a single large
abscess.
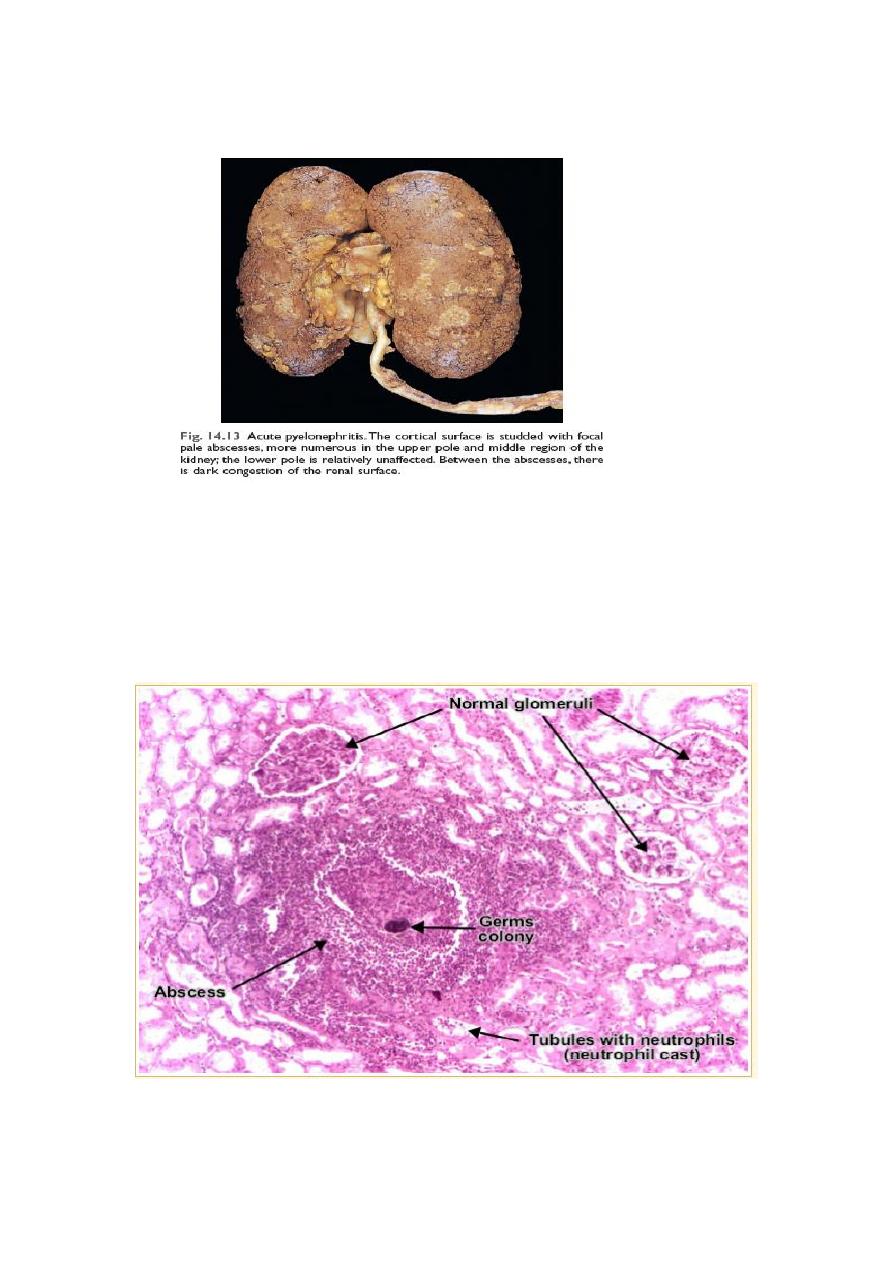
19
● When obstruction is prominent , the pus may fill the renal pelvis, calyces and ureter
producing pyonephrosis
microscopic fearures:-
● The characteristic features of acute pyelonephritis is suppurative necrosis with renal
parenchyma. Both the tubules and interstitium are infiltrated
● Large numbers of intratubular neutrophils frequently extending into the collecting ducts
giving rise to the characteristic white cell cast found in the urine
● Typically, the glomeruli are not affected.
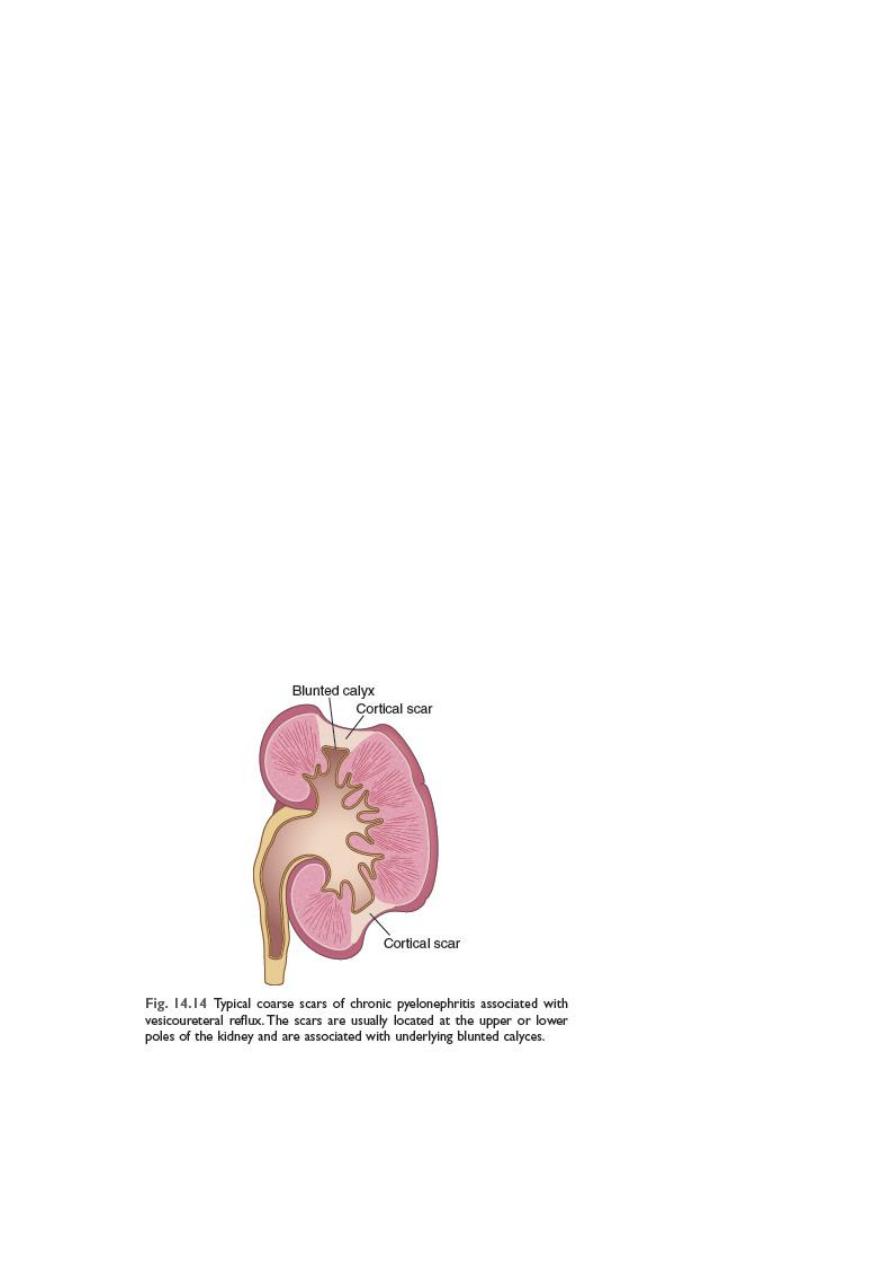
Chronic pyelonephritis (CPN) and reflux nephropathy:-
20
For the pathological diagnosis of the CPN two criteria must be present
1) Grossly visible scaring deformity of the pelvicalyceal system
2) Microscopic predominance of interstitial inflammation and fibrosis
CPN is an important cause of chronic renal failure . it can be divided into two forms.
