1
L3
Bacterial skin infections
D. Hadf
Objectives
After completing this lecture, the student should be able to:
Describe the morphology of common cutaneous bacterial infections.
Discuss the bacterial etiologies of cellulitis and erysipelas.
Become familiar with superinfection of resident normal flora
Recommend initial steps for the evaluation and treatment of common cutaneous
bacterial infections.
Natural defense of skin
1- Temperature more than 37cº
2- Dryness
3- Keratin & normal desquamation
4- Sebum with its low PH & high lipid content
5- Sweat with its low PH & high salt content
6- Skin associated lymphoid tissue
7- Resident microflora (mainly gram positive)
Resident microflora
• Millions of micro organisms, reside harmlessly on skin
• The total microbial cell count in and on our bodies is 10 times greater than the number
of human cells.
• After the gut, there are more microorganisms on the skin than anywhere else in the
body
• Bacterial species are the most numerous.
• Fungi, viruses and mites are also found on the normal skin
• Resident flora are found in the upper parts of the epidermis and congregated in and around
the hair follicles. They include:
• Bacteria:
Staphylococci,
Micrococci,
Diphtheroids:
Corynebacterium,
&
Brevibacterium
• Fungi: Candida albicans, Malasezzia & many other species
Staph.epidermidis+aerobic diphtheroids predominate on the surface.
Anaerobic diphtheroids deep in hair follicles
Transient bacteria
• S. aureus does not normally reside on the skin, but may be present transiently, inoculated
from colonized sites such as the nares(30%), axillae & vagina
2
• This colonization is usually transient except in 10-20% where it becomes persistent, these
are called staph carriers & are a hazard to the society.
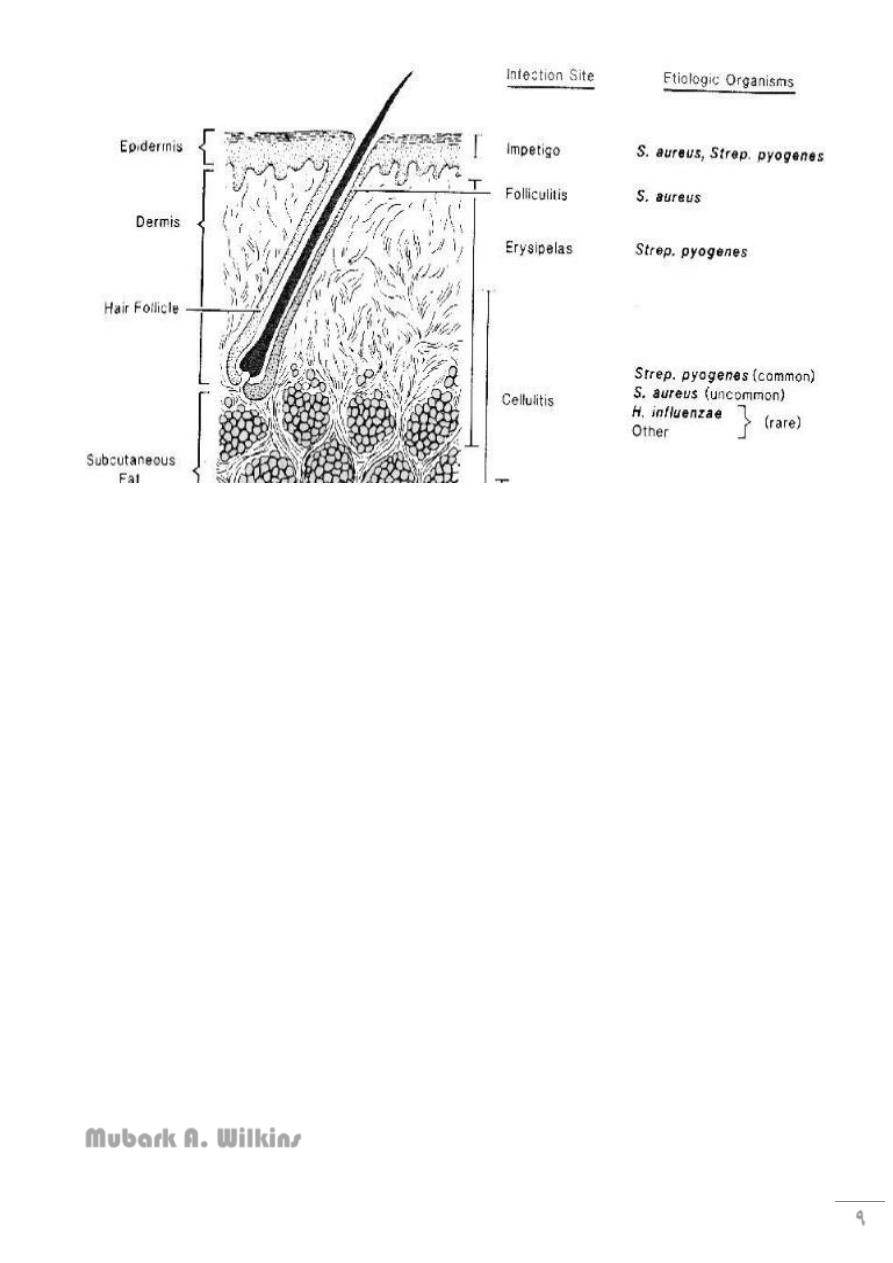
Primary bacterial infections
• Impetigo & ecthyma
• Folliculitis
• Furuncles & Carbuncles
• Erysipelas
• Cellulitis
Secondary bacterial infection
Infection of previously damaged or diseased skin, such as
• Dermatitis
• Herpes simplex
• Burn
• Scabies & pediculosis
Any child presenting with recurrent impetigo of the scalp we should look for underlying
pediculosis capitis.
Impetigo
• Acute, contagious bacterial infection of the skin
• Of 2 types:
• Bullous: caused by S. aureus
• Non-bullous: mainly by group A ℬ heamolytic streptococci
• Peak incidence aged 2-5 years, but can affect older children & adults
