Talib Hassan
12th lectureDisorders in Immunity 2
1
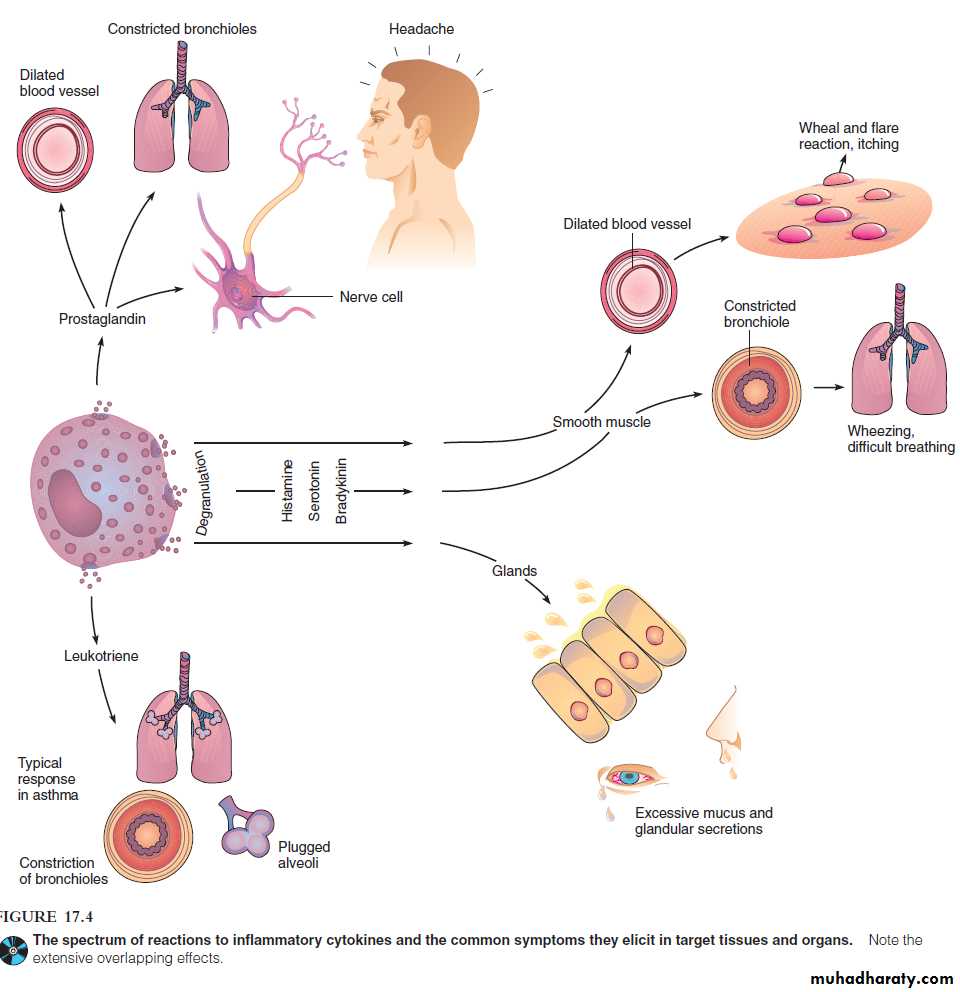
Cytokines, target organs, and allergic symptoms
Numerous substances involved in mediating allergy (and inflammation) have been produced by mast cells and basophilsThese chemicals, acting alone or in combination. Targets of these mediators include the skin, upper respiratory tract, gastrointestinal tract, and conjunctiva.
The general responses of these organs include rashes, itching, redness, rhinitis, sneezing, diarrhea, and shedding of tears.
12th lecture
2
Systemic targets include smooth muscle, mucous glands, and nervous tissue. Because smooth muscle is responsible for regulating the size of blood vessels and respiratory passageways, changes in its activity can profoundly alter blood flow, blood pressure, and respiration.
12th lecture
3Histamine: is the fastest-acting allergic mediator and potent stimulator of smooth muscle, glands, and eosinophils.
Histamine’s actions on smooth muscle vary with location. It constricts the smooth muscle layers of the small bronchi and intestine, thereby causing labored breathing and increased intestinal motility.
