Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
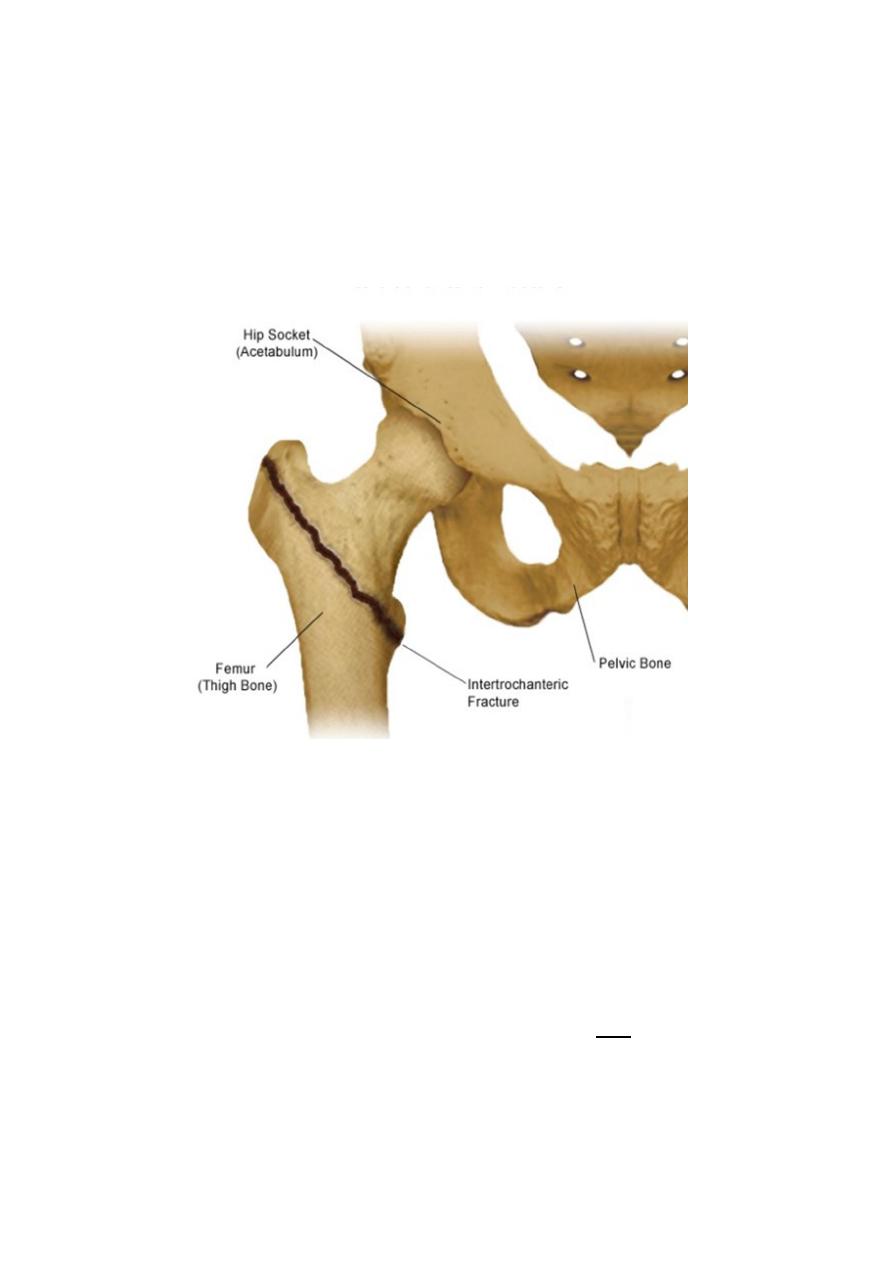
INTERTROCHANTERIC FRACTURES
Intertrochanteric fractures are, by definition, extracapsular.