• M=F
• Can be primary or secondary
3
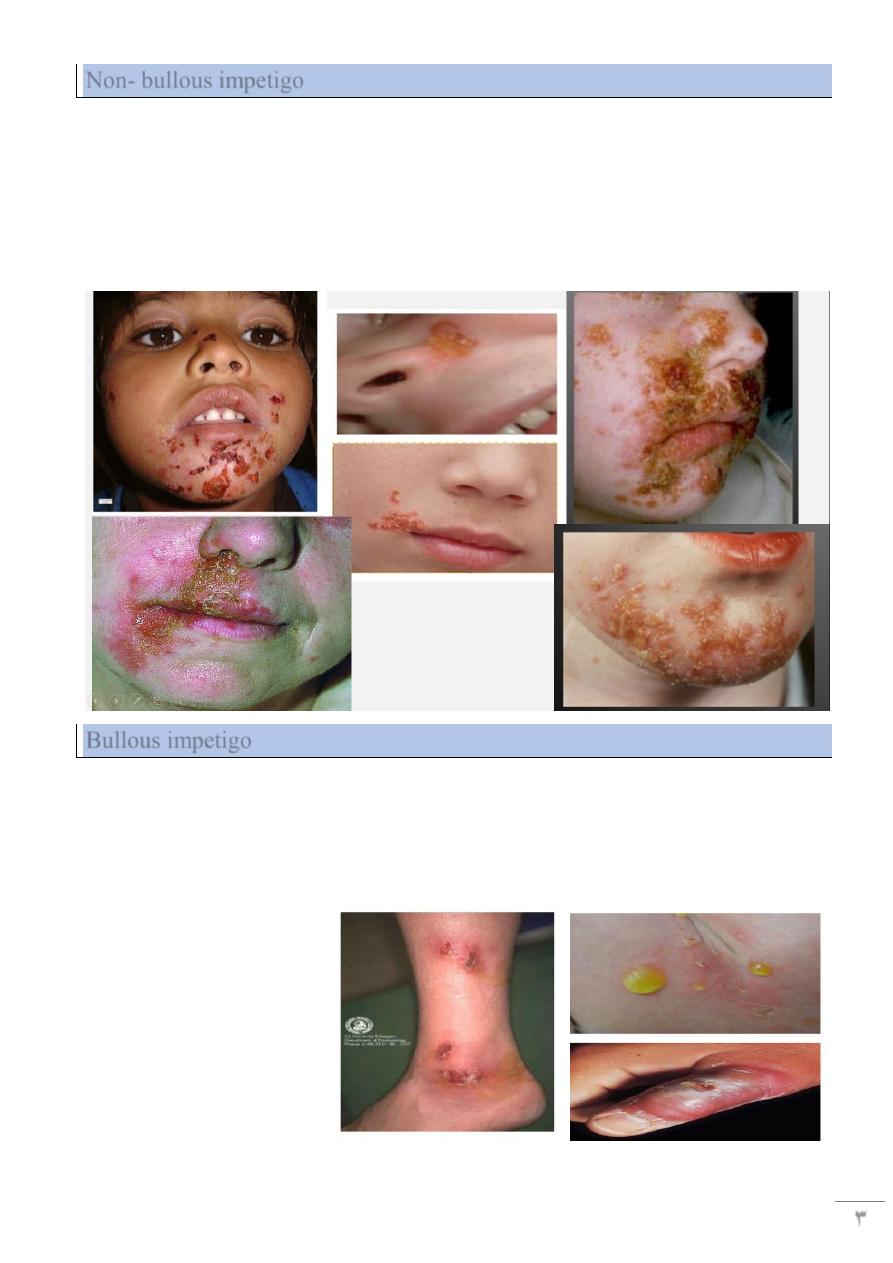
Non- bullous impetigo
• Caused by strept., staph., or usually a mixture of 2
• A thin walled vesicle on erythematous base, soon ruptures & a crust forms (yellowish
brown= honey colored)
• Heals without scarring
• Regional adenitis & fever in severe cases
• Can affect any part, except palms & soles
• Mostly exposed parts, especially central face
Bullous impetigo
• Mostly caused by s. aureus
• Mostly in newborn
• Target area is the face, but can occur anywhere even palm & soles
• Bullae are larger, persist longer(2-3 days), contents are first clear then become turbid,
then rupture forming thin varnish-like brownish crusts
4
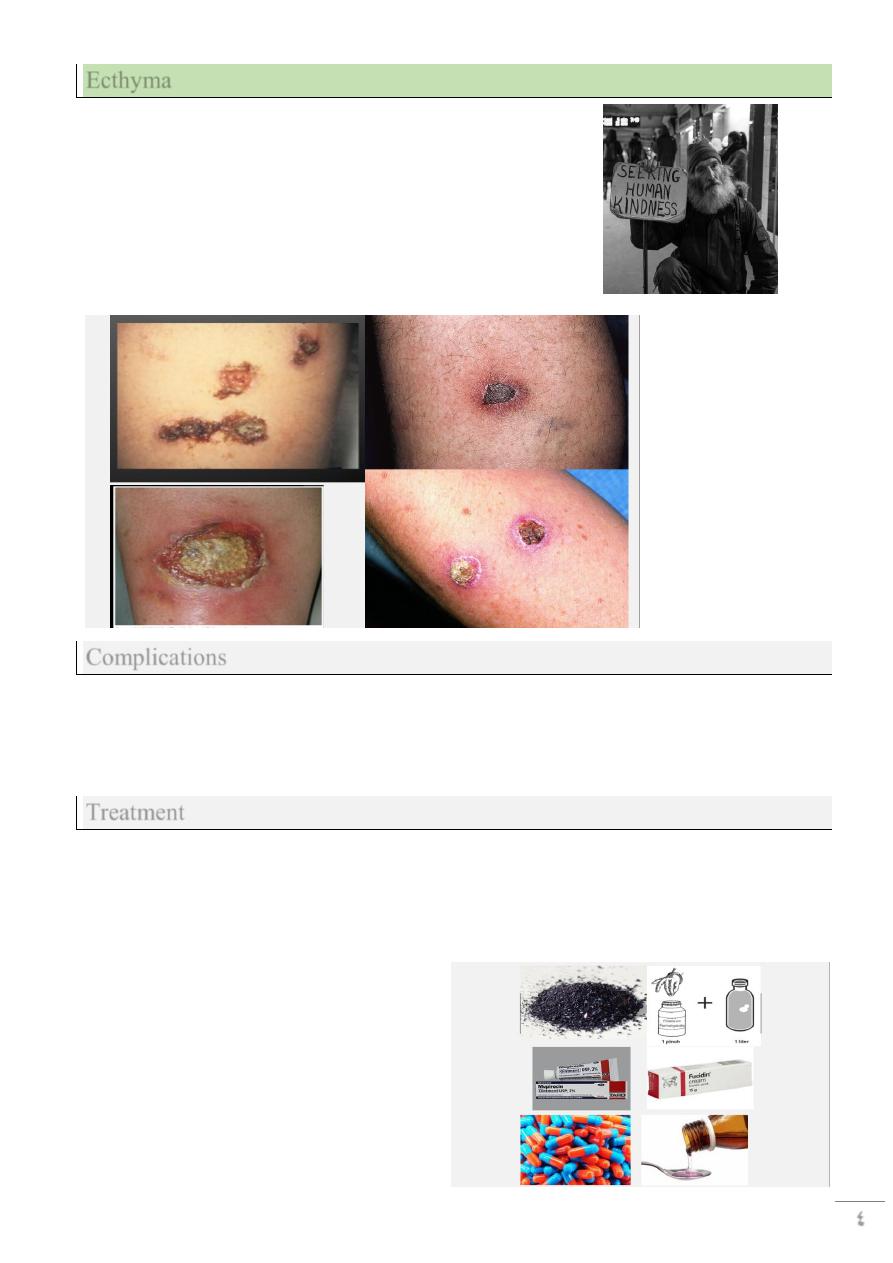
Ecthyma
• A lesion of neglect, develops at site of old
trauma
• Mostly elderly, diabetic, debilitated, or alcoholic
patients (= vagabond’s disease)
• Caused by strpt. pyogenes, & staph.
• Mostly on lower limbs
• Adherent crust, beneath which is a purulent
irregular ulcer, delayed healing with scarring.
Complications
• lymphangitis, lymphadenitis.
• Staphylococcal scalded skin syndrome (SSSS).
• Post streptococcal acute glomerulonephritis, especially in cases due to streptococcus
pyogenes M type 49
Treatment
• Wet compresses with antiseptic solution to remove crusts with topical antibiotics is
enough in mild cases.
If severe or a nephritogenic strain of strept is suspected; then a systemic antibiotic is added as
flucloxacillin , erythromycin or cephalexin.

5
Staphylococcal infections:
1- Superficial folliculitis:
• Inflammatory disease of the hair follicles, which may be infectious or non infectious
• The infection is superficial involving the ostium of the hair follicle
• Usually caused by staph aureus
• Common on scalp of children, beard, axillae, extremities, buttocks
• Heal spontaneously in 1 week, or become chronic
• In adults can progress to boils
Folliculitis
Can be:
1- infective: bacteria & yeast (pityrosporum)
2- Chemical: by mineral oils
3- physical: as after hair epilation
2- Deep folliculitis(=furuncles= boils)
• Staphylococcal infection of the hair follicles, similar to but deeper than folliculitis
• Start as firm, red, tender papule that becomes painful &fluctuant nodule, finally
ruptures & discharges pus, leaving a scar
• Sites of friction & sweating; mostly neck, buttocks & ano-genital area due to staph.