In contrast, relaxes vascular smooth muscle and dilates arterioles and venules. It is responsible for the reaction in the skin, itching, and headache.
More severe reactions (such as anaphylaxis) can be accompanied by edema and vascular dilation, which lead to hypotension, tachycardia, circulatory failure, and, frequently, shock. Salivary, lacrimal, mucous, and gastric glands are also histamine targets.
4
12th lecture
Serotonin: it is allergy effects is appear to complement those of histamine.
It is increasesvascular permeability,
capillary dilation,
smooth muscle contraction,
intestinal peristalsis,
respiratory rate,
but it diminishes central nervous system activity.
5
12th lecture
Leukotriene:
inducing gradual contraction of smooth muscle,prolonged bronchospasm,
vascular permeability,
mucous secretion
stimulate the activities of PMNs.
6
Platelet-activating factor:
is a lipid released by basophils, neutrophils, monocytes, and macrophages that causes platelet aggregation and lysis.The physiological response to stimulation by this factor is similar to that of histamine.
7
Prostaglandins:
are a group of powerful inflammatory agents, regulate smooth muscle contraction (for example, they stimulate uterine contractions during delivery).
In allergic reactions, they are responsible for
vasodilation,
increased vascular permeability,
increased sensitivity to pain,
bronchoconstriction.
8
12th lecture
Bradykinin:
is related to a group of plasma and tissue peptides known as kinins that participate in blood clotting and chemotaxis.In allergy, it causes
prolonged smooth muscle contraction of the bronchioles,
dilatation of peripheral arterioles,
increased capillary permeability,
increased mucous secretion.
9
10
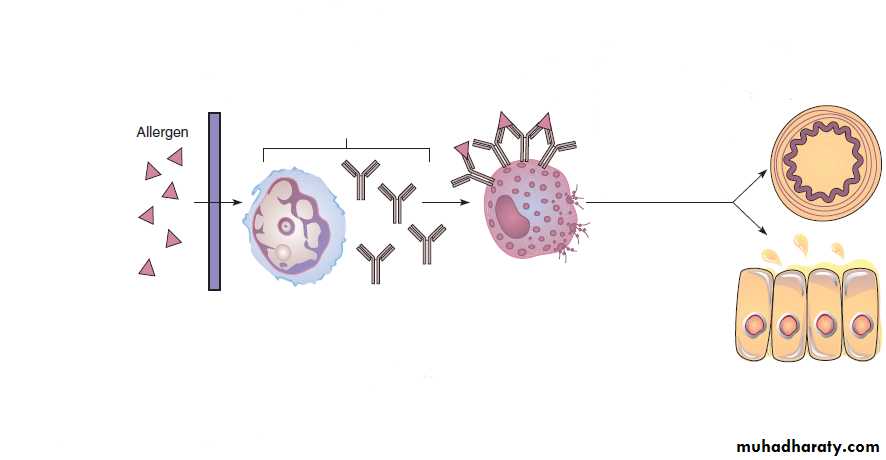
Specific IgE and Mast Cell-Mediated Allergy
1112th lecture
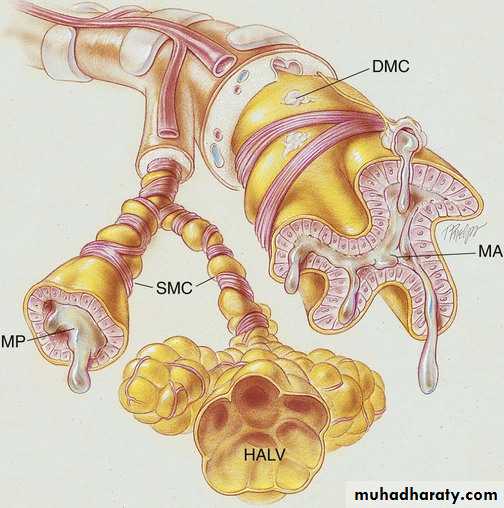
Asthma: is a respiratory disease characterized by episodes of impaired breathing due to severe bronchoconstriction.
The airways of asthmatic people are responsive to minute amounts of inhalant allergens, food, or other stimuli, such as infectious agents.
