Otitis Media
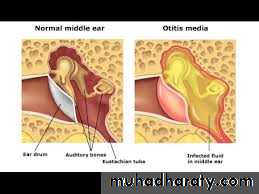
Inflammation and /or infection of the middle ear cleftSUPPURATIVE O.M.
NON SUPPURATIVE O.M.SUPPURATIVE O.M.
• ACUTE SUPPURATIVE O.M.• CHRONIC SUPPURATIVE O.M.
Acute suppurative otitis media
• Strep . Pneumonia
• Hemolytic strept.
• Staph aureous
• H . influenza
Branhamella catahralis
Beta- lactamase producing organism
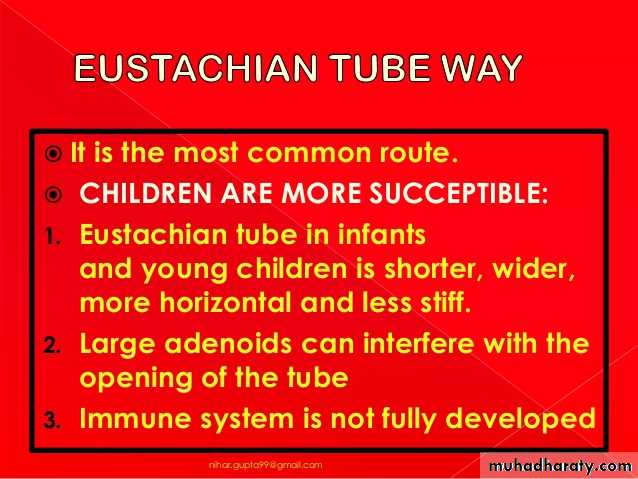
Ateology common in children /winter/viral //bacterial
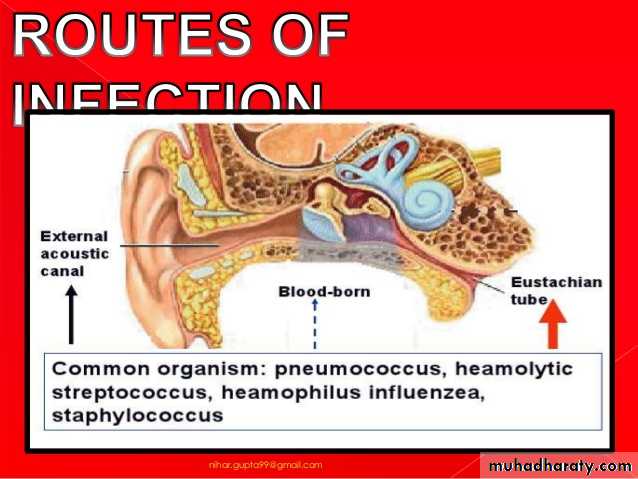
Routes of infection
* extension from infected N/Px viaan infected exudates through E.T.
or sub mucosal lymphatic vessels
** through perforated tymp. mem.
*** haematogenous route.
Pathology :
Tubal occlusionEngorgement & oedema of the cleft`s lining.
Exudation into the tympanic cavity /serous at beginning ----mucopurulent
Bulging of the T.M.
