Disorders
ofPigmentation
By
Dr.Alaa A. Al-Sahlany
May 13, 2020
Causes of hypopigmentation
Infection: leprosy and pityriasis versicolorPostinflammmatory hypopigmentation: psoroiasis
Pityriasis alba: mild type of atopic dermatitisGenetic diseases: piebaldism, albinism
Chemical : rubberPharmacological: topical and intralesional steroids
Idiopathic: vitiligo
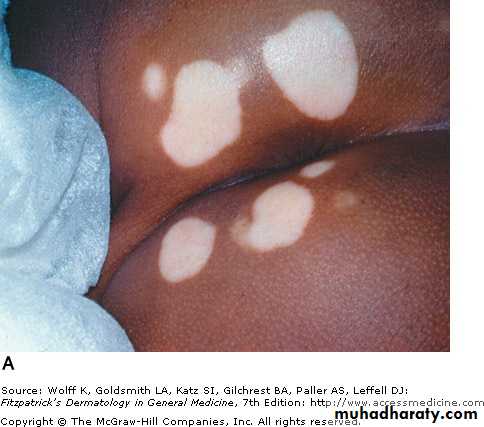
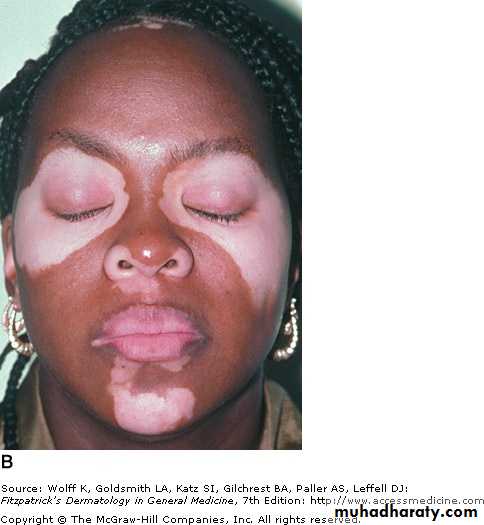
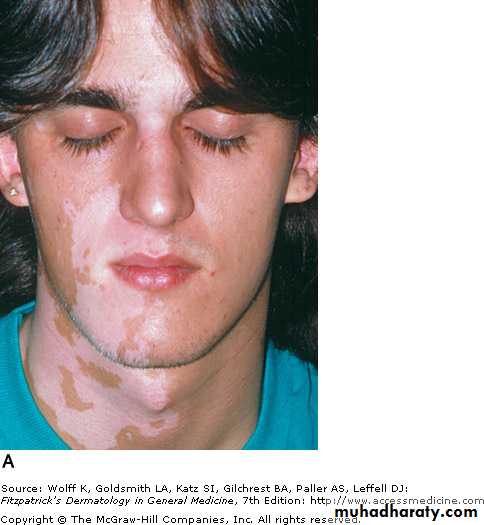
VitiligoIt affect 0.5-2% of general population worldwide
Average age of onset is 20 years but any age can be inflicted by this disease
Characterized by absence or decrease of melanocytes reflected by absence or decreased DOPA-positive melanocytesPathogenesis
Multifactorial: Genetic + EnvironmentalGenetic:
Susceptibility genes are AIS especially in vitiligo associated with autoimmune diseases
Environmental:
Autoimmune theory:
Humoral immunity: association with other auto-immune diseases in particular hypo and hyper thyroidism in addition to Addison’s , DM etc…
Cellular immunity: T cells that infiltrate perilesional epidermis are predominantly CD8 T cells