They are common in elderly, osteoporotic people; most of the patients are women in the
8th decade. However, in contrast to intracapsular fractures, extracapsular trochanteric
unite quite easily and seldom cause avascular necrosis.
Mechanism of injury
The fracture is caused either by a fall directly onto the greater trochanter or by an indirect
twisting injury.
The crack runs up between the lesser and greater trochanter and the proximal fragment
tends to displace in varus.
Pathological anatomy
& classification : -
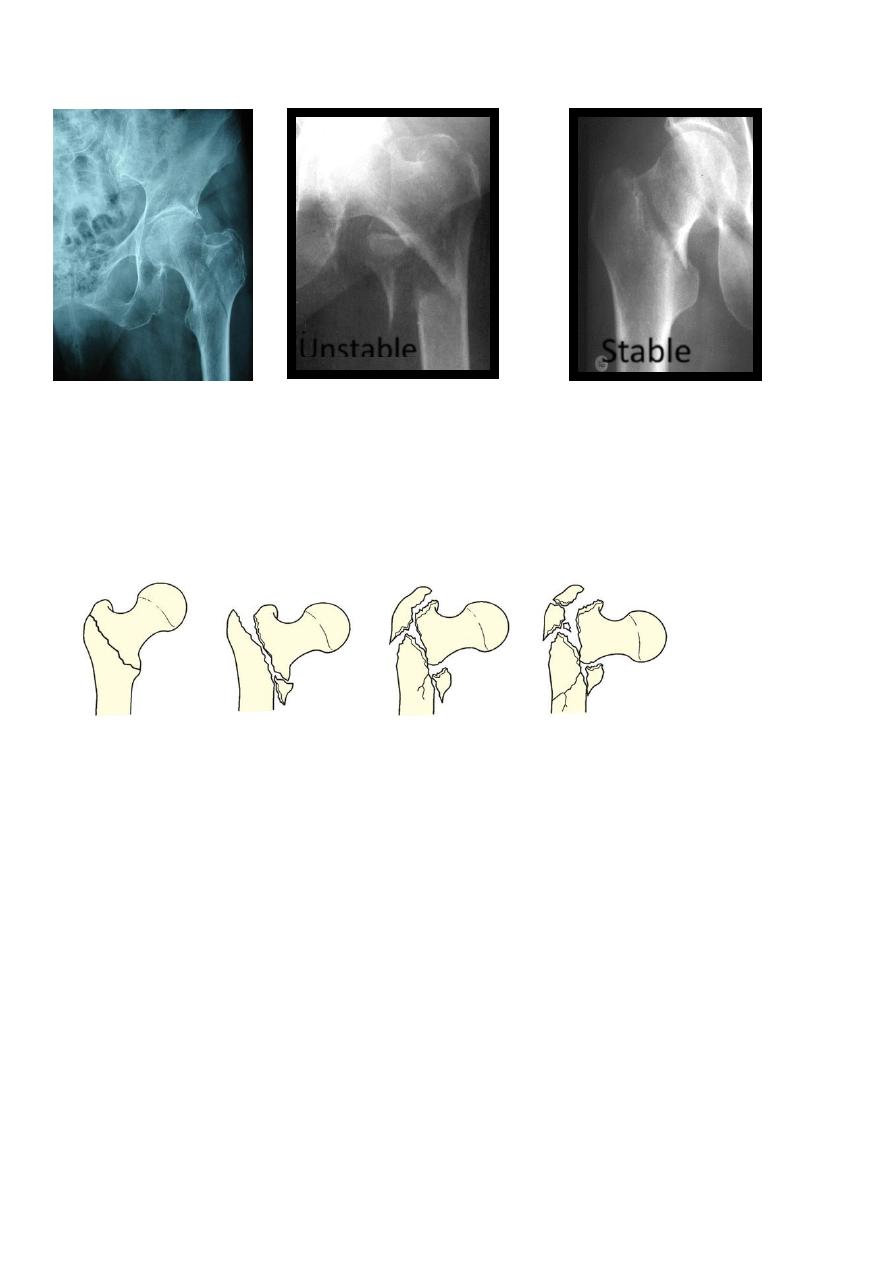
Generally the
intertrochanteric fractures are divided
into stable and unstable varieties (Evans). The unstable one is that when
>
2 pieces, Reverse
oblique and Subtrochanteric extension.
