MalignantEpidemiologyAbout 22 000 patients are diagnosed with colonic cancer everyyear. Over the last four decades, the 5-year survival rate hasimproved from 30% to about 45%.
AetiologyOther than genetic factors that have been implicated in the development of cancer have included dietary fibre. The hypothesis is that increased roughage is associated with reduced transit times, and this in turn reduces the exposure of the mucosa to carcinogens. Also increased dietary animal fat, smoking and alcohol to colorectal cancer. There is some evidence that links cholecystectomy, and therefore increased bile acid secretion, to an increased risk of colorectal cancer.
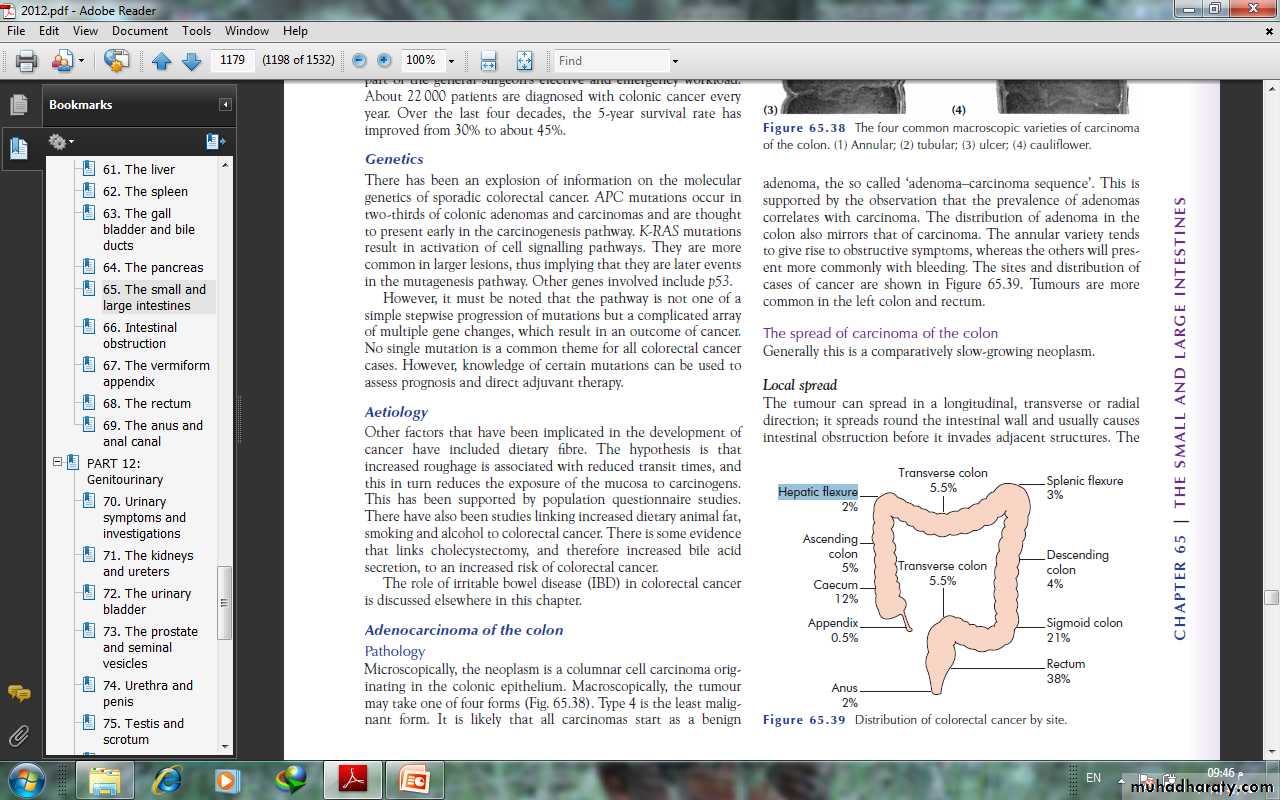
Adenocarcinoma of the colonPathologyMicroscopically, the neoplasm is a columnar cell carcinoma originating in the colonic epithelium. Macroscopically, the tumourmay take one of four forms (1) Annular; (2) tubular; (3) ulcer; (4) cauliflower. Type 4 is the least malignant form. It is likely that all carcinomas start as adenoma, the so called ‘adenoma–carcinoma sequence’.