Intrinsic defects of melanocytes theory: dilatation in rough endoplasmic reticulum
Defective free radical defense: H2O2 overproduction in lesional skin lead to oxidative damage of melanocytes
Neural theory: especially in segmental vitiligo. They believe that neuropeptides released from nerve endings cause decreased melanin productio
Viral theory: Cytomegalovirus DNA has been identified in skin biopsy specimen of some patients with vitiligo, causing damage to melanocytes
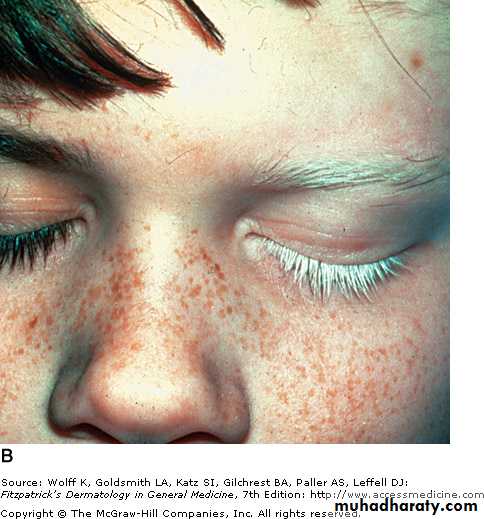
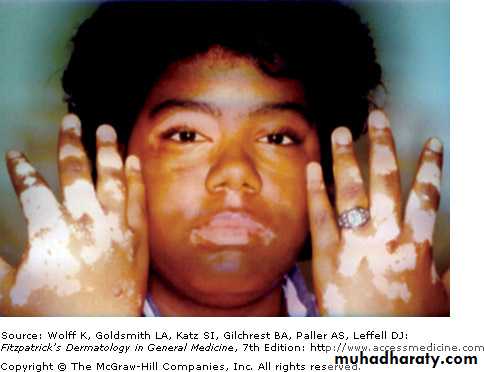
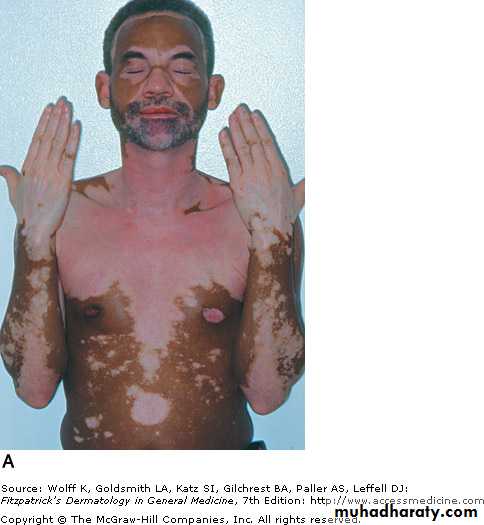
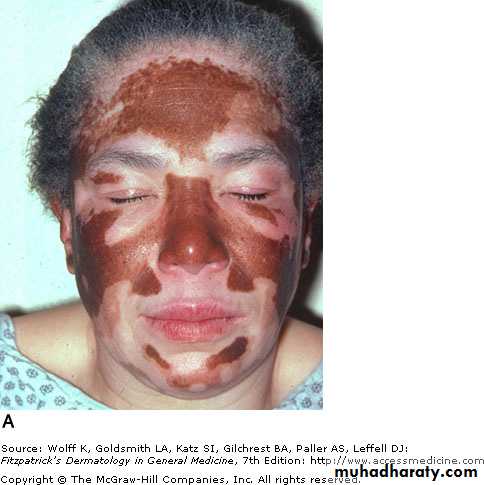
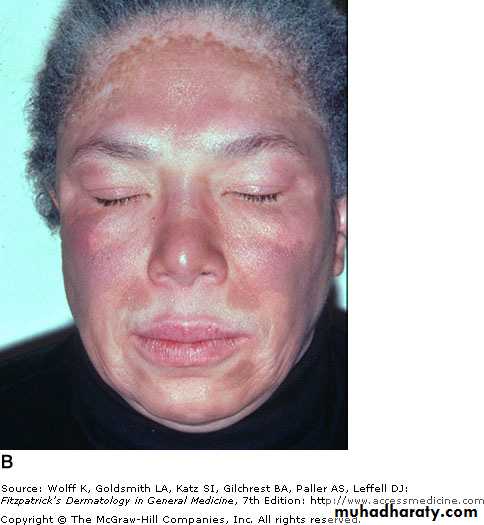
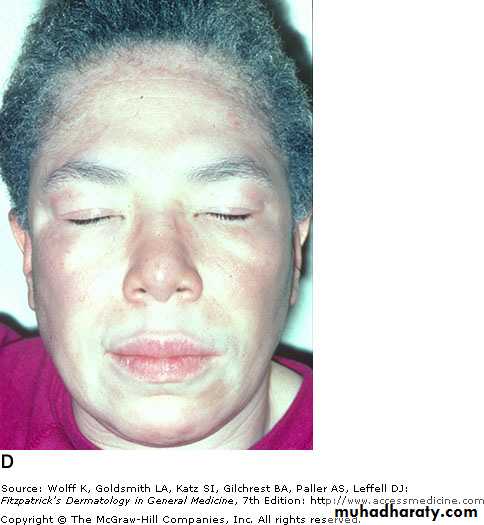
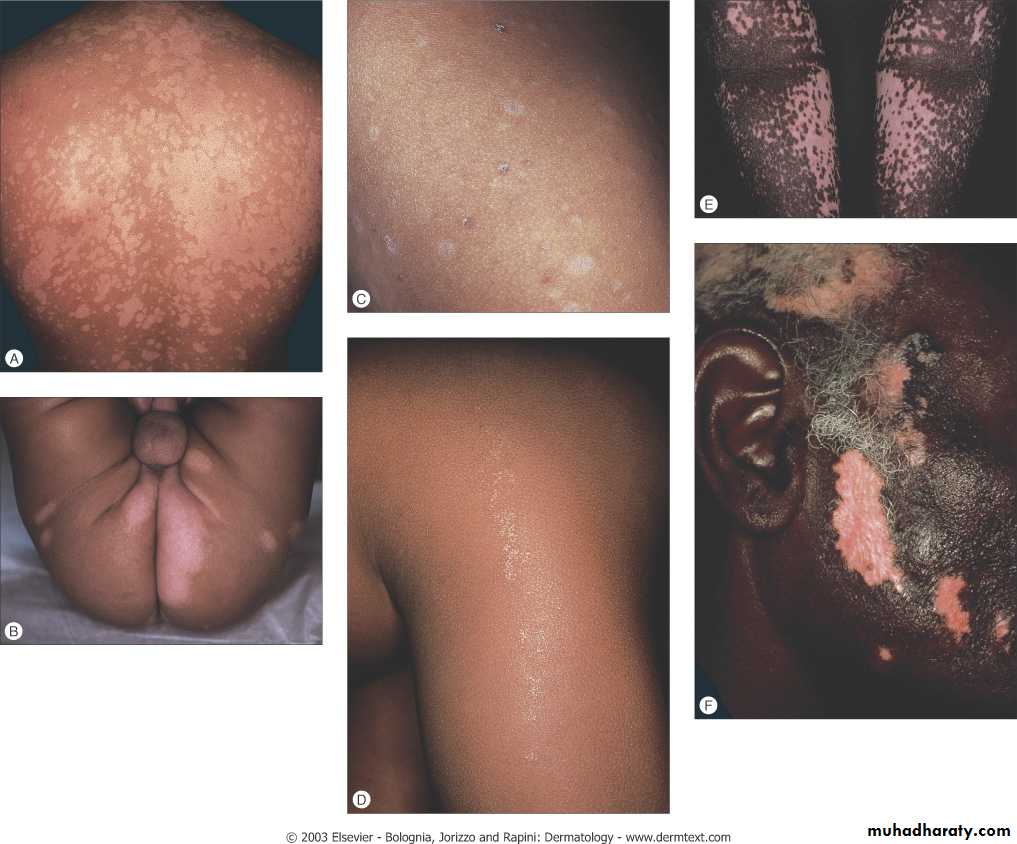
Clinical Presentation
Present as asymptomatic, non-scaly depigmented macules and patchesAffect face (periorificial), hands, knees, elbows, ankle, nipple, anogenial and and sacrum
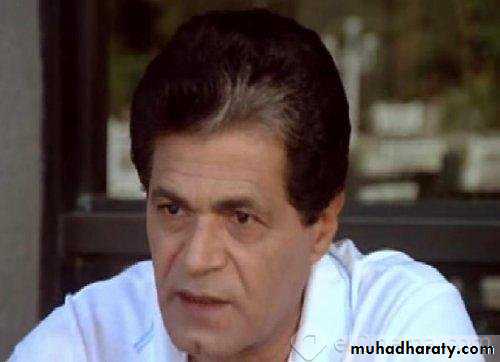
Can present as isolated localized patch of grey or white hair (poliosis) or as premature diffuse graying of hair ( canities)Classification