The importance of fracture pattern is detailed in the classification by Kyle (1994) which
distinguishes four basic patterns that reflect increasing the degree of the instability and
complexity and also increasing difficulty at reduction and fixation. Types 1 and 2 account for the
majority (nearly 60 per cent).
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
TYPE 1
TYPE 2
TYPE 3
TYPE 4
Type 1 :- Undisplaced, uncomminuted
Type 2 :- Displaced minimal comminuted lesser trochanter fracture varus
Type 3 :- Displaced greater trochanter fracture varus
Type 4 :- Severely comminuted subtrochanterec extension( reverse oblique)
Unstable
Stable

Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Clinical features
The patient is usually old and is unable to stand.
The leg is shorter and more externally rotated than with a transcervical fracture (because
the fracture is extracapsular) and the patient cannot lift his or her leg.
X-ray
--
Undisplaced, stable fractures may show no more than a thin crack along the
intertrochanteric line; the diagnosis may have to be confirmed by scintigraphy or MRI.
--
More often the fracture is displaced and there may be considerable comminution.
Treatment
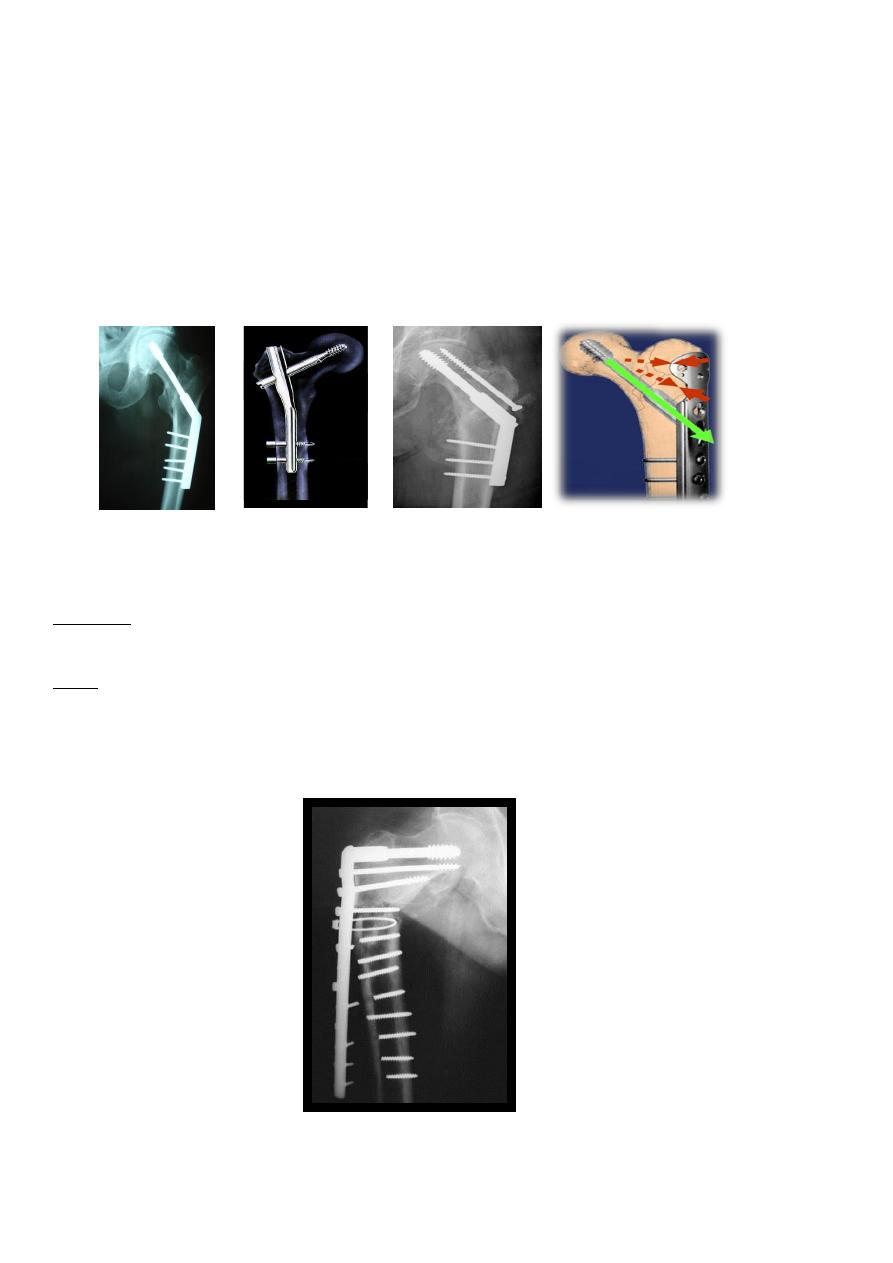
Intertrochanteric fractures are almost always treated by early internal fixation – not
because they fail to unite with conservative treatment (they unite quite readily), but (a) to
obtain the best possible position and (b) to get the patient up and walking as soon as
possible and thereby reduce the complications associated with prolonged recumbency.
Non-operative treatment may be appropriate for a small group who are too ill to undergo
