Dr.Sumeya
ECTOPIC PREGNANCYObgectives
The lecture discuss the definition ,risk factors, diagnosis and lines of management of ectopic pregnancyDefinition:
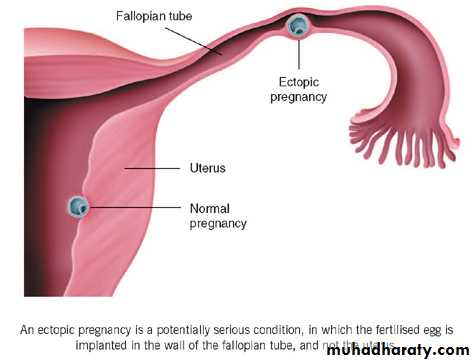
Implantation of coceptus outside uterine cavityIncidence; The incidence of ectopic pregnancy is11/1000pregnancies and the mortality rate is around10/100 000. Approximately 11 000 cases of ectopic pregnancies are diagnosed each year
• The rising incidence of ectopic pregnancy
• 1-early diagnosis of pregnancy can be made with the use of b-human chorionic gonadotrophin (bHCG)
• 2-ultrasound scans to identify the location of an early pregnancy
Heterotopic pregnancy
• is the simultaneous development of a pregnancy within and outside the uterine cavity. Although the incidence of a heterotopic pregnancy in the general population is low (1:25 000– 30 000), the incidence is significantly higher after in vitro fertilization (IVF) treatment (1 per cent).Common sites of implantation
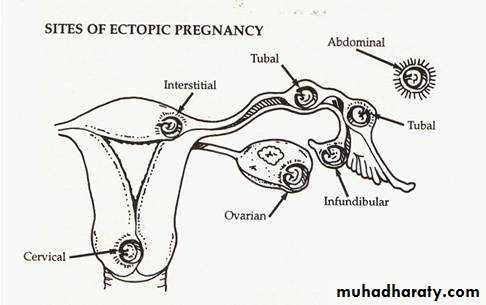
• Fallopian tubes (95 per cent)• ovaries (3 per cent)
• peritoneal cavity (1 percent).
In the Fallopian tubes, the distribution of sites
• the ampulla (74 per cent)
• isthmus (12 per cent)
• fimbrial end of the tube (12 per cent)
• interstitium (2 per cent).
• any mechanical or functional factors that prevent or interfere with the passage of the fertilized egg to the uterine cavity may be aetiological factors for an ectopic pregnancy.
Risk Factor for Ectopic Pregnancy
Previous PID – chlamydia infection 40%Previous ectopic pregnancy
Tubal ligation
Previous tubal surgery
Intrauterine device
THE OUTCOME OF ECTOPIC PREGNANCY
The muscle wall of the tube has not the capacity of uterine muscles for hypertrophy and distention and tubal pregnancy nearly always end in rupture or death.Tubal abortion – usually in ampullary about 8 weeks – forming pelvic haematocele
Rupture into the peritoneal cavity
Occur mainly from the narrow isthmus before 8 weeks or later from the interstitial portion of the tube. Haemorrhage is likely to be severe.
Sometimes rupture is extraperitoneal between the leaves of the broad ligament – Broad ligament haematoma.
• A high proportion of women with a tubal pregnancy miscarry during the early stages of gestation.
• The products of conception may persist for a considerable period of time within the tube as one form of 'chronic ectopic pregnancy', or they may be gradually absorbed.
•
Tubal pregnancy – effect on uterus
The uterus enlarge in first 3 months as if the implantation were normal, reach the size of a gravid uterus of the same maturity.• Uterine decidua grows abundantly(Arias-Stella reaction). and when the embryo dies bleeding occurs as the decidua degenerates due to effect of oestrogen withdrawal.
Clinical Finding:
Variable - Early diagnosis- location of the implantation
- Whether rupture has occurred
Classic symptom trait with unruptured ectopic pregnancy(subacute):
Amenorrhoea, abdominal pain, abnromal vagina bleeding(dark blood indicate old blood)
Classic signs – adnexal or cervical motion
tenderness.
With ruptured ectopic pregnancy(acute) finding parallel with the degree of internal bleeding and hypovolemia – abdominal guarding and rigidity, shoulder pain and fainting attacks and shock.
Pain – constant
- Cramp-likeIt may be referred to the shoulder if blood tracks to the diaphragm and stimulate the phernic nerve and it may be severe as to cause fainting.
The pain caused by the distension of the gravid tube by its effort to contract and expel the conceptus and by irritation of the peritoneum, by leakage of blood.
Vaginal bleeding – occur usually after death of the fetus and is an effect of oestrogen withdrawal. It is dark, scanty and its irregularity may lead the patient to confuse it with the menstrual flow and give misleading history.