Localized:Unilateral(segmental): stop abruptly at the medline
Acrofacial: extremities and faceGeneralized:
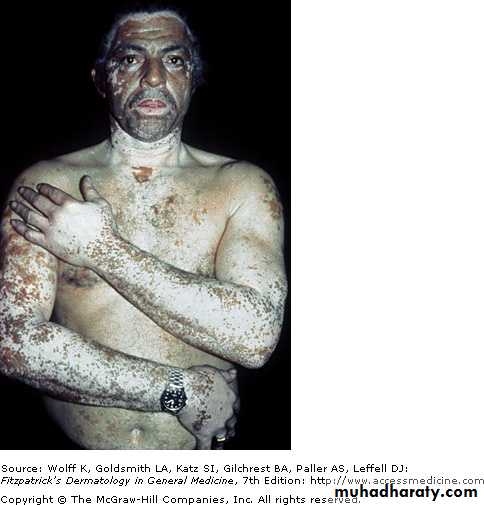
Universal: complete or nearly completeTreatment
If less than 20% of BSA is affected by vitiligo:Topical corticosteroids: first option
Topical immunosuppressant e.g. tacrolimus and topical pseudocatalaseSurgery: punch graft, suction blister graft, cultured melanocytes for vitiligo unresponsive to topical Rx
If more than 20% of BSA is affected by vitiligo:
Narrowband UVB(311 nm): first choice
Psoralen plus phototherapy(PUVA): psoralen can be applied topically(topical PUVA) or oral (oral PUVA) followed by exposure to artificial UV light or natural sunlight.
Excimer laser
Permanent depigmentation: e.g. monobenzyl ether of hydroquinone is used when vitiligo involve more than 50% of BSA and unresponsive to phototherapyOthers: systemic anti-oxidant, topical pseudocatalase
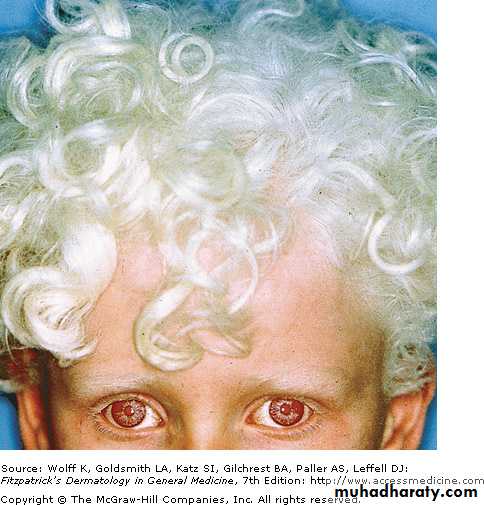
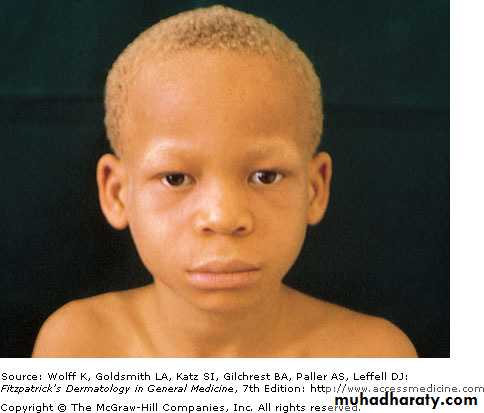
Oculocutaneous albinism