anaesthesia; traction in bed until there is sufficient reduction of pain to allow mobilization
which much depends on the quality of nursing care and physical therapy.
Fracture reduction at surgery is performed on a fracture table that provides slight traction
and internal rotation; the position is checked by x-ray and the fracture is fixed with an
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
angled device – preferably a sliding screw in conjunction with a plate or intramedullary
nail. The side plate should be long enough to accommodate at least 4 screws below the
fracture line.
If closed reduction fails to achieve a satisfactory position, open reduction and
manipulation of the fragments will be necessary.
The addition of bone grafts may hasten union of the medial cortex.
Postoperatively, exercises are started on the day after operation and the patient allowed
up and partial weightbearing as soon as possible.
Complications
most of these
ctures,
fra
Early complications are the same as with femoral neck
-
:
EARLY
patients
are in poor health.
LATE
Failed fixation
Malunion Varus and external rotation deformities are common.
Non-union: Intertrochanteric fractures seldom fail to unite.
Failed fixation
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Pathological fractures
: in Intertrochanteric region
Intertrochanteric fractures may be due to metastatic disease or myeloma, In addition to
internal fixation, methylmethacrylate cement may be packed in the defect to improve
stability.
If there is involvement of the femoral neck, replacement with a cemented prosthesis may
be preferable.