1) Chronic obstructive pyelonephritis: recurrent infections superimposed on obstructive
lesions lead to recurrent bouts of renal inflammation and scaring, which eventually
cause chronic pyelonephritis. The disease can be bilateral as with congenital anomalies
of the urethra (posterior urethral valves), or unilateral such as occur with calculi and
unilateral obstructive lesions of the ureter
2) Chronic reflux –associated pyelonephritis is the more common form and results from
superimposition of a UTI on congenital vesicouretral reflux and intrarenal reflux. Reflux
may be unilateral or bilateral; , thus, the resultant renal damage is either unilateral or
bilateral
Gross features:-
● One or both kidneys may be involved, either diffusely or in patches, even when
involvement is bilateral , the kidneys are not equally damaged and therefore are not
equally contracted kidneys
The hallmark of CPN is scaring involving the pelvis & or calyces leading to papillary blunting and
marked calyceal deformities
Microscopic features:-
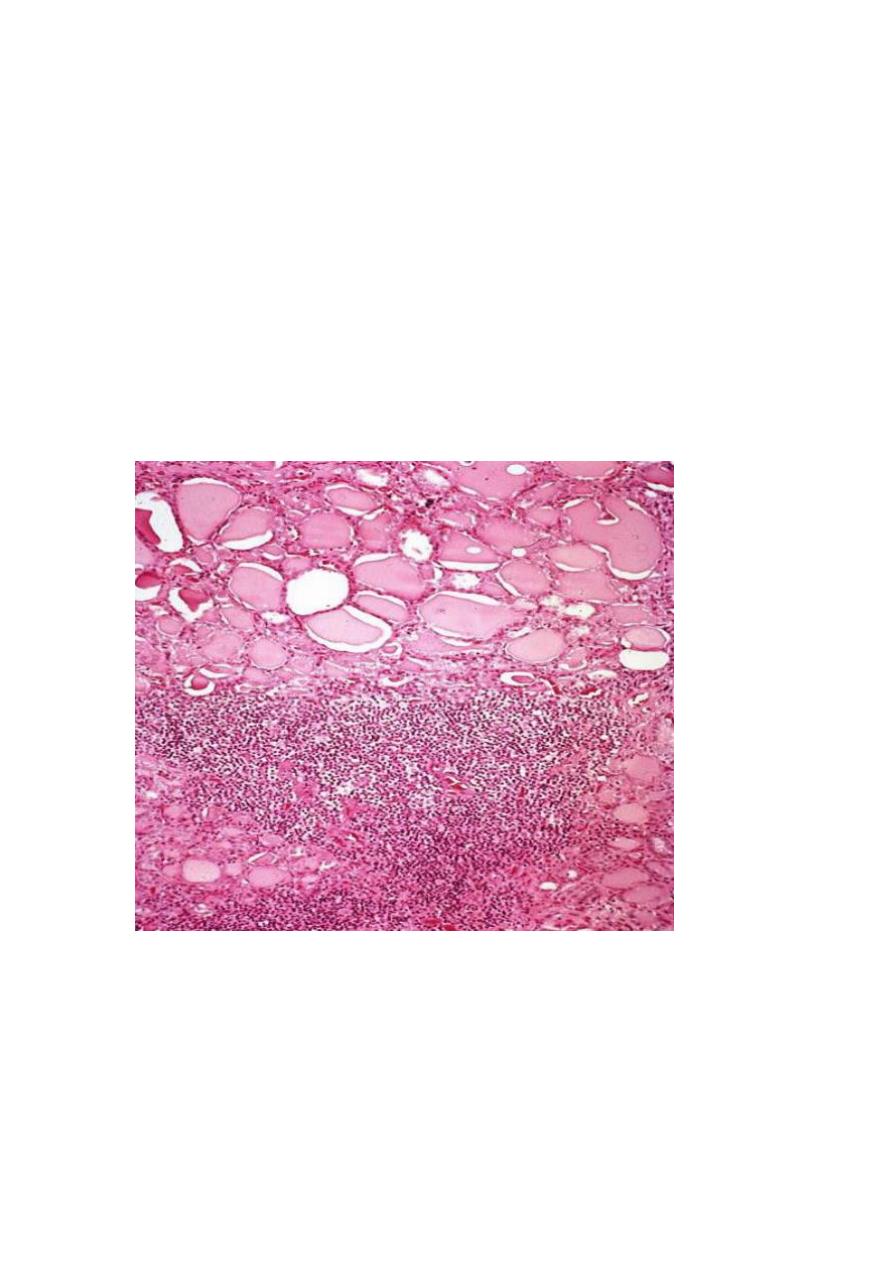
21
● These are largely non- diagnostic since similar alteration may be seen with other
tubulointerstitial disorders such as analgesic nephropathy.
● The parenchyma shows the following features.
-interstitial fibrosis with infiltration by lymphocytes, plasma cells, and sometimes neutrophils
-dilation or contraction of tubules with atrophic lining epithelium. Many of the dilated tubules
contain pink to blue colloid – like casts, the overall appearance is reminiscent of thyroid
tissue , hence the descriptive term thyroidization.
● Chronic inflammation with fibrosis involving the pelvi-calyceal mucosa and wall. This is
an important feature that is used in the differentiation from other conditions give
otherwise similar parenchymal changes.
● vascular changes of benign arterioseclerosis caused by the frequently associated HT.
although glomeruli may be normal some are sclerosed (glomerulosclerosis). Such changes
represent maladaptive changes secondary to nephron loss.
Absence of significant bacteriuria should not rule out CPN . if the disease is bilateral and
progressive , tubular dysfunction occur with loss of concentrating ability, manifested by
polyuria and necturia. Some persons with CPN or reflux nephropathy ultimately develop
glomerular lesion of global sclerosis and secondary FSGN. These are associated with
proteinuria and eventually contribute to progressive chronic renal failure.