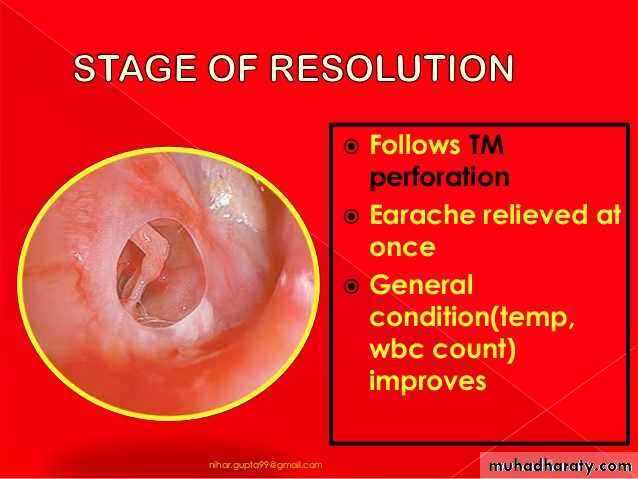
Pressure necrosis>>>rupture of the T.M. & otorrhoea
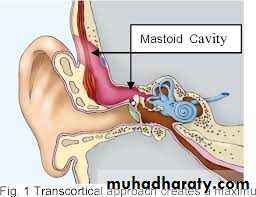
Exudation may be found in the mastoid process causes osteitis (mastoiditis)& erosion of the cortex >>>subperiosteal abscess
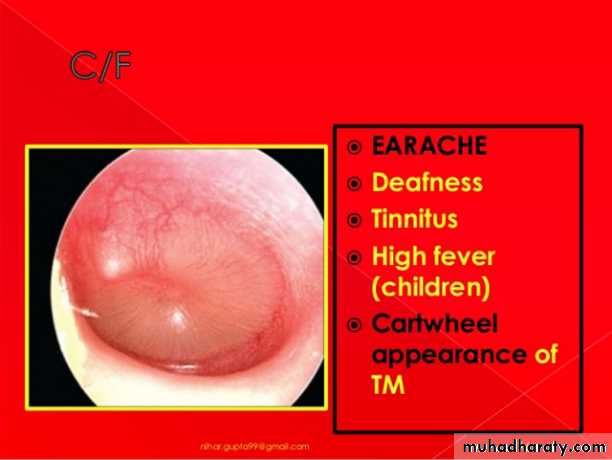
Clinical features:
Before perforation; (acute tubal occlusion)_ otalgia
- fullness in the ear.
_ deafness.
_ discomfort.
_ bubbling sound in the ear
_ autophonia
exam _ red t.m.
_ bulging.
After perforation
Relief of pain.otorrhoea
Retention of pus in the mastoid(mastoiditis)
pain in the mastoid regionOedema over the mastoid process
Increase constitutional features/ fever,pain ,malaise….etc
Treatment :
rest & sedationAnalgesia
Local heat
swab for C/S (discharge)
Systemic antibiotics
Local treatment AB. +/- steroid