The annular variety tendsto give rise to obstructive symptoms, whereas the others will present more commonly with bleeding. Tumours are morecommon in the left colon and rectum.
The spread of carcinoma of the colonGenerally this is a comparatively slow-growing neoplasm.Local spreadThe tumour can spread in a longitudinal, transverse or radialdirection; it spreads round the intestinal wall and usually causesintestinal obstruction before it invades adjacent structures.
ulcerative type more commonly invades locally, and an internalfistula may result, for example into the bladder.
Lymphatic spreadLymph nodes draining the colon are grouped as follows:N1: nodes in the immediate vicinity of the bowel wall;N2: nodes arranged along the ileocolic, right colic, midcolic, leftcolic and sigmoid arteries;N3: the apical nodes around the superior and inferior mesentericvessels where they arise from the abdominal aorta.
Bloodstream spreadMetastases are carried to the liver via the portal system, sometimes at an early stage before clinical or operative evidence isdetected (occult hepatic metastases).Transcoelomic spreadRarely, colorectal cancer can spread by way of cells dislodgingfrom the serosa of the bowel to other structures within the peritoneal cavity.
Staging colon cancerThere are several staging systems that are used such as Dukes,tumour–node–metastasis (TNM) . All of them can be usedin order to predict prognosis and standardise treatment, Dukes’ classification for colon cancer is as follows:A: confined to the bowel wall;B: through the bowel wall but not involving the serosa;C: lymph nodes involved.Dukes himself never described a D stage, but this is often used todescribe either advanced local disease or metastases to the liver.
TNM classificationThe TNM classification is more detailed and accurate but moredemanding:• T Tumour stage;• T1 Into submucosa;• T2 Into muscularis propria;• T3 Into pericolic fat but not breaching serosa;• T4 Breaches serosa or directly involving another organ;• N Nodal stage;• N0 No nodes involved;• N1 One or two nodes involved;• N2 Three or more nodes involved;• M Metastases;• M0 No metastases;• M1 Metastases;
Clinical features Carcinoma of the colon usually occurs in patients over 50 years of age, but it is not rare earlier in adult life. Twenty per cent of cases present as an emergency with intestinal obstruction or peritonitis. Those with first-degree relatives who have developed colorectal cancer at the age of 45 years or below are at high risk and may be part of one of the colorectal cancer family syndromes.
Carcinoma of the left side of the colonMost tumours occur in this location. They are usually of thestenosing variety.SymptomsThe main symptoms are those of increasing intestinal obstruction.This includes lower abdominal pain, which may be colickyin nature, and abdominal distension. The patient may have achange in bowel habit with alternating diarrhoea and constipation
Carcinoma of the sigmoidIn addition to symptoms of intestinal obstruction, a low tumourmay give rise to a feeling of the need for evacuation, which mayresult in tenesmus accompanied by the passage of mucus andblood. Bladder symptoms are not unusual and, in some instances,may herald a colovesical fistula.Carcinoma of the transverse colonThis may be mistaken for a carcinoma of the stomach because ofthe position of the tumour together with anaemia and lassitude.
Carcinoma of the caecum and ascending colonThis may present with the following:• anaemia, severe and unrespond to treatment;• the presence of a mass in the right iliac fossa• a carcinoma of the caecum can be the apex of an intussusceptionpresenting with the symptoms of intermittent obstruction.
Metastatic diseasePatients may present for the first time with liver metastases andan enlarged liver, ascites from carcinomatosis peritonei and, morerarely, metastases to the lung, skin, bone and brain.