22
Diseases of renal blood vessels :-
Changes affecting blood vessels are both frequent and important for the following
reasons:-
1. The renal vasculature is secondarily involved in almost diseases of the
kidney
2. Various form of systemic arteritis also involved blood vessels and such
involvement is secondarily important
3. The kidney is intimately involved in the pathogenesis of both essential and
secondary HT
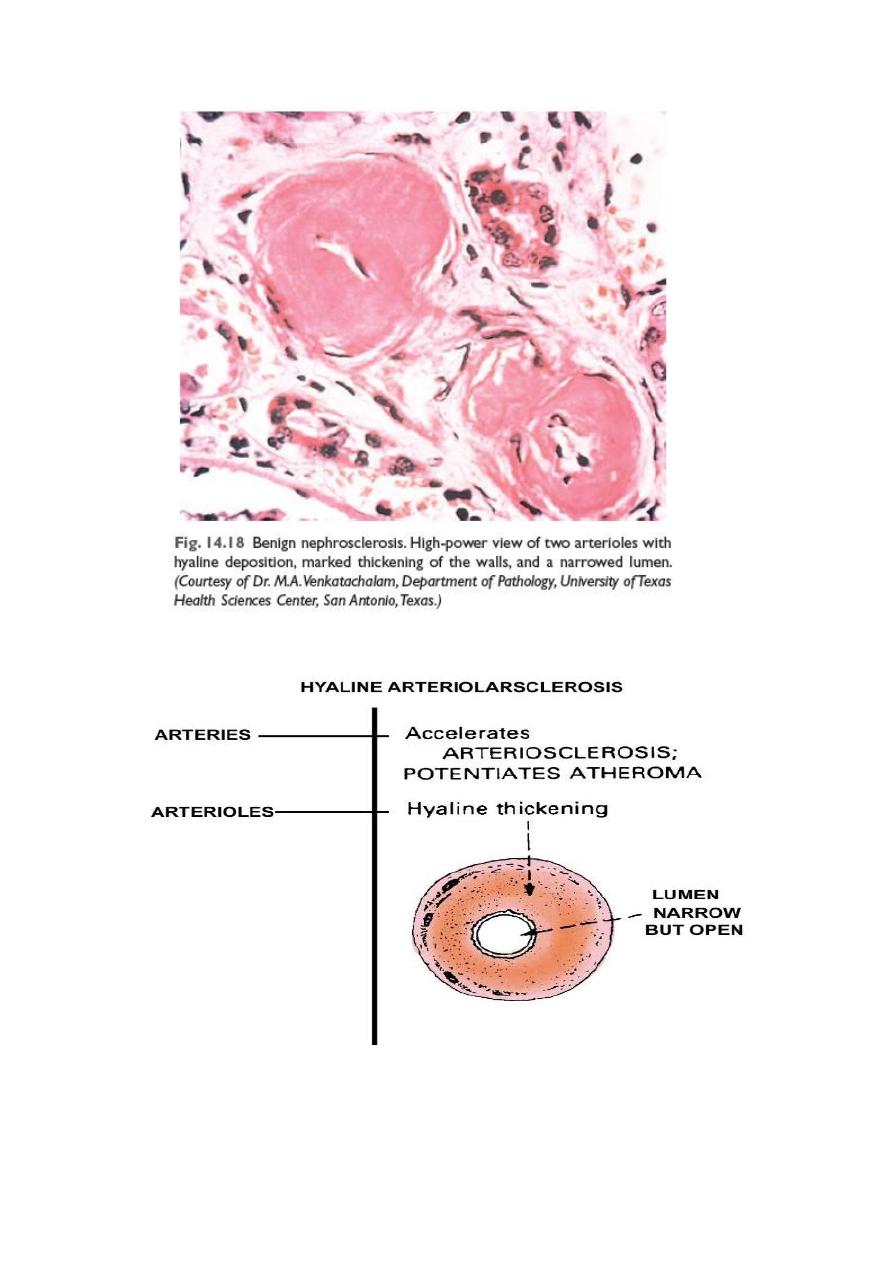
Benign nephrosclerosis (BNS):-
Some degree of BNS is present in many of those older than 60 years of age.
The frequency and severity of the lesion are increased at any age when HT &DM is present .
it is not clear whether BNS is a cause of HT or conversely, HT just accelerates an age related
vascular seclerosis.
Howevere many renal diseases cause HT which in turn associated with BNS . thus this renal
lesion is often seen superimposed on other primary kidney diseases
Gross features:-
The kidneys are symmetrically shrunken with diffuse fine granularity of the surface
Microscopic features :-
● The basic changes are hyaline thickening of the walls of the small arteries and arterioles
(hyaline arteriosclerosis). This appears as a homogenous pink hyaline thickening that
reduce the lumen
● The narrowing of the lumen result in markedly decreased blood flow through the
affected vessels and thus producing ischemic atrophy of all structures of the kidney.
● In advance cases the glomeruli become globally seclerosed . diffuse tubular atrophy and
interstitial fibrosis are often present.