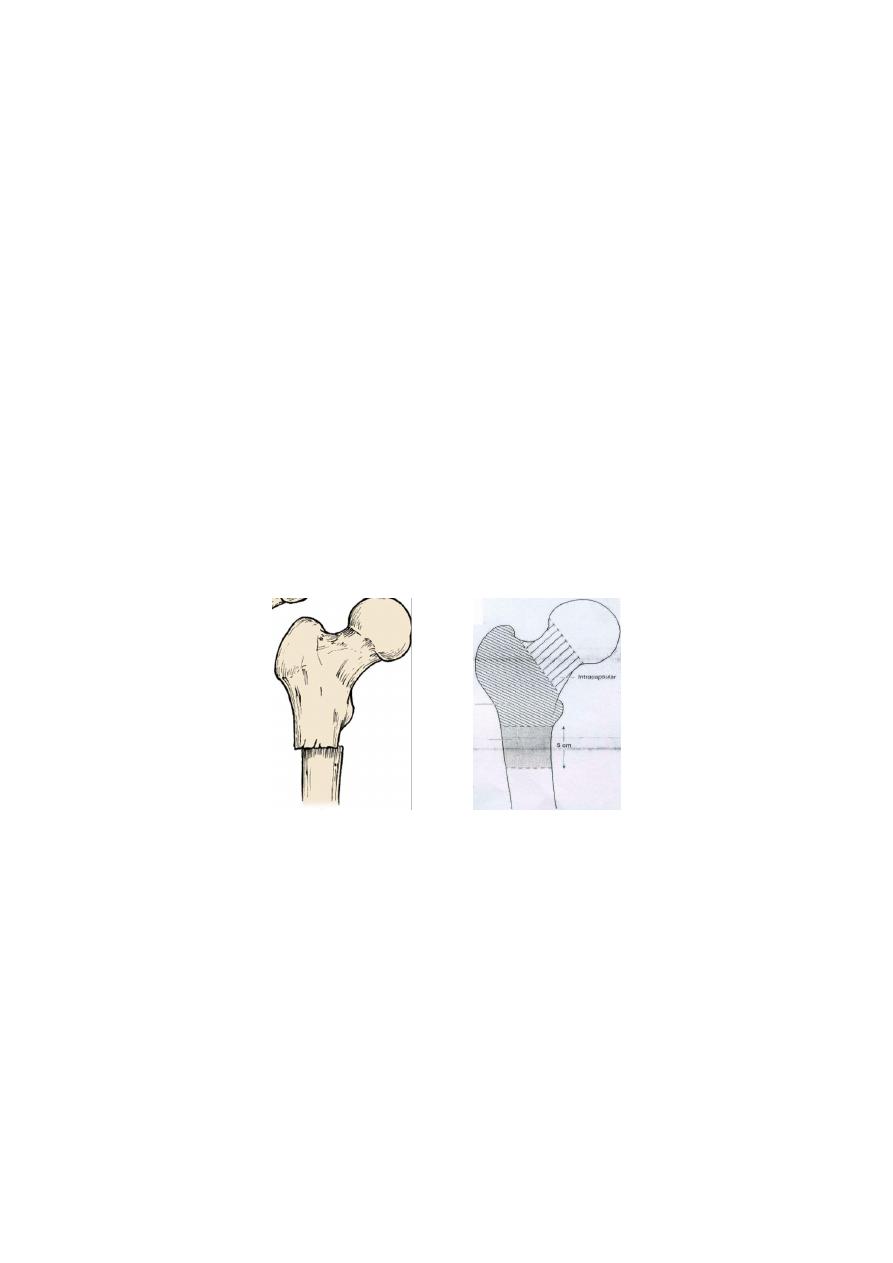
Subtrochanteric Fractures
Within 5cm from lesser trochanter
in young adults large forces are needed to cause the fractures in this area.
in the elderly, the fracture quite frequently, the injury is relatively trivial; here the reason is a
weakening of bone in this area by:- osteoporosis, osteomalacia, Paget’s disease, a secondary
deposit
Blood loss is greater than with femoral neck or trochanteric fractures.
There may be subtle extensions of the fracture into the intertrochanteric region.
The proximal part is abducted and externally rotated by the gluteal muscles, and flexed by the
psoas.
Clinical features
The leg lies in neutral or external rotation
looks short
the thigh is markedly swollen.
Movement is excruciatingly painful.
X-ray:-The fracture is through or below the lesser trochanter. It may be transverse, oblique or
spiral, and is frequently comminuted.
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Treatment
Traction may help to reduce blood loss and pain, until the patient, is stabilized and prepared for
surgery.
Open reduction and internal fixation is the treatment of choice.