The symptoms of asthma range from occasional, annoying bouts of difficulty breathing to fatal suffocation. Labored breathing, shortness of breath, wheezing, and cough are present to one degree or another.
The respiratory tract is chronically inflamed and severely overreactive to allergy chemicals, especially leukotrienes and serotonin from pulmonary mast cells.
12
Other pathologic components are thick mucous plugs in the air sacs and lung damage that can result in long-term respiratory compromise.
An imbalance in the nervous control of the respiratory smooth muscles is apparently involved in asthma, and the episodes are influenced by the psychological state of the person, which strongly supports a neurological connection.
13
12th lecture
DMC, Degranulation of mast cell; HALV, hyperinflation of alveoli; MA, mucous accumulation; MP, mucous plug; SMC, smooth muscle constriction (bronchospasm)
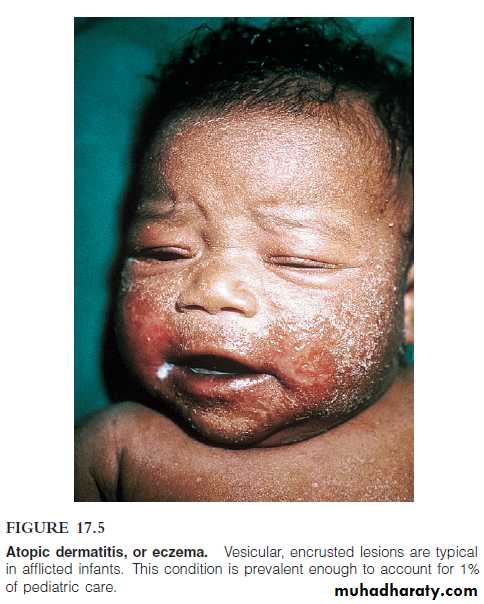
Atopic dermatitis
It is an intensely itchy inflammatory condition of the skin, sometimes also called eczema.Sensitization occurs through ingestion, inhalation, and, occasionally, skin contact with allergens.
It usually begins in infancy with reddened, vesicular, weeping, encrusted skin lesions.
It then progresses in childhood and adulthood to a dry, scaly, thickened skin condition.
Lesions can occur on the face, scalp, neck, and inner surfaces of the limbs and trunk. The itchy, painful lesions cause considerable discomfort, and they are often predisposed to secondary bacterial infections.
14
12th lecture
Food Allergy
The ordinary diet contains a vast variety of compounds that are potentially allergenic, may be an additive (preservative or flavoring).food allergies can also affect the skin and respiratory tract.
Gastrointestinal symptoms include vomiting, diarrhea, and abdominal pain.
In severe cases, nutrients are poorly absorbed, leading to growth retardation.
Other manifestations of food allergies include eczema, hives, rhinitis, asthma, and occasionally, anaphylaxis.
The most common food allergens come from peanuts, fish, cow’s milk, eggs, shellfish, and soybeans.
15
12th lecture
12th lecture
16Drug Allergy
drugs are foreign compounds capable of stimulating allergic reactions. In fact, allergy to drugs is one of the most common side effects of treatment (present in 5–10% of hospitalized patients).virtually any tissue of the body can be affected, and reactions range from mild atopy to fatal anaphylaxis.
Compounds auch as antibiotics (penicillin) synthetic antimicrobics (sulfa drugs), aspirin, and anaesthetics.
Some forms of penicillin sensitivity are due to the presence of small amounts of the drug in meat, milk, and other foods and to exposure to Penicillium mold in the environment.
17
12th lecture
Anaphylaxis
Two clinical types of anaphylaxis are distinguishedCutaneous anaphylaxis: the local injection of allergen.
Systemic anaphylaxis: sudden respiratory and circulatory disruption that can be fatal in a few minutes.
concentration of chemical mediators and the strength of the response are greatly amplified.
The immune system exposed to a provocative dose of allergen responds with a sudden, massive release of chemicals into the tissues and blood.
Anaphylactic persons have been known to die in 15 minutes from complete airway blockage.