● BNS rarely causes severe damage to the kidney . however all person with this lesion
usually show some functional impairment
23

24
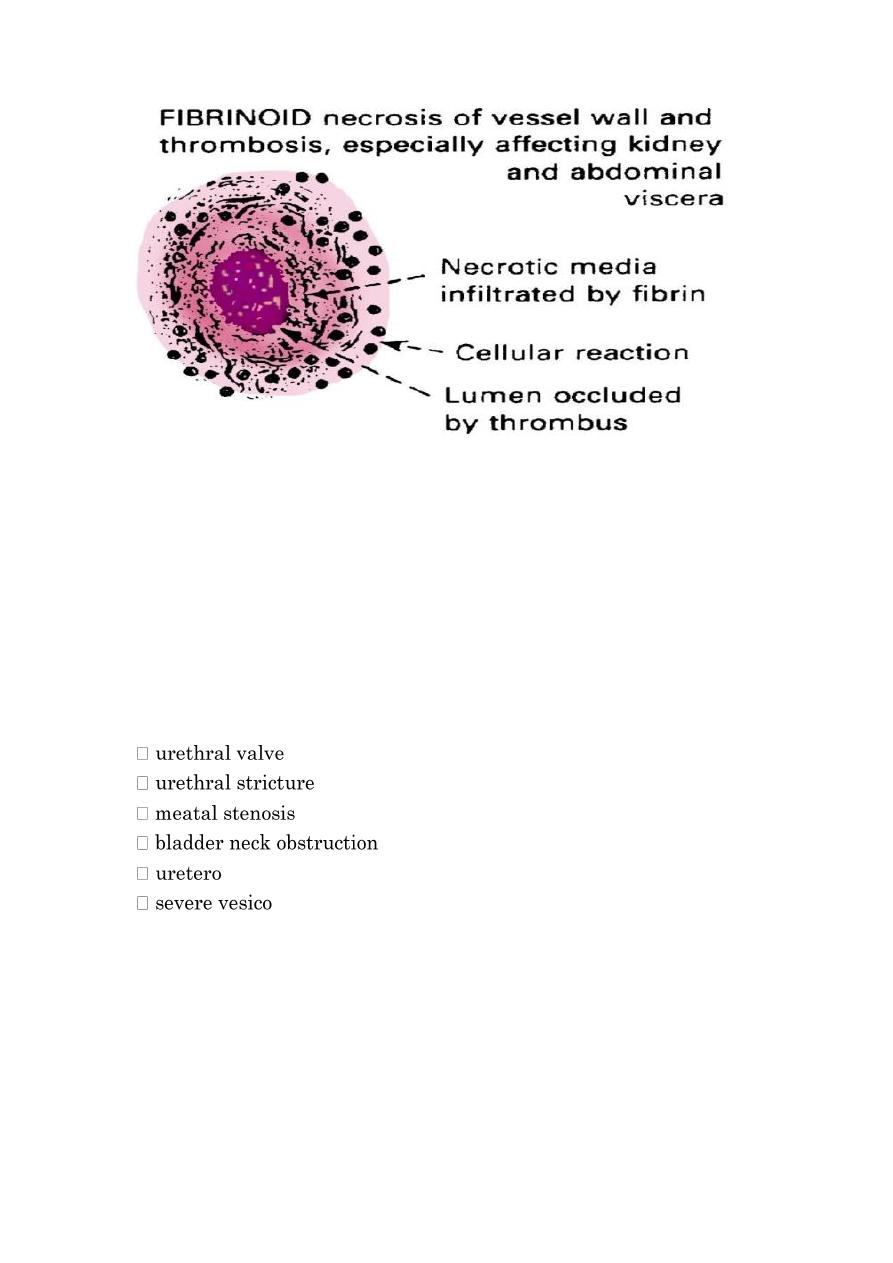
Malignant nephroseclerosis:-
Malignant HT occur in only about 5% of hypertensive pateints. It may occur de novo or
suddenly complicates mild HT
Pathogenesis
The following sequence of event is suggested
1. Initially there is renal arteriolar vascular damage mostly from long standing benign HT.
the result is increased permeability of the small vessels to fibrinogen and other plasma
proteins, endothelial cell injury and platelets deposition
2. This lead to occurrence of fibriniod necrosis of the arterioles and small arteries with
thrombosis
3. Platelet derived and other growth factors cause intimal smooth muscle hyperplasia
4. With severe involvement of the renal afferent arterioles , the renine stem is cycle is thus
created in which angiotensin II causes intrarenal vasoconstriction and the resultant
renal ischemia stimulates renini secretion.
5. Aldosterone levels are elevated the salt retention contributes to the elevation of the
blood pressure
The consequences of markedly elevated blood pressure on the blood vessels throughout
the body are known as malignant arteriosclerosis and the renal disorder is referred to as
malignant nephroseclerosis.
Gross feature:
The kidney which may be normal in size or slightly shrunken display small pinpoint petechial
hemorrahges on the cortical surface due to rupture of arterioles or glomerular capillaries.
These give the kidney a pecular flea –bitten appareance
Microscopic:-
● There is fibrinoid necrosis of the arterioles. The vessel walls show homognous
granular eosinophilic appareance.
● In the small arteries and large arterioles, proliferation of the intemal smooth muscle
cells produce hyperplastic arterioloselerosis in which the intimal smoothe cells show
concentric arrangement (onion skin appearance). This lesion cause marked
narrowing of the arterioles and small arteries to the point of total obliteration
● Necrosis may also involve glomeruli, with microthrombi within the glomeruli and
necrotic arterioles.
25
The full-developed syndrome of malignant HT is characterized by diastolic pressures greater
than 120 mmHg, papilledema, encephalopathy cardiovascular abnormalities and renal failure at
the onset of rapidly rising blood pressure there is marked proteinutia and microscopic or
sometimes macroscopic hematuria followed soon by renal failure. The syndrome is a true
medical emergency. About 50%of patients survive at least 5 years. Ninety percent of deaths
are caused by uremia and the other 10% by cerebral hemorrhage or cardiac failure
Urinary Tract Obstruction "Obstructive Uropathy"
Causes
✓ Congenital abnormalities or anomalies:
-pelvic Junction Obstruction
-ureteral reflux
✓ urinary stone
✓ Benign prostatic hypertrophy
✓ Tumors (Ca. prostate, bladder, cervix, ureter, Renal pelvis,
retroperitoneum).
✓ Inflammation: prostatitis, ureteritis, urethritis, retroperitoneal fibrosis,
endometriosis.
✓ Sloughed necrotic papillae, blood clots.
✓ Pregnancy, uterine prolapsed.
26
✓ Neurogenic bladder (spinal cord damage).
Obstruction either
sudden or insidious onset
complete or intermittent & partial
Unilateral or Bilateral
Obstruction increases the susceptibility to infection UTI and stone formation,
if not relieved → permanent renal atrophy.