25% of cases presents without any vaginal bleeding
Internal blood loss – severe and rapid. The usual sign of collapse and shock and it is less common than the condition presenting by slow trickle of blood into the pelvic cavity.
Peritoneal irritation – muscle guarding
- frequency of micturation
- fever
Pelvic examination – extreme tenderness
- cystic mass may be felt
Abdominal - tenderness in one or other fossa.
General tenderness and resistance to palpation over whole abdomen.
Differential diagnosis:
• Salpingitis• Abortion
• Appendecitis
• Torsion of pedicle of ovarian cyst
• Rupture of corpus luteum or follicular cyst
• Perforation of peptic ulcer.
• Diagnosis:
• - Careful history about LMP its timing and appearance.• - Always think of tubal pregnancy women with lower abdomen pain in whom there is possibility of pregnancy should be regarded as having an ectopic until proved otherwise.
• - Pregnancy test nearly always be found by the time of clinical presentation.
•
Investigation
• • Observations: BP, pulse, temperature• • Laboratory investigations: Haemoglobin, group
and save (or crossmatch if patient is severely compromised)
• HCG :This hormone is a glycoprotein produced by the placenta. It has a half-life of up to 24 hours and peaks at around ten weeks. Pregnancy tests measure the b-subunit of HCG.
• A bHCG level of less than 5 mIU/mL is considered negative for pregnancy, and anything above 25 mIU/ mL is considered positive for pregnancy. In 85 per cent of pregnancies, the bHCG levels almost double every 48 hours in a normally developing pregnancy.
• In patients with ectopic pregnancies, the rise of bHCG is often suboptimal. However bHCG levels can vary widely in individuals and thus often multiple readings are required for comparison purposes.
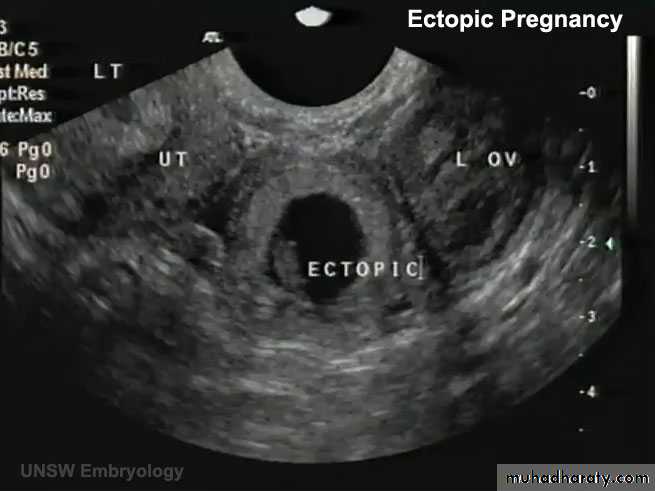
• Transvaginal ultrasound scan (TVS): An intrauterine gestational sac should be visualized at about 4.5 weeks of gestation. The corresponding bHCG at that gestation is around 1500 mIU/ mL. By the time a gestational sac with fetal heart pulsation is detected (at around 5 weeks gestation), bHCG level should be around 3000 mIU/mL.
Hence, the interpretation of bHCG must be done in context with the clinical picture and ultrasound findings.
Thus, if there were discrepancy between the bHCG concentrations and that seen on ultrasound scan (e.g. a high bHCG with no intrauterine pregnancy on ultrasound scan), the differential diagnosis of an ectopic pregnancymust be made.
Identification of an intrauterine pregnancy (gestation sac, yolk sac along with fetal pole) on TVS effectively excludes the possibilityof an ectopic pregnancy in most patients except in those patients with rare heterotopic pregnancy.
The presence of free fluid during TVS is suggestive of a ruptured ectopic pregnancy.
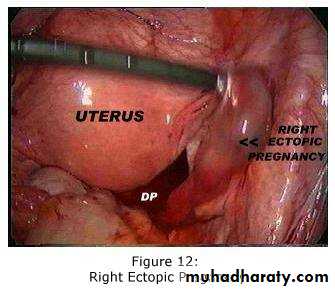
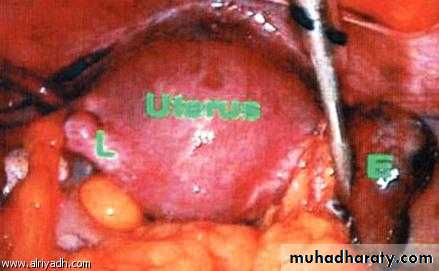
Laparoscopy: this can be used to diagnose and treat ectopic pregnancy.
Management
Ectopic pregnancy can be managed using an expectant, medical or a surgical approach, depending on clinical presentation and patient choice.Expectant
Expectant management is based on the assumption that a significant proportion of all tubal pregnancies will resolve through regression or a tubal abortion without any treatment.This option is suitable for patients who are haemodynamically stable and asymptomatic. This entails serial bHCG measurements and ultrasonography.