18
12th lecture
DIAGNOSIS OF ALLERGY
including nonspecific, specific, in vitro, and in vivo methods.tests measures
elevated blood levels of tryptase, (an enzyme released by mast cells that increases during an allergic response).
The leukocyte histamine-release test measures the amount of histamine released from the patient’s basophils when exposed to a specific allergen.
Serological tests that use radioimmune assays to reveal the quantity and quality of IgE are also clinically helpful.
19
12th lecture
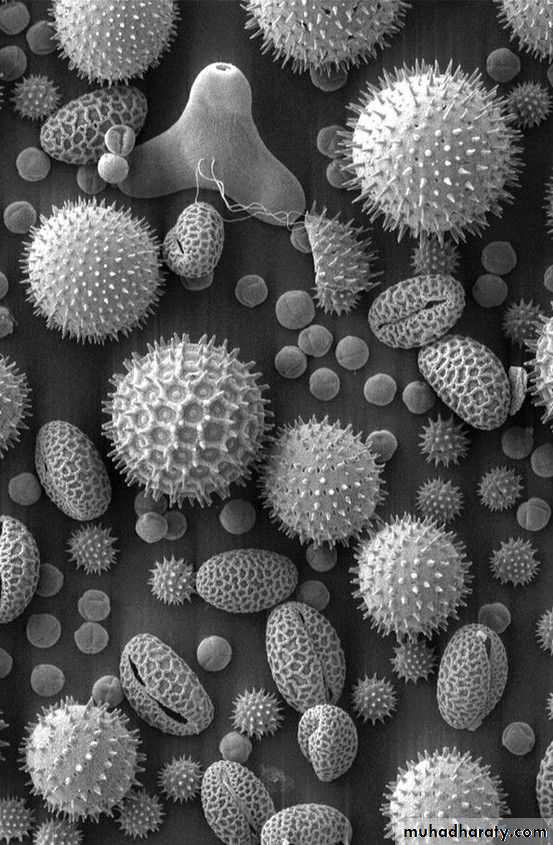
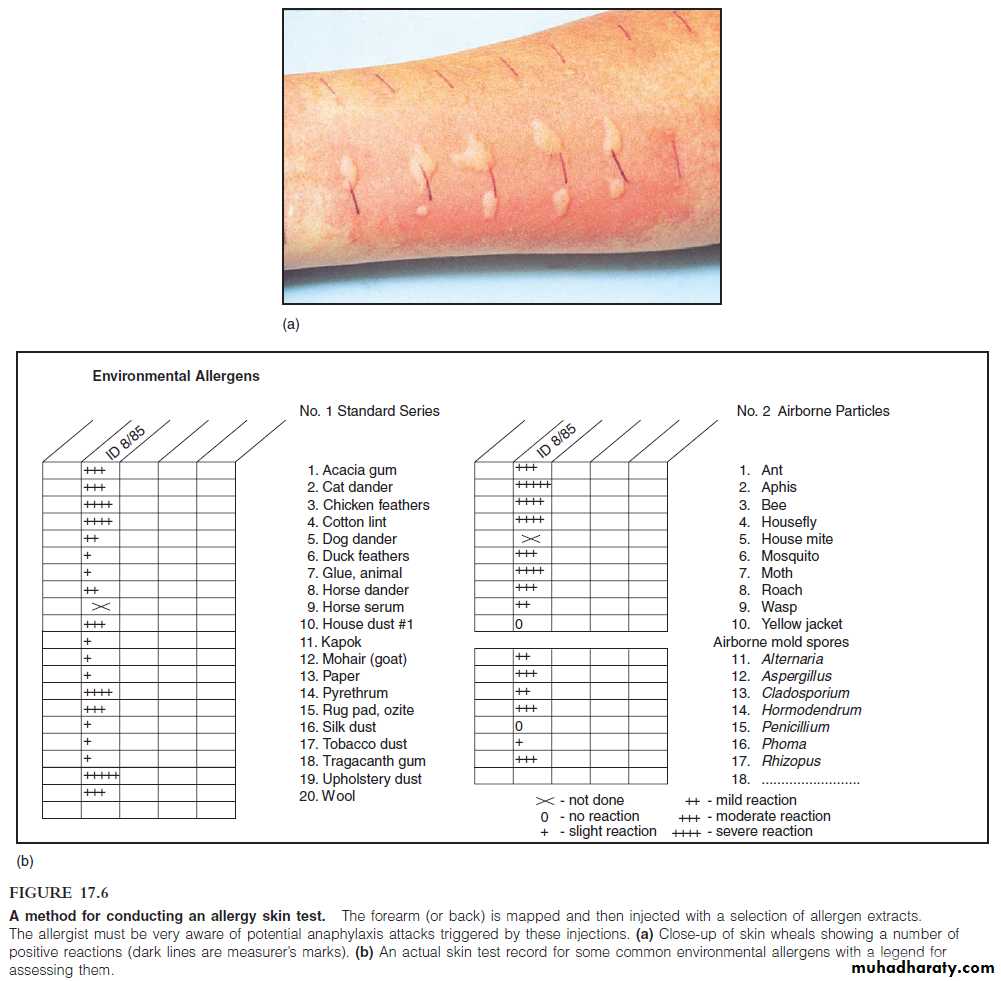
Skin Testing
in vivo method to detect sensitivities is skin testing.patient’s skin is injected, scratched, or pricked with a small amount of a pure allergen extract (common airborne allergens (plant and mold pollen) and unusual allergens (mule dander, theater dust, bird feathers).
Approximately 20 minutes after antigenic challenge, each site is appraised for a wheal response indicative of histamine release.
The diameter of the wheal is measured and rated on a scale of 0 (no reaction) to 4" (greater than 15 mm).
20
12th lecture
21
TREATMENT AND PREVENTION OF ALLERGY
treating and preventing type I allergy involve:• Avoiding the allergen
• Taking drugs that block the action of lymphocytes, mast cells, or chemical mediators.
• Undergoing desensitization therapy.
since there is no way to tell in advance if a person will develop an allergy to a particular substance. Although rigorous cleaning and air conditioning can reduce contact with airborne allergens, it is not feasible to isolate a person from all allergens, which is the reason drugs are so important in control.
22
12th lecture
Therapy to Counteract Allergies