Complication
1. Infection.
2. Stone formation.
3. Hydronephrosis.
Effects of urinary obstruction
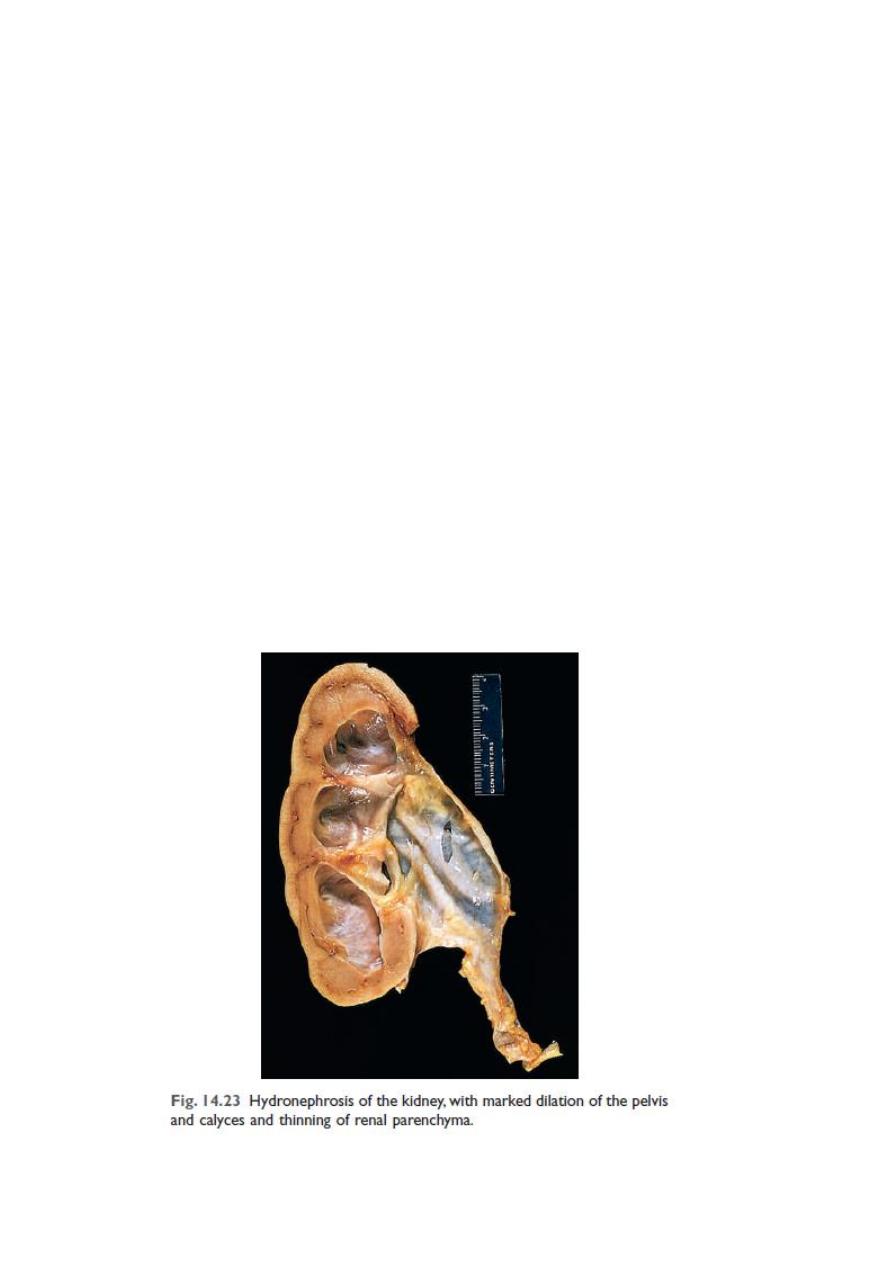
Hydronephrosis
☒ Dilatation of the renal pelvis and calyces with progressive atrophy of the
kidney due to chronic incomplete (Partial) obstruction to urine outflow.
☒ With more progressive dilatation → more atrophy of renal parenchyma and
kidney become as cystic structure

27
☒ Effects:
1. infection
2. stone formation
3. Renal Failure (Bilateral)
Renal Stones (calculi, Urolithiasis)
❖ Can occur at any level of urinary tract, but mainly occur in the kidney.
❖ Male > Female.
❖ Types: according to the constituents of stones, can be classified into:
1. Calcium stones. 80%
2. Triple phosphate stone. 10 – 15%
3. Uric acid stone. 6%
4. Cystine stone. 1 – 2%
Calcium stones
✓ Composed of

28
Hypercalciuria, hypercalcemia & Hyperoxaluria
✓ The stone are radio opaque.
✓ Formed in acidic urine
Triple phosphate (Struvite) stone
Composed of magnesium, ammonium & phosphate.
Formed in alkaline urine by urea splitting bacteria
stag-horn stones (infection)
Radio opaque.
Uric acid stone
☒ Common in pt. with hyperuricemia, such as gout-
☒ Radiolucent.
☒ Formed in acidic urine
Cystine stones
occur due to genetically defect in the renal transport of amino acid like
cystine.
Predisposing factors
1. Decreased urine volume (dehydration).
2. Increased of stone constituents
3. Obstruction + Stasis of urine,
e,g, Prolong immobilization.
4. Infections.
5. change in urine PH.
6. Diet. Vitamin A deficiency.
7. Idiopathic
8. Lack of inhibiter of crystal
formation & urinary mucoprotein
Effects and complications
1. Passage of small stone → down the ureter to bladder → severe renal colic
with injury to ureter → hematuria & /or inflammation → stricture with
subsequent impaction.
2. Passage of large stone → impaction at upper or lower end of ureter or
pelvic brim → stasis causing hydroureter, hydronephrosis & infection + stasis
with further stone formation – stag horn stones

29
3. Pelvic suppuration and ulceration.
4. Squamous metaplasia of pelvis Transitional epith. with risk of
development of Sq. cell Ca.
Urinary bladder stones
❖ Either single or multiple
❖ most cases arise in renal pelvis and pass down to bladder where grow to
larger size sometime very large size
❖ it cause cystitis, hematuria, obstruction, ulceration of mucosa, Squamous
metaplasia & risk of Sq. cell . Ca.
Tumors of the Kidneys
Benign Tumors
Adenoma
✓ Small yellowish cortical tumor
✓ less than 5 mm Ø.
Angiomyolipomas
Hamartoma composed of mixture of blood vessels, smooth muscle, and fat,
common in patient with Tuberous sclerosis.
Oncocytoma
Epithelial tumour composed (oncocytic cells), may reach large size 12 cm Ø.
Renal hemangioma
Hematuria.
Renal fibroma
☒ Small round whitish nodule of fibrous tissue
☒ Seen in medulla
Malignant Tumors
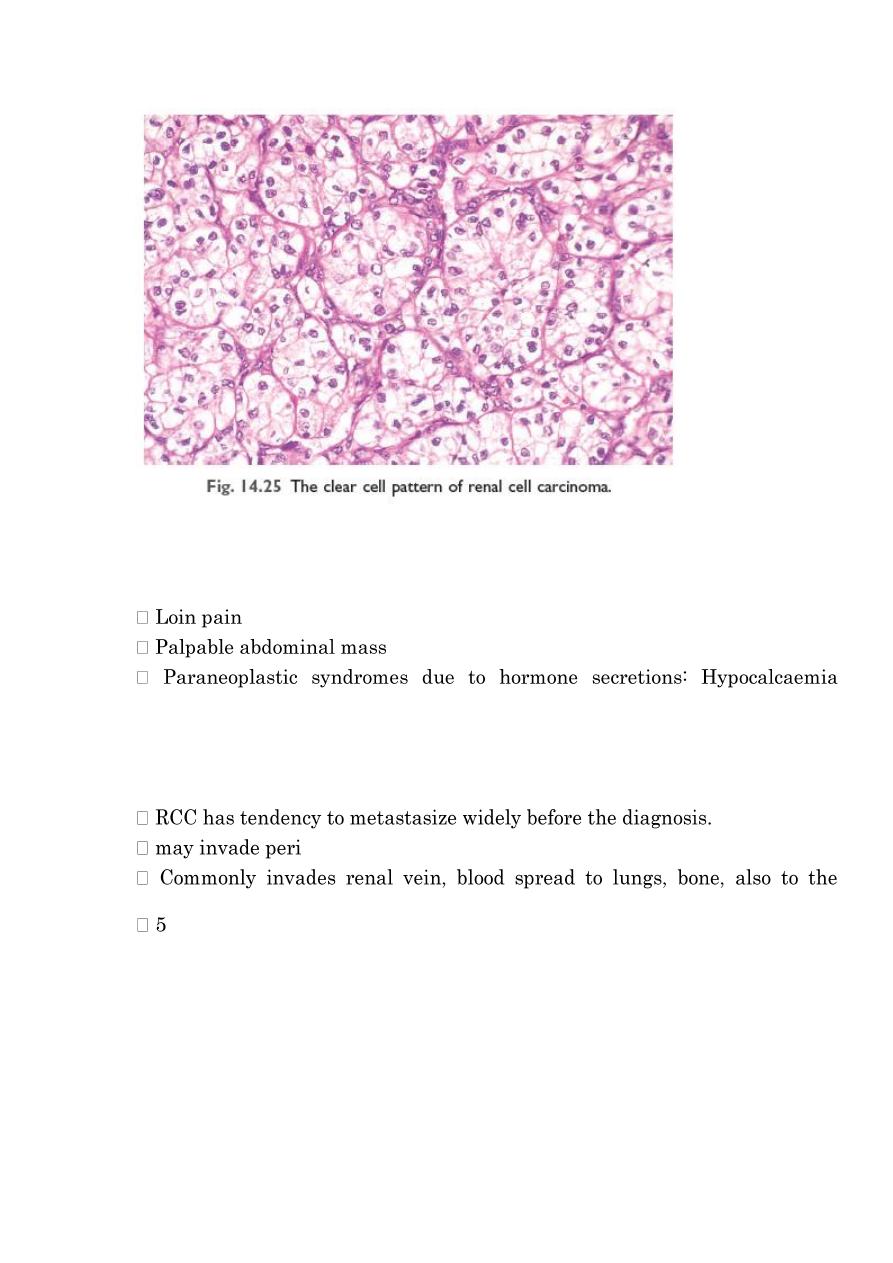
Renal cell carcinoma, Hypernephroma , Adenocarcinoma
Clear cell carcinoma
The commonest primary malignant renal tumor in adult
❖ 90% of all renal cancers (tubular epithelial cell)
❖ 1-3% of visceral cancers.