Methods of investigation of colon cancerFlexible sigmoidoscopyThe 60-cm, fibreoptic, flexible sigmoidoscope is increasinglybeing used in the out-patient clinic or in special rectal bleedingclinics. The patient is prepared with a disposable enema andsedation is not usually necessary. This is particularly useful in supplementing barium investigations where diagnosis is difficult due to diverticular disease.
ColonoscopyThis is now the investigation of choice if colorectal cancer is suspected provided the patient is fit enough to undergo the bowelpreparation. It has the advantage of not only picking up a primarycancer but also having the ability to detect synchronous polyps oreven multiple carcinomas, which occur in 5% of cases. Ideally,every case should be proven histologically before surgery. Fullbowel preparation and sedation are necessary. However, one mustbe aware of a small risk of perforation.
RadiologyDouble-contrast barium enema is used when colonoscopy is contraindicated.it shows a cancer of the colon as a constant irregular filling defect.Ultrasonography is often used as a screening investigation forliver metastases over the size of 1.5 cm, and CT is used in patientswith large palpable abdominal masses, to determine local invasion,and is particularly used in the pelvis in the assessment ofrectal cancer.
Apple core appearance
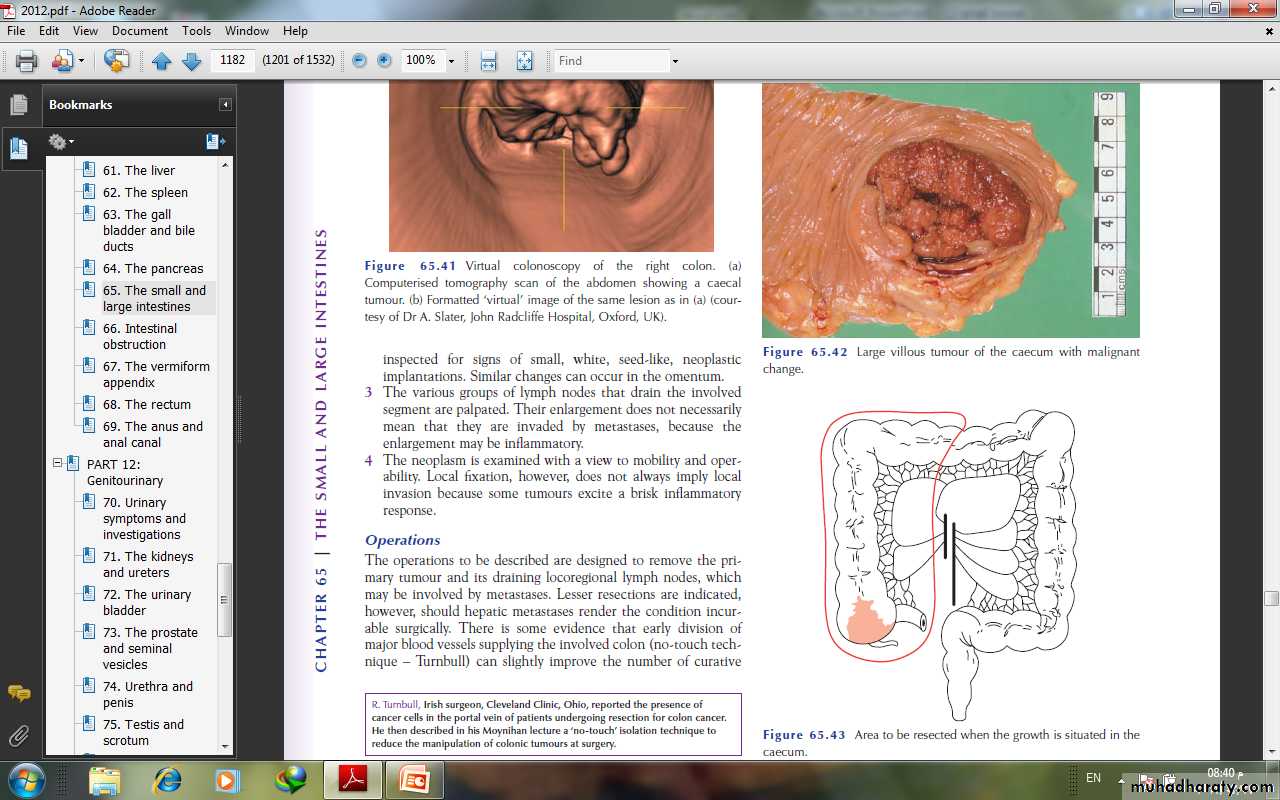
there has been the introduction of virtual colonoscopy, which is effective in picking up polyps down to size of 6 mm. This mayeven replace colonoscopy as the standard investigation in thefuture. Urograms have a role in left-sided tumours where there is evidence of hydronephrosis on CT or ultrasound.