carriage at these areas
• Constitutional symptoms may be present
• Some have recurrent attacks (=chronic furunculosis)
Chronic furunculosis
• They may recur at intervals for no apparent cause, these patients are staph carriers
(they carry s. aureus in their nostrils, axillae & groins)
• They may be treated by topical antibiotics applied to carrier sites
• Long courses of oral flucloxacillin
• Care about hygiene & predisposing factors
6
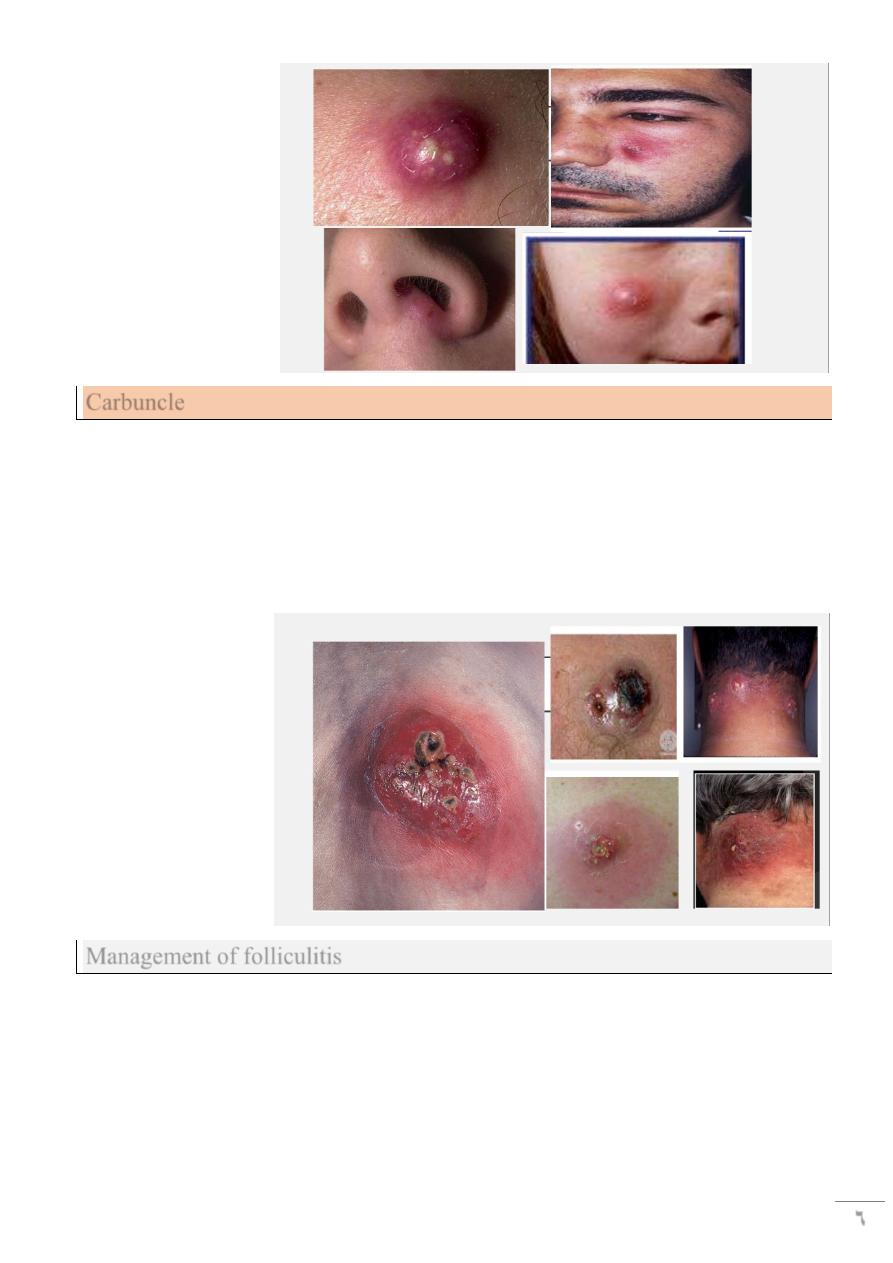
Carbuncle
• Collection of boils
• Swollen suppurating painful areas discharging pus from several points
• In areas of thick inelastic skin the infection spreads to subcutaneous fat such as nape
of neck, back & thighs