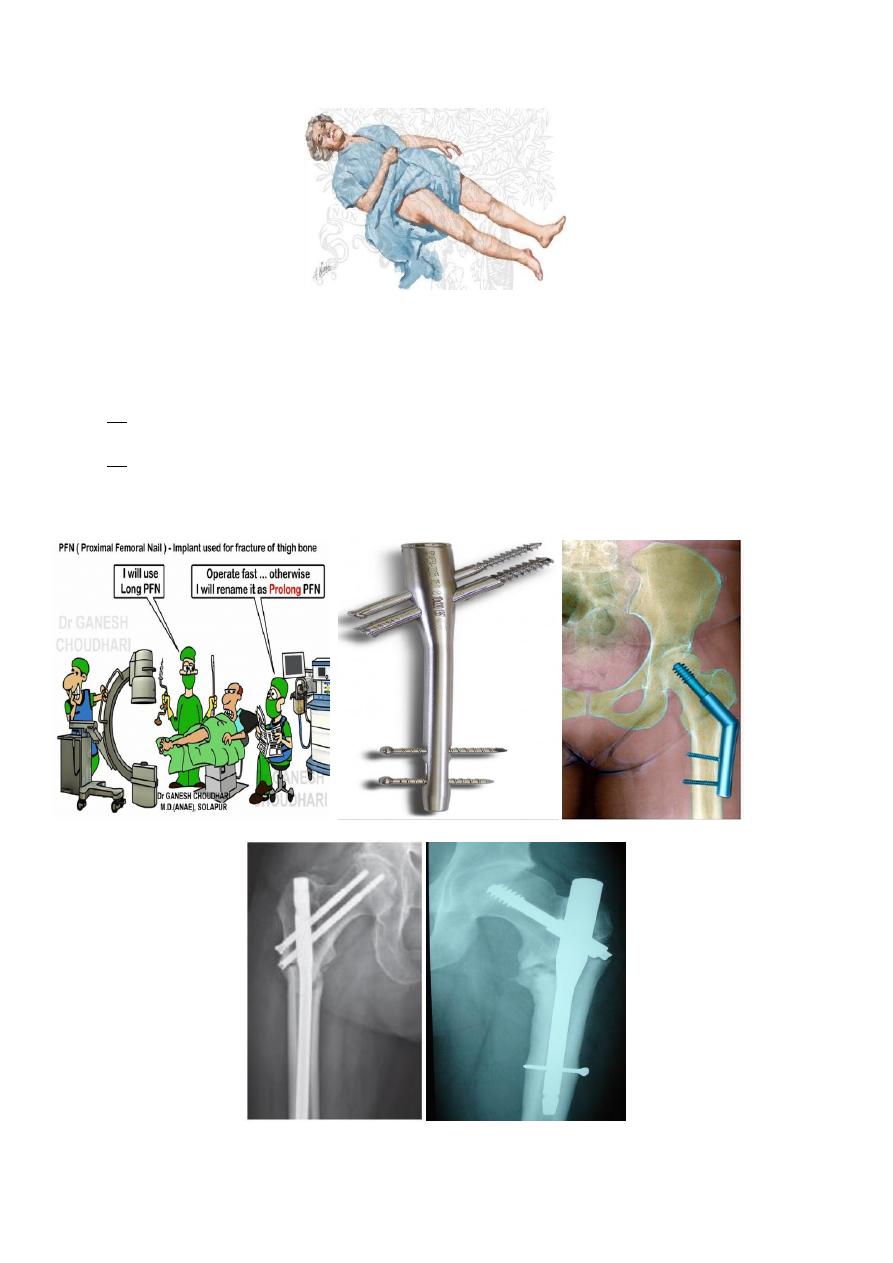
Two main types of implant are used for fracture fixation:
(a) an intramedullary nail with a proximal interlocking screw that can be directed into the
femoral head or placed in the standard manner
(b) a 95 degree hip screw-and-plate device.
Postoperatively the patient is allowed partial weightbearing (with crutches) until union is secure.

Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Complications
Malunion Varus and rotational malunions are fairly common.
Non-union This occurs in about 5 per cent of cases.
THANK YOU
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Assistant Professor and Consultant Orthopaedic Surgeon