❖ Most common in 50-70 years of age
❖ Male predominance
❖ Most cases sporadic, very few familial cases.
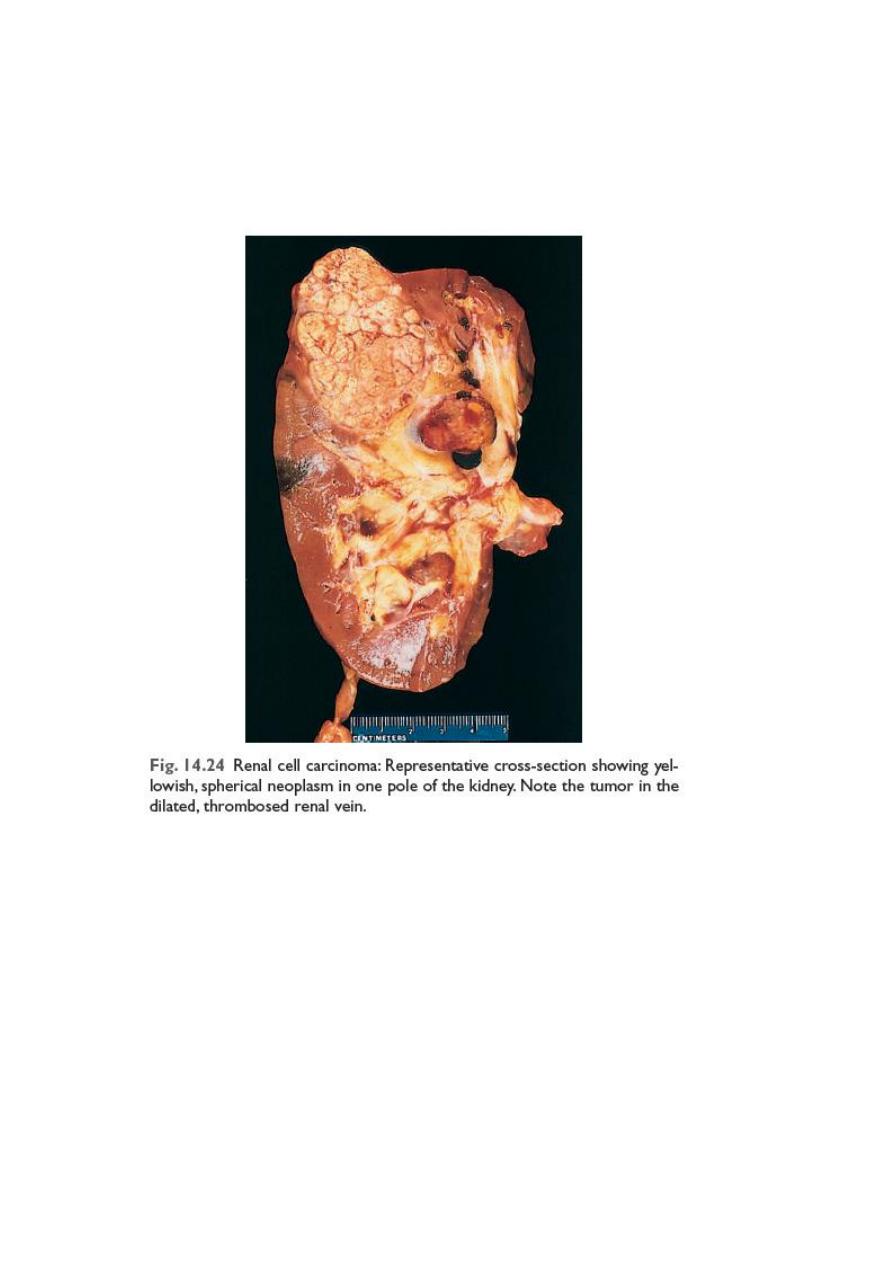
30
❖ 40% of patient with von- Hippel-lindaue disease (retinal hemangioma with
cerebellar hemangioblastoma) develop RCC, usually bilateral (AD disease)
Grossly: rounded mass 3-15 cm or more, partially encapsulated, yellowish-
orange in color, with areas of hemorrhage, necrosis and cyst formation.
❖ Histology: tumor composed of large clear cells (Clear Cell Carcinoma) rich
in glycogen and lipid, arranged in solid masses, tubules, acini, and papillae,
some tumor composed of granular cells
31
clinically
Hematuria
(PTH), Polycythemia (erythropoietin), H.T (renin), Cushing syndrome
(glucocorticoid), Amyloidosis.Secondaries (pathological fracture) Bone
Prognosis
depend on Tumour size, Grade and Stage (extent of spread).
-renal fat, adrenal glands and others.
lymph nodes by lymphatic.
- year survival is 45%, and up to 70% in absence of metastasize.