• More painful & severe with constitutional symptoms
• More in diabetics
• Blood stream invasion may occur
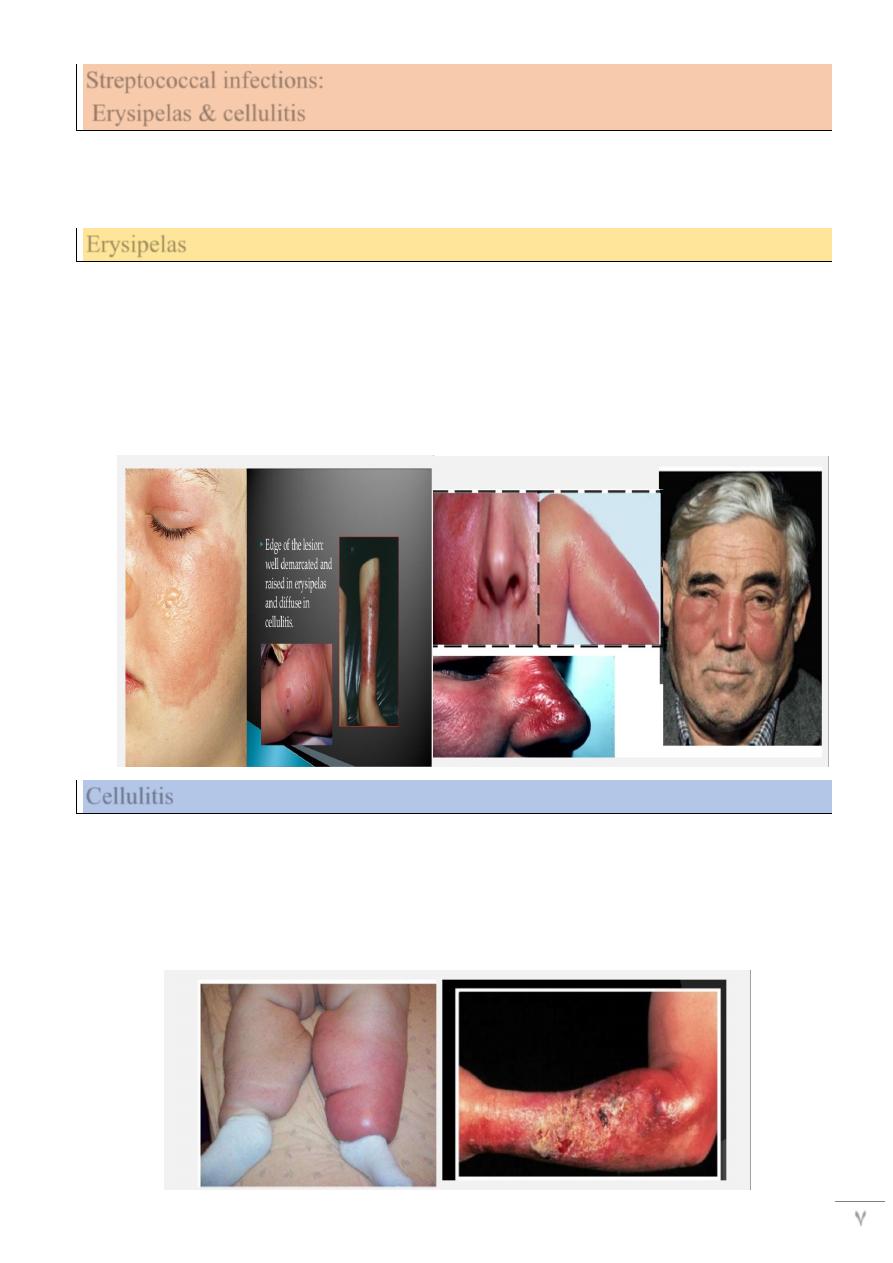
Management of folliculitis
• Correction of underlying causes: diabetes, anemia, poor hygiene.
• Swabs for culture from lesions & carrier sites.
• Topical & systemic antibiotics.
• Incision of boils & carbuncle to speed healing.
• Recurrent boils need treatment of carrier states by b.d. topical antibiotics for 6 weeks+
improve patient’s hygiene.
7
Streptococcal infections:
Erysipelas & cellulitis
• Cellulitis: infection of the subcutaneous tissue
• Erysipelas: infection of the dermis & upper part of subcutaneous tissue
• by group A ℬ heamolytic strept.