Autosomal recessive group of diseases characterized by diffuse pigmentary dilution due to partial or total absence of mealnin in skin, hair follicles and eyes despite the normal number of melanocytes in skinEyes may be affected by decreased visual acuity, nystagmus and photophobia
Those patient are at increased risk for skin cancerTreatment is photoprotection, photoprotection and photoprotection
Clinical featuresGene defect
Type of albinism
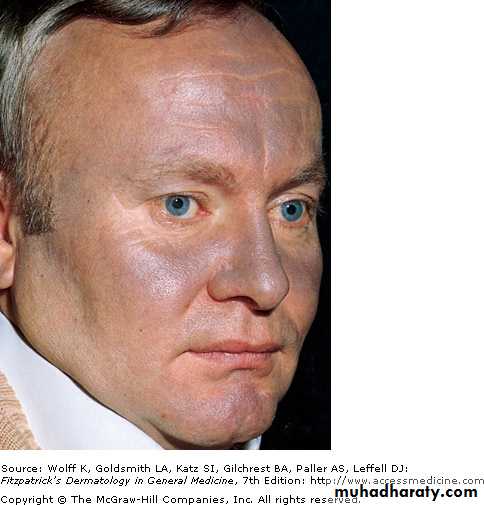
White skin, white hair and blue eyes (some are blind)
Develop some pigmentation of hair and skin with age (yellow OCA)
Tyrosinase(complete absence of activity)
Tyrosinase (Partial absence of activity)
OCA1AOCA1B
Skin and hair are light brown (brown OCA)OCA2
Bronze skin color , red hair (rufous albinism)OCA3
Decreased visual acuity, phtophobia and nystagmus. Skin is normalOA1
OCA1A
OCA1B
OCA2(BROWN)
Temperature-sensitive albinism
SCC in albinism patient
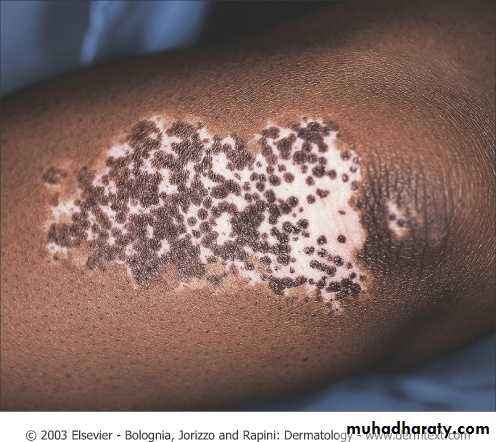
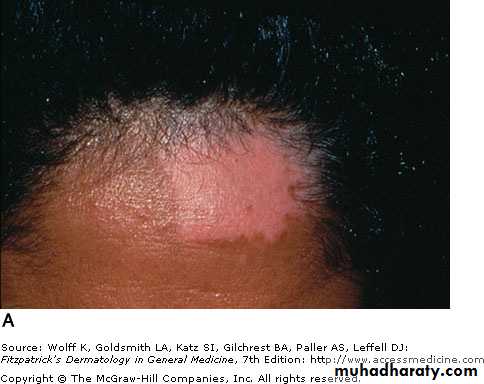
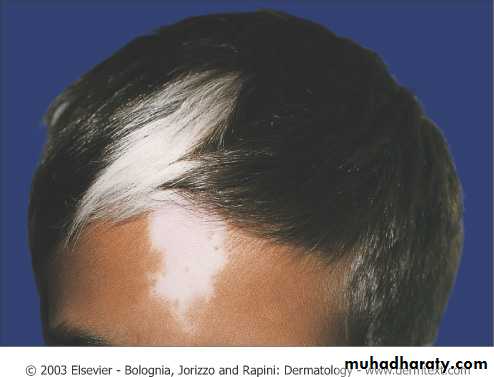
Piebaldism
