Poliomyelitis
Poliomyelitis
ETIOLOGY.The polioviruses are positive-stranded RNA viruses, and include 3 serotypes (types 1, 2, and 3).
EPIDEMIOLOGY & Transmission :
*Poor sanitation and crowding have permitted the continued transmission of poliovirus in certain poor countries .
*Humans are the only known reservoir for the polioviruses, which are spread by the fecal-oral route. Poliovirus has been isolated from feces for >2 wk before paralysis to several weeks after the onset of symptoms.
Rarely paralytic poliomyelitis result from oral polio vaccine(OPV) which called vaccine-associated paralytic poliomyelitis (VAPP) .
Infants acquire immunity transplacentally from their mothers which disappear during the 1st 4–6 mo. of life.
*Active immunity after natural infection is lifelong but protects against the infecting serotype only; infections with other serotypes are possible.
PATHOGENESIS :
polioviruses enter the body via the gastrointestinal tract. The primary site of replication is in the M cells lining the mucosa of the small intestine.Regional lymph nodes are infected & the virus seeds multiple sites, including the reticuloendothelial system, and skeletal muscle.
The virus accesses the CNS along peripheral nerves . Its primarily infects motor neuron cells in the spinal cord (the anterior horn cells) and the medulla oblongata (the cranial nerve nuclei).
Clinical manifestations
The incubation period 8–12 days. Poliovirus infections may follow 1 of several courses:
1- inapparent infection :which occurs in 90–95% of cases and causes no disease and no sequelae but induce protective immunity.
2-Abortive Poliomyelitis(minor illness) :
Fever, anorexia, and headache are prominent features, and there may be sore throat and abdominal or muscular pain.The illness lasting 2–3 days. The physical examination may be normal. Recovery is complete, and no neurologic sequelae develop.
3-Nonparalytic Poliomyelitis(major illness) :
There is more intense headache, nausea, and vomiting, and stiffness of neck, trunk, and limbs(symptoms like aseptic meningitis).Physical examination reveals nuchal and spinal rigidity. In the infants, the anterior fontanel may be tense or bulging . Its either improve over 7-10days or proceed into paralysis within 2-3days . Most paralytic polio. pass through major illness .
4-Paralytic Poliomyelitis :
It develops in about 0.1% of persons infected with poliovirus, causing 3 clinically recognizable syndromes:
*Spinal paralytic poliomyelitis: . Severe headache, fever, muscle pain are present, with paresthesia, and spasms.
Within 1–2 days, asymmetric flaccid paralysis occurs.
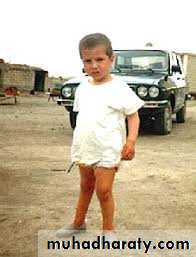
Involvement of 1 leg is most common . There is also muscle tenderness, & absent or diminished reflexes .Bowel and bladder dysfunction with constipation and urinary retention often occur.
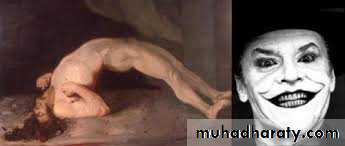
Sensation is intact . Atrophy of the limb, and deformity is common.*Bulbar poliomyelitis : clinical findings occurs due to dysfunctions of the cranial nerves and medullary centers .
*Polioencephalitis: a rare form of the disease in which higher centers of the brain are severely involved.
DIAGNOSIS:
1- Isolation and identification of poliovirus in the stool . 2 stool specimens should be collected 24–48 hr apart .2- CSF : The cells in the CSF may be polymorphonuclear early during the course of the disease but then shift to mononuclear cells .The CSF protein is normal or only slightly elevated .
3- Serologic test : to detect the IgM and IgG antibodies.
Differential Diagnosis :
Poliomyelitis should be differentiated from other causes of acute flaccid paralysis in children :1- Guillain-Barré syndrome : the paralysis is characteristically symmetric and sensory changes are common . There are few cells but an elevated protein level in the CSF.
2- Transverse myelitis: causing an acute symmetric paralysis of the lower limbs with concomitant anesthesia ,diminished sensory perception. The CSF is normal .
3- Traumatic neuritis: as Intramuscular gluteal injection. Paralysis occurs from a few hours to a few days after the traumatic event, is asymmetric, acute, and affects only 1 limb.
4- Pseudoparalysis : include unrecognized trauma, acute osteomyelitis, acute rheumatic fever, and viral myositis .
Complications of Paralytic poliomyelitis
1- Acute gastric dilatation .2- single or multiple superficial intestinal erosions.
3- Hypertension
4- Hypercalcemia, nephrocalcinosis & renal stone .
5- Cardiac irregularities & myocarditis .
TREATMENT :
no specific antiviral treatment for poliomyelitis .*All intramuscular injections and surgical procedures are contraindicated during the acute phase of the illness because these may result in progression of disease.
Paralytic Poliomyelitis :
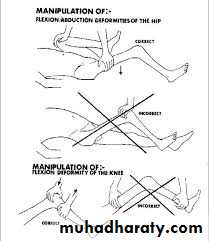
1- Hospitalization with complete physical rest in 1st 2–3 weeks .2- A neutral position with the feet at a right angle to the legs, knees slightly flexed, and hips and spine straight is achieved by use of boards.
3- Physiotherapy with active and passive movements.
4- hot packs relieve muscle pain and spasm.5- Adequate dietary and fluid intake .