Wilm's Tumour (Nephroblastoma)
✓ commonest malignant renal tumour in infant and childhood
✓ 25% of all cancer in children
✓ Most occurs between 2-5 years
✓ Usually unilateral as palpable Abdominal Mass
✓ Most cases are sporadic
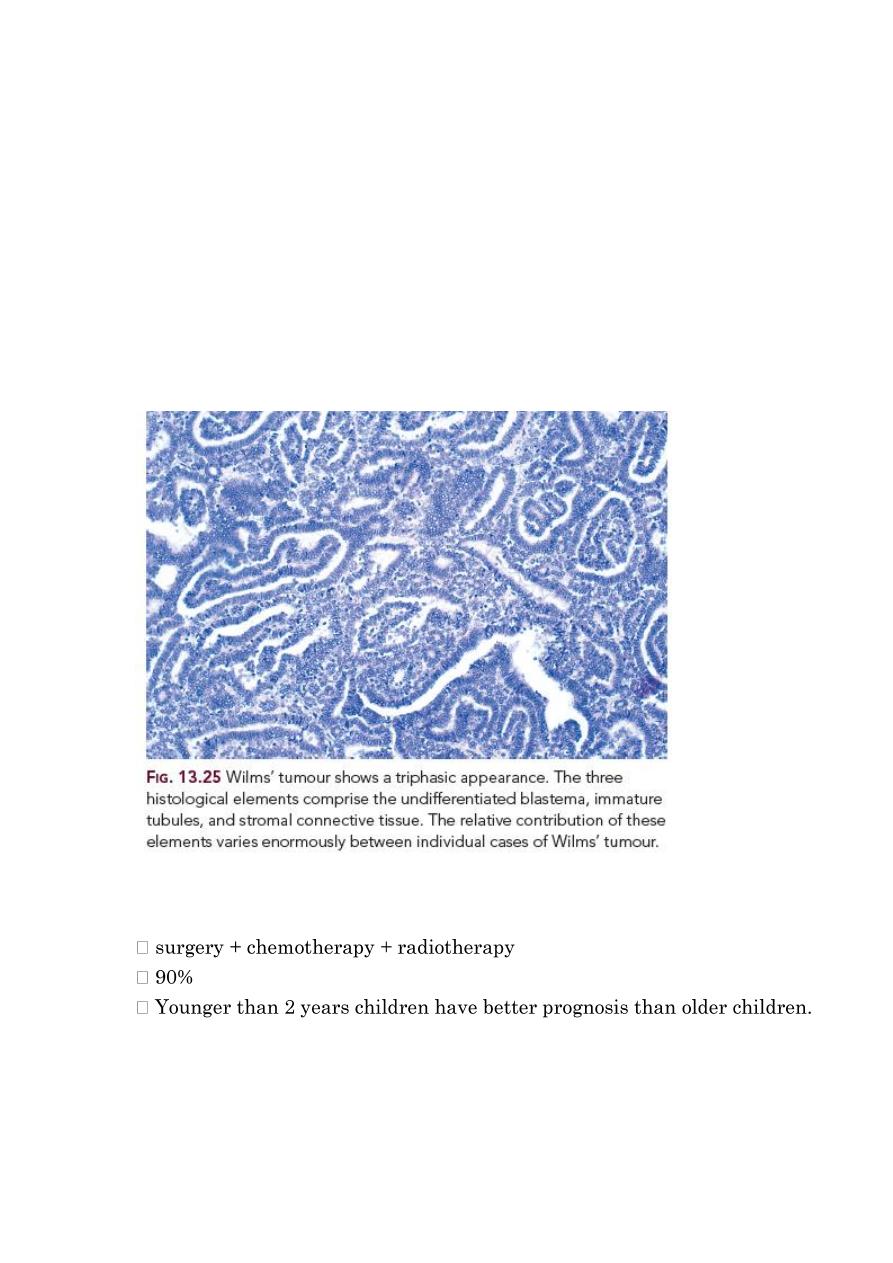
32
✓ few cases 5-10% familial associated with other developmental
malformation syndrome have deletion in chromosome 11p
✓ (aniridia, genitourinary anomalies, mental retardation), hemihypertrophy.
& It is embryonic tumor derived from renal blastema
✓ Gross: large soft well – circumscribed whitish renal mass rapidly invades
blood vessels and give pulmonary metastasis.
Triphasic histological features
1. Blastema cells – small round cells.
2. Epithelial cells – forming primitive tubules and primitive glomeruli.
3. Stromal spindle cells
Prognosis
improved recently by combination of
-95% - survival or cure.
Transitional cell carcinoma of Renal Pelvis
✓ 5-10% of renal tumour
✓ Early diagnosed because of obstruction, hematuria, or renal colics
✓ Similar to urothelial tumour of bladder, most are papillary

33
Prognosis
● Good for papillary superficial-low grade tumor
● 70% -- 5 yrs survival
● Poor for Invasive (infiltrating )--high grade tumour
● 10% --5 yrs survival
✓ Secondary tumor
are not uncommon in kidney
Diseases of the urinary Tract
1. Obstruction
2. Infections
3. Stone formation
4. Tumors
Ureter
Obstructive lesions most important causing hydroureter and hydronephrosis
Intrinsic Factors
Stone < 5mm Ø causing renal colic, larger not enter
Stricture either congenital or acquired (inflammation)
Tumour – TCC
Blood clots: massive hematuria from stone, tumours, papillary necrosis.
Neurogenic bladder
Extrinsic Factors
Periureteral inflammation: e.g.: salpingitis, peritonitis, diverticulitis,
retroperitoneal fibrosis & endometriosis.
Tumour: e.g. rectum, bladder, prostate, ovaries, uterus, cervix, lymphoma,
sarcoma
ureteral obstruction is one cause of death in cervical carcinoma.
Urinary bladder
Congenital anomalies
Diverticula

34
☒ Congenital defect or more commonly acquired from persistent urethral
obstruction
☒ Predispose to infection, stone formation, vesicoureteral reflux & rarely
carcinoma.
Bladder Extrophy
❖ Incomplete closure of anterior abdominal & bladder walls, as exposed sac
❖ Predispose to infection and adenocarcinoma
Inflammation
Acute and Chronic Cystitis
✓ Very common, causing frequency, dysuria, lower abdominal pain & fever
✓ chronic cystitis is the result of repeated attacks of acute cystitis-
✓ common in female especially during pregnancy.-
✓ common in elderly male it associated with obstruction of the urethra
caused by BPH or urethral stricture.
Causative agents:
● Bacteria e.g. E- coli, proteus, klebsiella
● viruses e.g. cytomegalovirus, adenovirus
● Fungi e.g. Candida (in immunosuppressed patients, “AIDS, cancer
patient, DM, and receiving long-term Antibiotic”) Chlamydia &
Mycoplasma.
Tuberculous cystitis
Occurs secondary to TB of kidney & epididymis.
Radiation cystitis
hemorrhagic cystitis due to chemotherapy such as cyclophosphamide.
Bilhariziasis is common in Egypt, produce chronic granulomatous cystitis &
predispose to carcinoma.