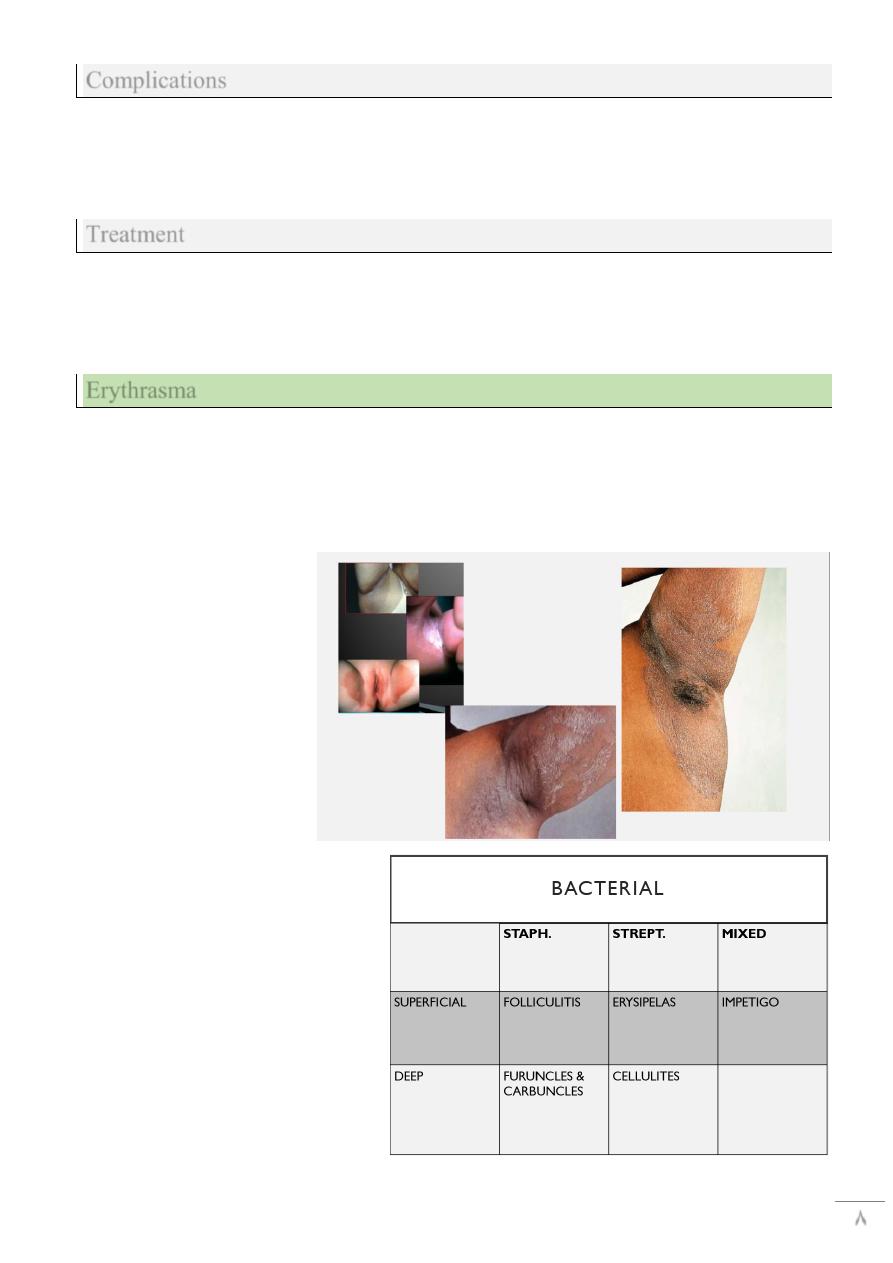
Erysipelas
• Minor cracks or wounds in the skin are the port of entry
• Starts with severe constitutional symptoms
• Followed by appearance of rapidly spreading painful erythematous plaque with well
defined margins.
• May show hemorrhage or blistering
• 80% occur on the face
• Can be fatal if untreated
Cellulitis
Similar to erysipelas, with some differences
1- deeper level of skin involvement (subcutaneous tissue)
2- Other organisms than strept. can cause it, like s. aureus
3- more raised & swollen but less well-defined border
4- More on the lower limbs than the face
8
Complications
1- recurrences may lead to lymphedema
2- subcutaneous abscess
3- Septicemia
4- nephritis
Treatment
• Rest, analgesia
• Systemic antibiotics especially penincillin
• E.g: benzyl penicillin 600-1200 mg IV/6 hourly
• Or cephalosporin
Erythrasma
• Caused by corynebacterium minutissimum a member of resident flora
• Asymptomatic, well demarcated, scaly, reddish brown
• Body folds: axilla, groins, toe webs
• Coral red fluorescence with Wood’s lamp
• Treated by topical antifungal, antibiotics, or sometimes systemic erythromycin
9
Mubark A. Wilkins