Autosomal dominant, cc by stable depigmented patches on anterior trunk, mid extremities, central forehead and frontal scalp(white forelock), sparing the backPresent at birth
The involved skin has no melanocytes
Treatment: topical steroid and phototherapy is not effective. Auto graft from normal skin is successful
Causes of hyperpigmentation
Infection: Pityriasis versicolorFriction: macular amyloidosis
Drug-induced : amiodarone, silver, gold, minocyclinePostinflammatory hyperpigmentation: lichen planus and fixed drug eruption
Physical:erythema ab igne which is due to long-term exposure to heat e.g. laptop on the thighsIdiopathic: melasma
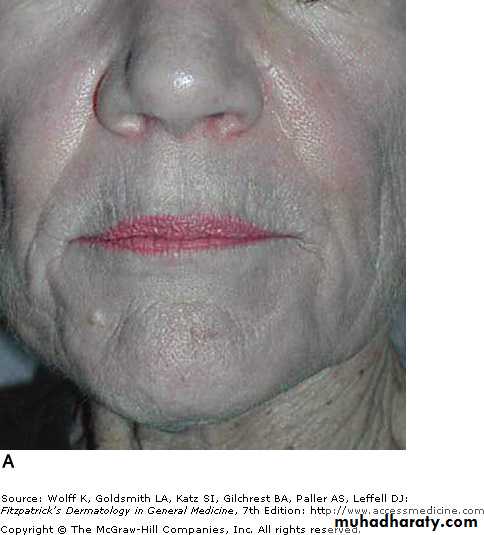
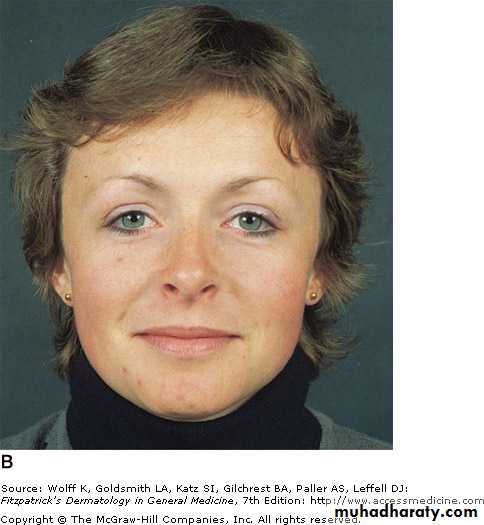
MelasmaSynonyms: chloasma, mask of pregnancy
It is most prevalent among young to middle aged women
Hispanic, Asian, African or middle eastern descent are inflicted by this diseasePathogenesis
Exposure to UV : fading of lesion in winter, involvement of sun-exposed areas and sparing of philtrum
Genetic/ethnic predisposition : Mostly it is related to darker skin type
Hormones: OCP, pregnancy (appearnace or exacerbation)Autoimmune thyroid diseases