Nasal decongestant drops
Cortical mastoidectomy
Chronic otitis media
TubotympanicAttico antral
1-Tubotympanic
Aetiology:
*- residue of acute s.o.m.
**- re infection
Pathology of tubotympanic c.s.o.m.
PerforationOedematous mucosa of the tympanic Cavity
Occasionally aural polyp or granulation tissue
Metaplasia of non secretory epith. >>> sec. col. Epith >>discharge
Same changes in the mastoid air cells>>chronic mastoiditis (mastoid reservoir)
Clinical features
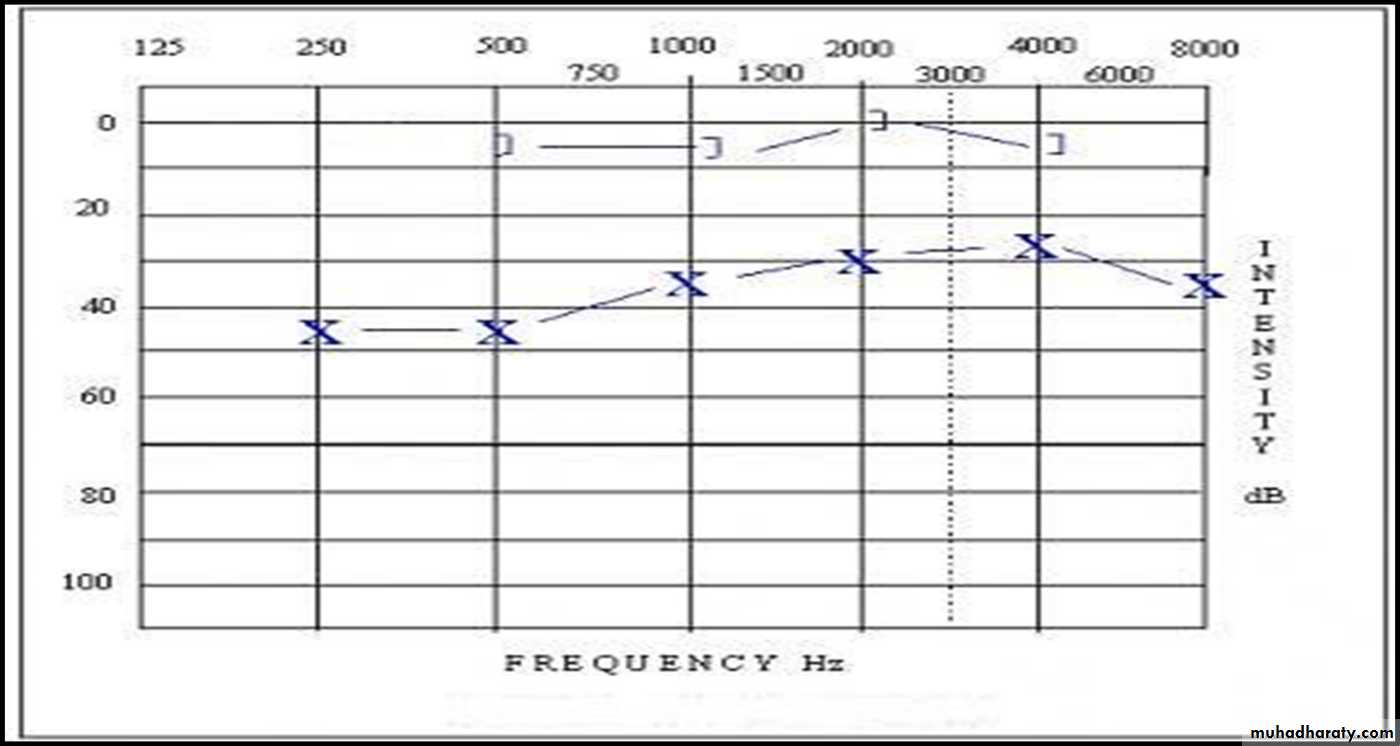
• Discharge ; often scanty mucoid, but becomes copious & purulent during exacerbation of U.R.T.I.• Conductive deafness
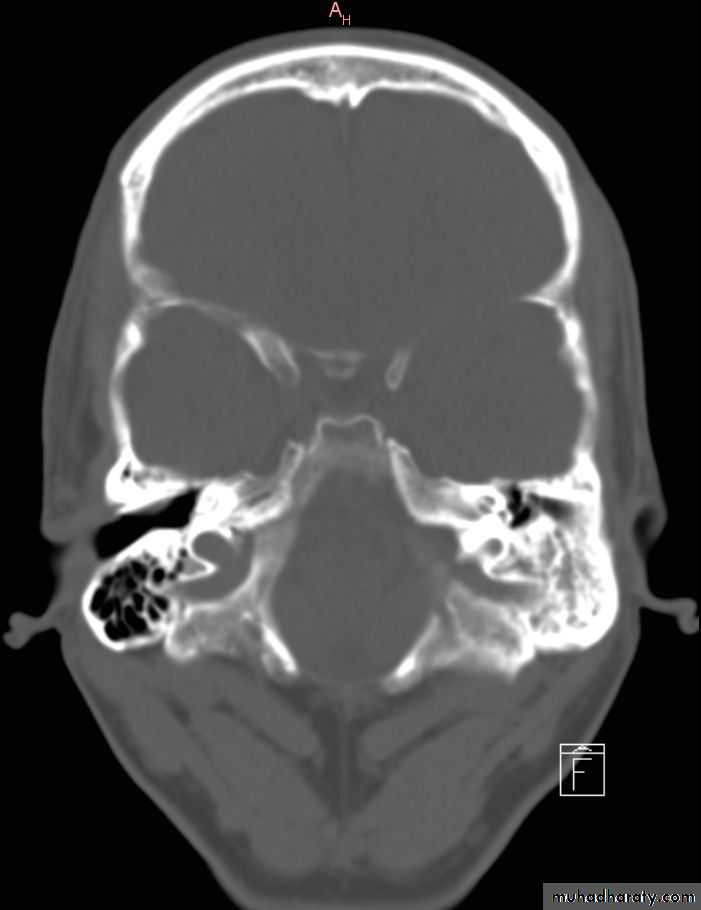
• Radiological findings reveals , sclerosis of the mastoid air cells
Treatment:
• Swab for C/S• Aural toilet
• Systemic& local AB.