anti allergy medication is to block the progress of the allergic response.Oral anti-inflammatory drugs such as corticosteroids inhibit the activity of lymphocytes and reduce the production of IgE, but they also have dangerous side effects and should not be taken for prolonged periods.
Some drugs block the degranulation of mast cells and reduce the levels of inflammatory cytokines.
Asthma and rhinitis sufferers can find relief with a new drug that blocks synthesis of leukotriene and a monoclonal antibody that inactivates IgE (Xolair).
23
12th lecture
24
Avoidance
of allergenCorticosteroids
keep the plasma cell
from synthesizing IgE
and inhibit T cells.
12th lecture
antihistamines interfere with histamine activity by binding to histamine receptors on target organs.aspirin and acetaminophen, which reduce pain by interfering with prostaglandin.
theophylline, a bronchodilator that reverses spasms in the respiratory smooth muscles.
epinephrine can reverses constriction of the airways and slows the release of allergic mediators.
25
12th lecture
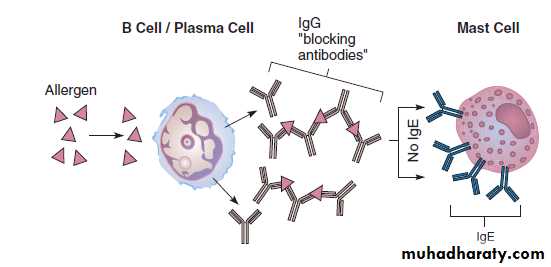
desensitization or hyposensitization, is a controlled injections of specific allergens to prevent reactions between allergen, IgE, and mast cells, by stimulate the formation of high levels of allergen-specific IgG that block or remove allergen from the system before it can bind to IgE, thus preventing the degranulation of mast cells.
It is also possible that allergen delivered in this fashion combines with the IgE itself and prevents it from reacting with the mast cells.
12th lecture
26
The blocking antibody theory for allergic desensitization. An injection of allergen causes IgG antibodies to be formed instead of IgE; these blocking antibodies cross-link and effectively remove the allergen before it can react with the IgE in the mast cell.
12th lecture
27