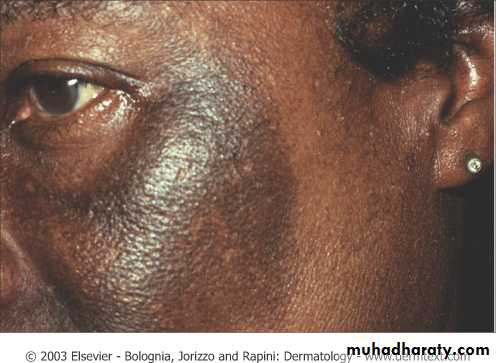
Clinical featuresBrown or gray patches on the face, but may affect extensor forearm and central upper chest
May lighten or disappear after delivery in light skinned women but may persist in dark skinned
Using Wood’s lamp, melasma is subdivided into epidermal( the lesion is accentuated), dermal (the lesion blend with the surrounding) and mixed
Treatment
Sun protection , sun protection and sun protection
Hydroquinonen( tyrosinase inhibitor). Side effects: allergic and irritant contact dermatitis, ochronosis
Kojic acid (tyrosinase inhibitor)
Azelaic acid (tyrosinase inhibitor)Others: Chemical peels e.g. using salicylic acid and glycolic acid, Laser, Dermabrasion
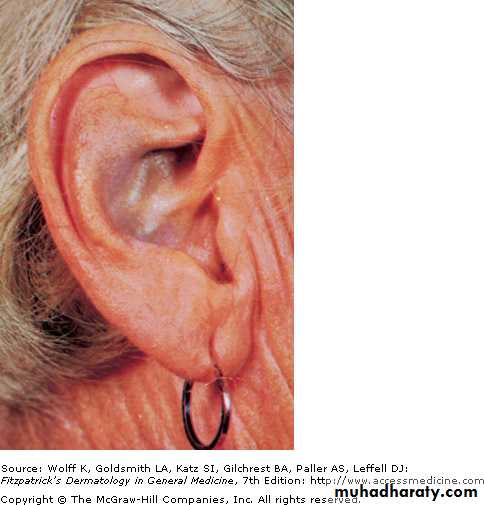
OchronosisThere are two types:
(1)Exogeneous: due to long-term application of hydroquinone, and products containing mercury, resorcinol and phenol
Rx: cessation of offending drug
(2) Endogeneous: due to defect in homogentisic acid oxidase. CC by deposition of pigment in cartilage of ear, nose and on sclera(osler sign) and by arithritis