• If haemorrhage and shock present
• Restore blood volume by the transfusion of red cells or volume expander• Proceed with Laparotomy
Medical Managment
MethotrexateIndicationss:
Haemodynamically stable, no active bleeding, No haemoperitneum, minimal bleeding and no painNo contra indication to methotrexate
General anaesthesia poses a significant risk
cornual pregnancy;
patient with one Fallopian tube and fertility desired
treatment of ectopic pregnancy where trophoblast is adherent to bowel or blood vessel.
Medical treatment should be offered only if facilities are present for regular follow-up visits.
Systemic methotrexate is a treatment option for a carefully selected subgroup of patients.
Methotrexate, a folic acid antagonist, inhibits DNA synthesis in trophoblastic cells. It can be administered as a single intramuscular injection or in a multiple fixed dose regimen. .
Contraindications:
BreastfeedingImmunodeficiency / active infection
Chronic liver disease
Active pulmonary disease
Active peptic ulcer or colitis
Blood disorder
Hepatic, Renal or Haematological dysfunction
Side Effects:
Nausea & VomitingStomatitis
Diarrhea, abdominal pain
Photosensitivity skin reaction
Impaired liver function, reversible
Pneumonia
Severe neutropenia
Reversible alopecia
Haematosalpinx and haematoceles
Treatment failure and tubal rupture:
Significantly worsening abdominal pain, regardless of change in serum HCG (Check CBC)Haemodynamic instability
Level of HCG do not decline by at least 15% between Day 4 & 7 post treatment
or plateauing HCG level after first week of treatment
Follow-Up:
Repeat HCG on Day 5 post injection if <15 % decrease – consider repeat doseIf BHCG >15 recheck weekly until <25 ul/l
Surgery should also considered in all women presenting with pain in the first few days after methotrexate and careful clinical assessment is required. If these is significant doubt surgery is the safest option
• SURGICAL MANAGEMENT:
Surgical treatment can be by laparoscopy or laparotomy.Laparoscopic surgery is the mainstay of management
The laparoscopic approach offers significant advantage when compared to laparotomy as it results in
less blood loss,
shorter operating time,
less analgesia requirement,
a shorter hospital stay and a
shorter convalescence than laparotomy..
Laparotomy
Is mainly reserved forseverely compromised patients
The lack of endoscopic facilities
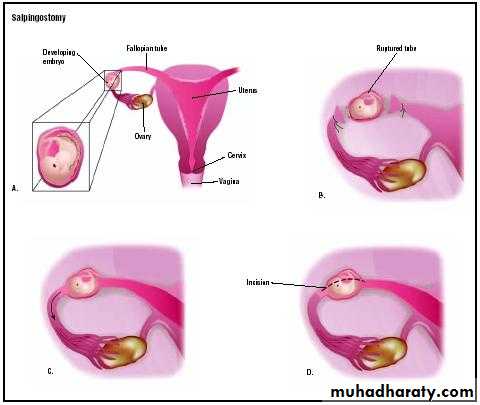
During surgery, the Fallopian tube can either be removed (salpingectomy) or
a small opening can be made at the site of the ectopic pregnancy and the trophoblastic tissue extracted via the opening (salpingotomy).
In general, if the patient has a normal remaining tube, salpingectomy is the treatment of choice.
Salpingotomy is thought to be associated with a higher rate of subsequent ectopic pregnancy.
1. Positive pregnancy test
Lowe abdominal pain +
Minimal Vaginal bleeding
Asymptomatic with factors
for ectopic pregnancy
Risk factors
Previous ectopic pregnancyPrevious PID
Tubal surgery
Tubal Surgery
Tubal pathology (PID, endometriosis
Infertility, ovarian stimulation
IUCD failure
Sterilization failure
Previous abdominal surgery
DES exposure in utero
Multiple sexual partners
2. History + clinical examination
MANAGEMENT OF ECTOPIC PREGNANCY
If sure of date of LMP and /or
Regular cycle, i.e.
>6 wks. gestation,
Arrange TV ultrasound
If unsure of date of LMP
and /or irregular cycle,
Measure serum hCG
If hCG <100
(?early Intrauterine/
? Ectopic pregnancy
If Hcg >1000, use
protocol for
suspected
Ectopic pregnancy
3. Empty uterus + free fluid in POD + adnexal + serum hCG > 1000
Meet criteria for
Methorexate treatmentDoes not meet criteria
for methotrexate treatment
Use methotrexate
protocol
Laproscopic /salpingotomy/
Salpingectomy ? OR Laparotomy if
haemodynamically unstable
In a woman of child bearing age with pelvi-abdominal pain and/ or vaginal bleeding …… ALWAYS….think
Ectopic Pregnancy