• Removal of the polyp & gr. t. if present
• Elimination of the adjacent foci of infection/ts.,sinusitis…etc
• Mastoid exploration
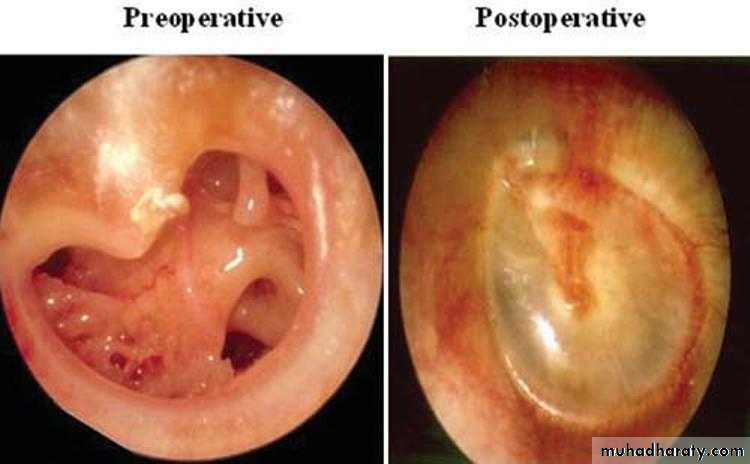
• Myringoplasty for dry perforation
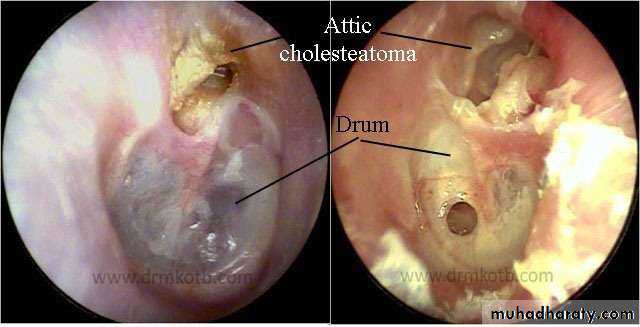
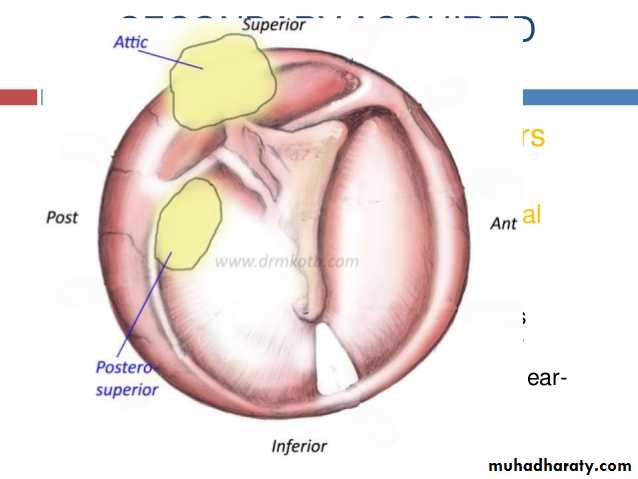
2- attico-antral
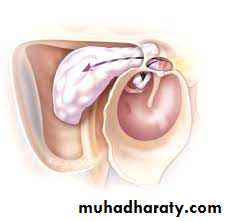
Dangerous diseaseAss. Cholesteatoma (epidermoid cyst containing keratin with cholestrol crystals)
Pathology:
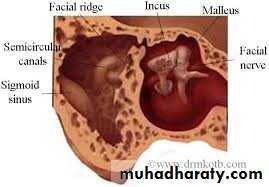
Disease is limited at attic region (pars flaccida) or extruteded into ext.canal.Extension into the tymp. Cavity +/- ossicular chain disruption.
Expansion into the mastoid bone >>absorption of the bone(auto mastoidectomy)
Gr. T. & polyp
Invasion of the labyrinth >> fistula & SNHL.
Invasion of the meninges >>meningitis
Pressure on the facial n.>> palsy
Clinical features :
• Deafness• Malodourous scanty otorrhoea
• Perforation // attic or mariginal
• Cholesteotoma may be visible as keratin leaf
• Signs of complications may be found ; fever, headache ,earache, vertigo, facial palsy .
• Radiological findings shows bone destruction in the advance stage
•
Treatment:
• Conservative R;• * if no complications or small cholesteatoma
• via repeated suction clearance & regular follow up
• Surgical R;
• - complications
• - fail of cons. R,
• * atticotomy
• * mastoidectomy
• * tympanoplasty (removal of the disease & reconstruction of the ossicular chain)
complications
• Sub periosteal abscess• Facial n. palsy
• Labyrinthitis
• Meningitis
• Thrombophlebitis of the sigmoid sinus
• Brain abscess
• septicemia