TreatmentPreoperative preparationRecent literature has suggested that no bowel preparation is safefor right-sided colonic surgery. The most commonly used methodis dietary restriction to fluids only for 48 hours before surgery; onthe day before the operation, two sachets of Picolax are taken to purge the colon. In addition, a rectal washout may be necessary. A stoma site is carefully discussed with the stoma care nursing specialist and anti-embolus stockings are fitted; the patient is started on prophylactic subcutaneous heparin, and intravenous prophylactic antibiotics are given at the start of surgery.
When intestinal obstruction is present, preparation in this waymay precipitate abdominal pain, and it may be safer to use an ontable lavage technique at the time of the operation
The test of operabilityThe abdomen is opened and the tumour assessed for resectability.1 The liver is palpated for secondary deposits, the presence ofwhich is not necessarily a contraindication to resection.2 The peritoneum, particularly the pelvic peritoneum, isinspected for signs of small, white, seed-like, neoplasticimplantations.3 The various groups of lymph nodes that drain the involvedsegment are palpated.4 The neoplasm is examined with a view to mobility and operability.
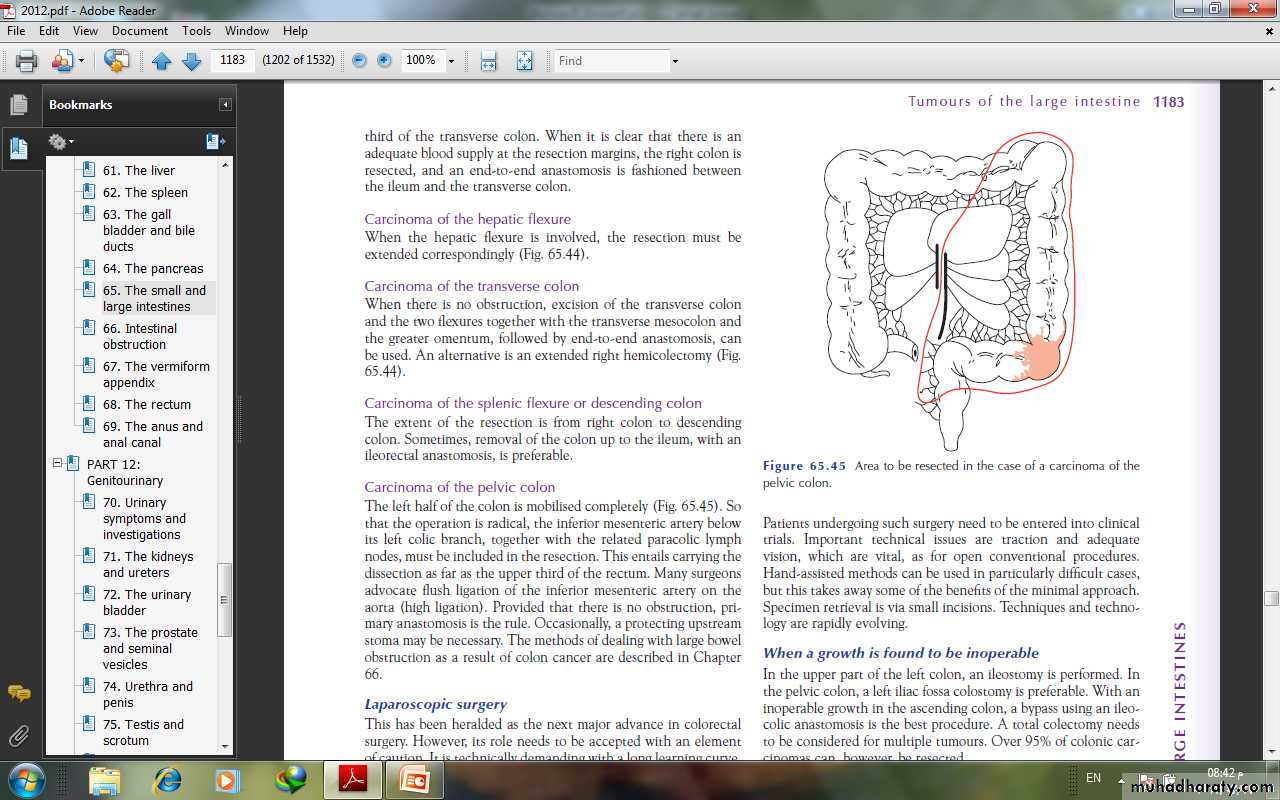
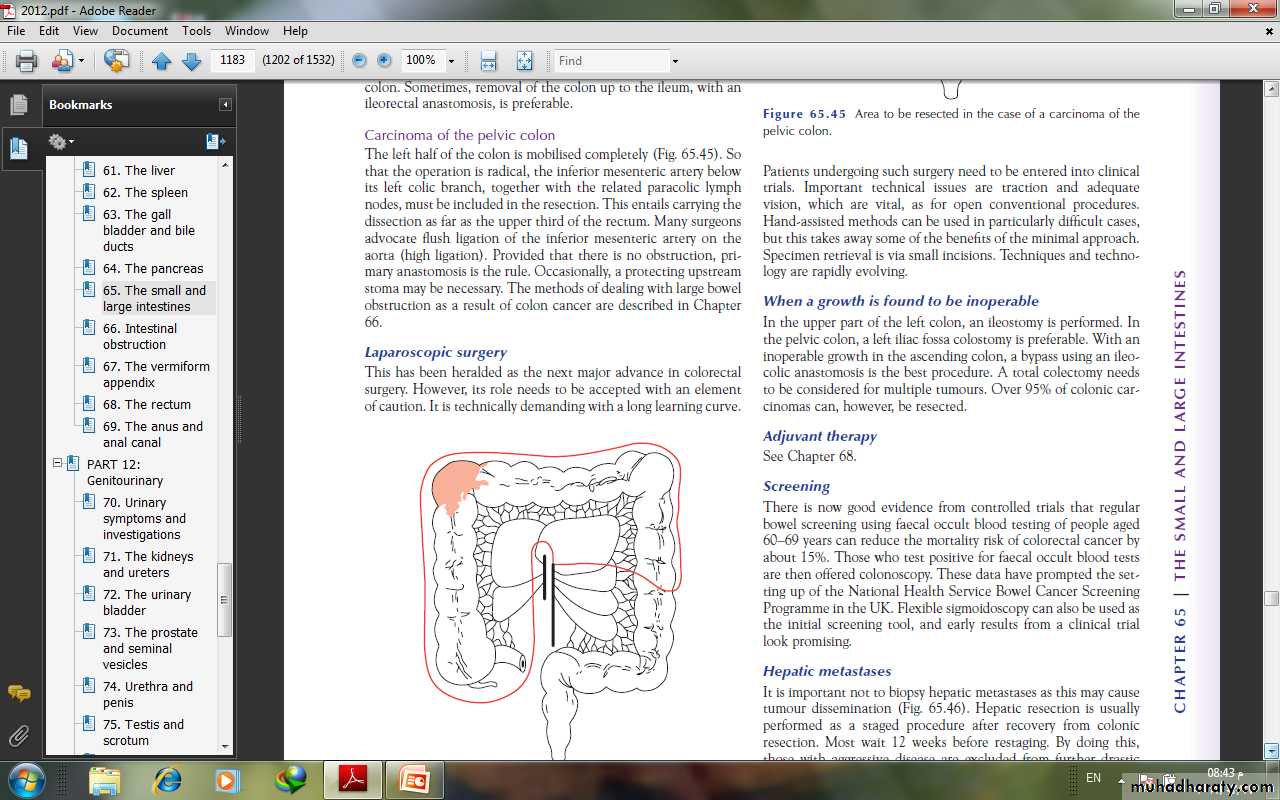
OperationsThe operations to be described are designed to remove the primary tumour and its draining locoregional lymph nodes, whichmay be involved by metastases. Lesser resections are indicated,however, should hepatic metastases render the condition incurable surgically. There is some evidence that early division ofmajor blood vessels supplying the involved colon (no-touch technique.