* Factors increased risk for paralytic poliomyelitis :
1-Pregnancy .2- Tonsillectomy enhance the risk for acquisition of bulbar disease .
3- Intramuscular injections .4- Increased physical activity, exercise, and fatigue.
PREVENTION :
1- Hygienic measures.2- Immunization: 2 types of polio vaccine
*live-attenuated OPV (sabin).
*Inactivated polio vaccine (IPV) (salk)
Tetanus
ETIOLOGY.
Tetanus, also called lockjaw, is an acute, spastic paralytic illness caused by the neurotoxin (tetanospasmin or tetanus toxin) produced byClostridium tetani, gram-positive, spore-forming anaerobe whose naturally found in the soil, dust, and the alimentary tracts of various animals.
EPIDEMIOLOGY.
*The most common form, neonatal (or umbilical) tetanus. The neonate will get infection after cutting the umbilical cord by a non-sterile instrument. It occurs because the mother was not immunized.*maternal tetanus results from postpartum, or postsurgical wound infection with C. tetani in unimmunized women .
Most non-neonatal cases of tetanus are associated with a traumatic injury, or a penetrating wound by a dirty object.
PATHOGENESIS :
After introduction of spores into the injury site, they germinate & multiply. Toxin is released after vegetative bacterial cell death and lysis .This toxin binds at the neuromuscular junction and enters the motor nerve, next enters the spinal inhibitory interneurons, where it prevents release of the neurotransmitters γ-aminobutyric acid (GABA) , thus blocks the normal inhibition of antagonistic muscles & affected muscles sustain maximal contraction and cannot relax.
CLINICAL MANIFESTATIONS :
The incubation period typically is 2–14 days. Tetanus either generalized, which is more common, or localized1- Generalized tetanus:
The presenting symptom in 50% of cases is trismus (masseter muscle spasm, or lockjaw).
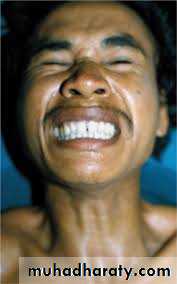
Headache, restlessness, and irritability are early symptoms, followed by stiffness, difficulty chewing, dysphagia, and neck muscle spasm.The so-called sardonic smile of tetanus (risus sardonicus) results from intractable spasms of facial and buccal muscles.
When the paralysis extends to abdominal, lumbar, hip, and thigh muscles, the patient may assume an arched posture of extreme hyperextension of the body (opisthotonos), the typical boardlike rigidity of tetanus .
Laryngeal and respiratory muscle spasm can lead to airway obstruction.
The patient remains conscious, in extreme pain because tetanus toxin does not affect sensory nerves or cortical function .Tetanic seizure then develop. Sight, sound, or touch may trigger a tetanic seizure .
Fever, as high as 40°C, is common .
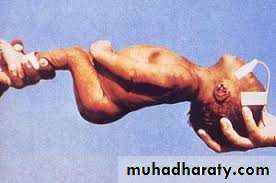
Tachycardia, dysrhythmias, & hypertension also may occur.2- Neonatal tetanus (tetanus neonatorum) :
The infantile form of generalized tetanus, typically manifests within 3–12 days of birth as progressive difficulty in feeding (sucking and swallowing), associated hunger, and crying. Paralysis, rigidity to the touch, and spasms, with or without opisthotonos, are characteristic. The umbilical stump may hold remnants of dirt, clotted blood, or serum .3-Localized tetanus :
results in painful spasms of the muscles adjacent to the wound site and may precede generalized tetanus.4- Cephalic tetanus :
is a rare form of localized tetanus involving the bulbar musculature that occurs with wounds or foreign bodies in the head, nostrils, or face.DIAGNOSIS :
1- Clinically.2- leukocytosis result from a secondary bacterial infection of the wound.
3- The CSF is normal . Neither EEG nor EMG shows a characteristic pattern.
4- C. tetani is not always visible on Gram stain of wound material, and it is isolated in only about ⅓ of cases.COMPLICATIONS :
1- Aspiration of secretions and pneumonia.2- Seizures → rhabdomyolysis with myoglobinuria and renal failure, long bone or spinal fractures.
3- Pulmonary embolism, gastric ulceration .
4- Cardiac arrhythmias.TREATMENT :
1- Surgical wound excision and debridement.2- Tetanus immunoglobulin (TIG) should be given as soon as possible in order to neutralize toxin that diffuses from the wound into the circulation before the toxin can bind at distant muscle groups.
If TIG is unavailable, use human intravenous immunoglobulin (IVIG) or tetanus antitoxin (TAT) .
3- Antibiotics : Penicillin G (100,000 U/kg/day divided every 4–6 hr IV for 10–14 days) . Erythromycin and tetracycline (for persons >8 yr of age) are alternatives for penicillin-allergic patients.
4- Muscle relaxants. Diazepam provides both relaxation and seizure control .
5- Neuromuscular blocking agents such as pancuronium, which produce a general flaccid paralysis that is then managed by mechanical ventilation .6- α- and β- blocking agents for autonomic instability .
SUPPORTIVE CARE :
* The patient should be sedated and protected from all unnecessary sounds, sights, and touch.*Endotracheal intubation or tracheostomy require in severe cases .
*Cardiorespiratory monitoring, frequent suctioning, and maintenance of the fluid, electrolyte, and caloric needs .