Special forms of cystitis
Interstitial cystitis (Hunner ulcer)
☒ Chronic cystitis of unknown etiology
☒ Commonly seen women
☒ Associated with severe pain not respond to treatment.
Malakoplakia: (soft Yellowish plaques)
☒ Chronic bacterial cystitis (E. coli & Proteus)
☒ characterized by soft- yellowish plaques covering bladder mucosa
☒ It may occurs in other organs such as colon, lung, bones, kidney & prostate.
35
Metaplasia
Two types occur in bladder mucosa
1. Glandular (intestinal) metaplasia
Occurs in chronic inflammation, characterized by formation of cystic glands
lined by columnar cells called cystitis cystica and cystitis glandularis, when
extensive, carry risk of adenocarcinoma.
2. Squamous metaplasia
Result from chronic inflammation, stone, bilhariziasis, extrophy
predisposes to Squamous cell Carcinoma of the bladder.
Bladder Tumors
most bladder tumours 95% arise from transitional epithelium (Urothelium)
“Transitional cell tumors“
Are very common.
Benign Tumours
Papilloma
❖ is very rare, composed of finger - like papillae
❖ May recur, local excision
❖ some regard all transitional cell tumors are malignant, no papilloma =
grade- I TCC
❖ But other are not believed this.
Inverted papilloma
Downward growth of papillae with smooth surface, from benign nodule.
Bladder Carcinomas
✓ Are common.
✓ 5% squamous cell carcinoma
✓ 1-2% adeno carcinoma
✓ 3-4% mixed carcinoma.
✓ 90% are transitional cell carcinoma
✓ Predisposing factors
1. Smoking.
2. Infection: Bilharziasis.
3. Analgesic abuse.
4. Chemotherapy
5. Chemical substances: Naphthylamine.
36
Transitional cell carcinoma TCC
Commonest Ca. of bladder
Trigone common site
Also occurs in ureter and renal pelvis.
More in male, M/F: 3:1
Between 50-80 years.
Grading of TCC is important for prognosis
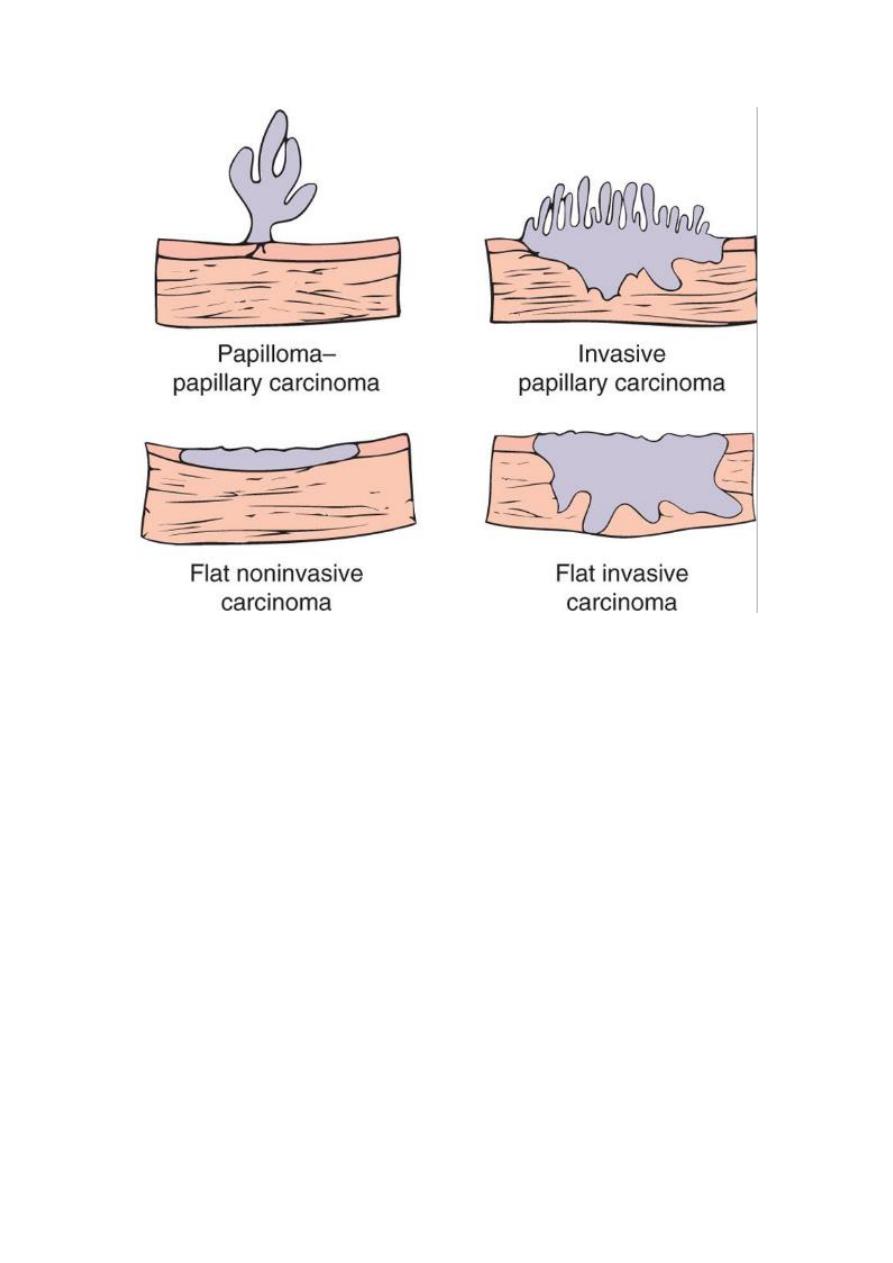
Low-Grade Papillary TTC (I – II)
☒ Papillary, Well-Differentiated Tumor
☒ Usually Superficial- Non Invasive Tumor.
☒ Good prognosis
☒ Local Recurrence is common.
High-grade TTC (III-IV)
❖ Most aggressive Sessile (Non-Papillary) Tumors
❖ Less-Differentiated Tumors
❖ Invasion of muscle layers and lymphatic in the bladder wall are
widespread and extensive
❖ Very poor prognosis
❖ Clinically – Painless hematuria
Frequency and Dysuria
❖ Prognosis depend on
❖ 5-Yr survival is 95% for Low- Grade, 35% for High- Grade
Four morphologic patterns of bladder tumor:
37
Squamous cell carcinoma
✓ Arise in areas of squamous metaplasia due to chronic inflammation and
irritation as in stone and Billariziasis
✓ Usually poorly – differentiated
✓ Prognosis is very poor, Regardless of the tumour grade.
✓ Death occurs in the first year of the diagnosis.
Adenocarcinoma
Uncommon 1-2 % of all cancer
Arise in the background of
✓ chronic inflammation with cystitis cystica and cystitis – glandularis
(glandular metaplasia)
✓ Bladder Extrophy
✓ Urachal remnant at the dome.