When a growth is found to be inoperableIn the upper part of the left colon, an ileostomy is performed. Inthe pelvic colon, a left iliac fossa colostomy is preferable. With aninoperable growth in the ascending colon, a bypass using an ileocolic anastomosis is the best procedure.
ScreeningThe regular bowel screening using faecal occult blood testing of people aged 60–69 years can reduce the mortality risk of colorectal cancer by about 15%. Those who test positive for faecal occult blood tests are then offered colonoscopy. Flexible sigmoidoscopy can also be used as the initial screening .
OTHER DISORDERSTraumatic ruptureThe intestine can be ruptured with or without an external wound– so called blunt trauma . The most common cause ofthis is a blow to the abdomen that crushes the bowel against thevertebral column or sacrum; also, a rupture is more likely to occurwhere part of the gut has been fixed, for example in a hernia, orwhere a fixed part of the gut joins a mobile part such as the duodenojejunal flexure.
In small perforations, the mucosa may prolapse through thehole and partly seal it, making the early signs misleading. In addition, there may be a laceration in the mesentery. The patient will then have a combination of intra-abdominal bleeding and release of intestinal contents into the abdominal cavity, giving rise to peritonitis.
Traumatic rupture of the large intestine is much less common.In blast injuries of the abdomen following the detonation of a bomb, the pelvic colon is particularly at risk of rupture. Compressed air rupture can follow the dangerous practical joke of turning on an airline carrying compressed air near the victim’s anus.
STOMASColostomyA colostomy is an artificial opening made in the large bowel todivert faeces and flatus to the exterior, where it can be collectedin an external appliance. Depending on the purpose for which thediversion has been necessary, a colostomy may be temporary orpermanent.
Temporary colostomyA transverse loop colostomy has in the past been most commonlyused to defunction an anastomosis after an anterior resection. Itis now less commonly employed as it is fraught with complicationsand is difficult to manage; a loop ileostomy is preferred.A loop left iliac fossa colostomy is still sometimes used to preventfaecal peritonitis developing following traumatic injury tothe rectum, to facilitate the operative treatment of a high fistulain-ano and incontinence.
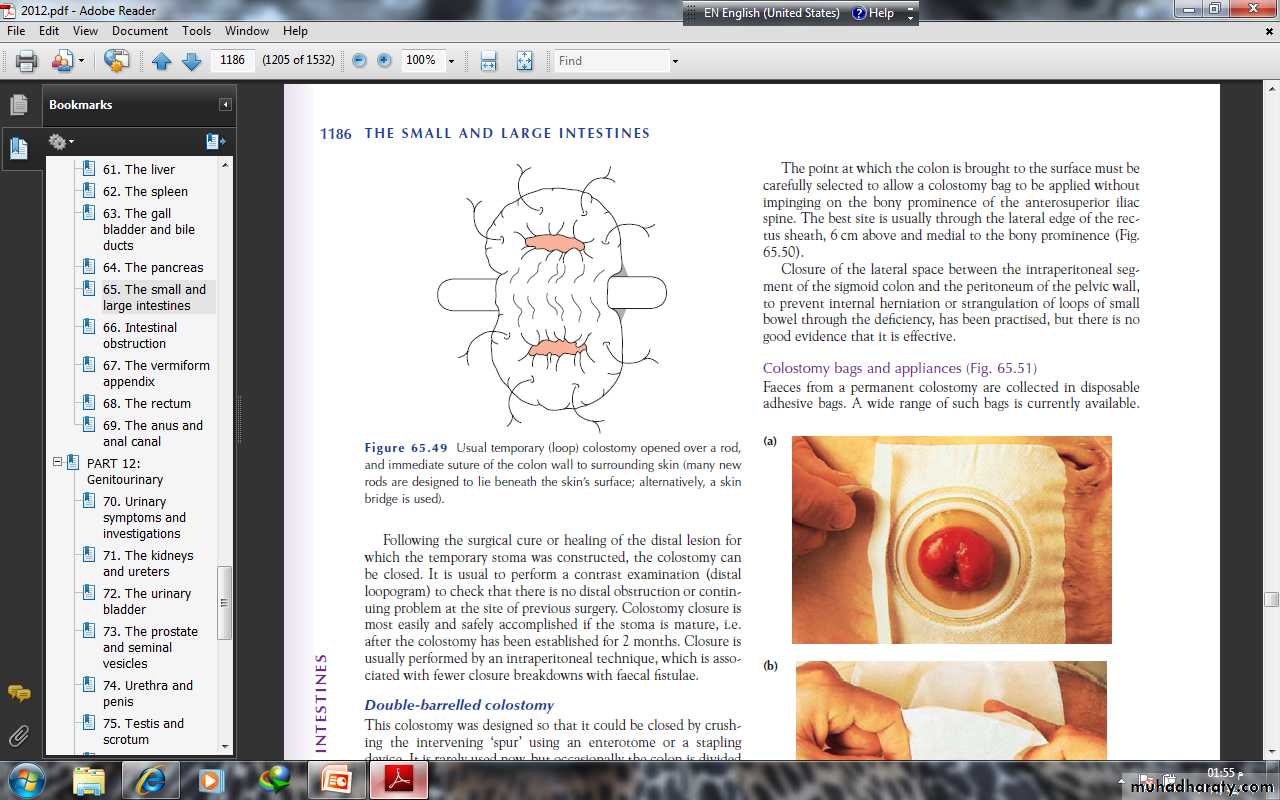
A temporary loop colostomy is made, bringing a loop of colonto the surface, where it is held in place by a plastic bridge passedthrough the mesentery. Once the abdomen has been closed, thecolostomy is opened. When firm adhesion of the colostomy to the abdominal wall has taken place, the bridge can be removed after 7 days. Colostomy closure is most easily and safely accomplished if the stoma is mature, i.e. after the colostomy has been established for 2 months.
Permanent colostomyThis is usually formed after excision of the rectum for a carcinomaby the abdominoperineal technique. it is formed by bringing the distal end (end-colostomy) of the divided colon to the surface in the left iliac fossa .
The point at which the colon is brought to the surface must becarefully selected to allow a colostomy bag to be applied withoutimpinging on the bony prominence of the anterosuperior iliacspine. The best site is usually through the lateral edge of the rectussheath, 6 cm above and medial to the bony prominence.
Colostomy bags and appliances Faeces from a permanent colostomy are collected in disposableadhesive bags. A wide range of such bags is currently available. Many now incorporate a stomahesive backing, which can be leftin place for several days. In most hospitals, a stoma care service isavailable to offer advice to patients, to acquaint them with thelatest appliances and to provide the appropriate psychologicaland practical help.
Complications of colostomiesThe following complications can occur to any colostomy but aremore common after poor technique or siting of the stoma:• prolapse;• retraction;• necrosis of the distal end;• fistula formation;• stenosis of the orifice;• colostomy hernia;• bleeding (usually from granulomas around the margin of thecolostomy);• colostomy ‘diarrhoea’: this is usually an infective enteritis andwill respond to oral metronidazole 200 mg three times daily.