Rx: low protein, low tyrosine and low pheylalanine diet
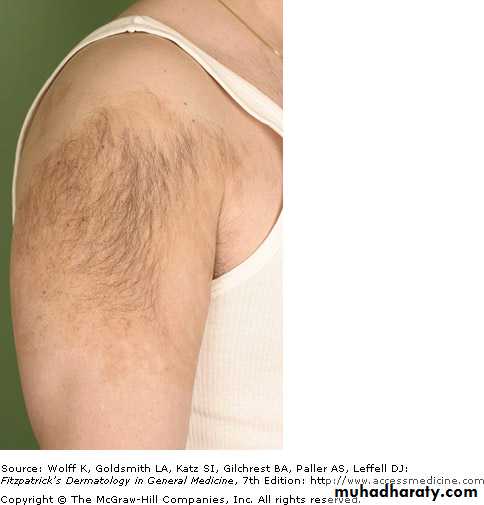
Macular amyloidosis
Pruritic confluent or rippled hyperpigmented macules and patchesMostly involve upper back and forearms
Women affected more than menlocal friction from nylon brushes, towels and other rough materials contributes to the production of this disease
Treatment: breaking itch-scratch cycle , stopping friction and use of topical steroids plus keratolytics
Drug Reactions
EpidemiologyThe skin is one of the most common targets for adverse drug reactions
women are more susceptible than men
Paradoxically, the incidence of most immunologically mediated drug eruptions is increased in the setting of immunosuppression; for example, in patients with AIDS
The incidence of adverse reactions also increases with the age of the patient
PathogenesisExample
The mechanism
IgE-mediated e.g. urticaria
1. Immunological mechanisms (unpredictable)
Phamacological side effects e.g. Chemothearapy cause hair loss that cannot be seperated from the desirable action of this drug2. Non-immunological mechanisms (predictable)
Stevens- Johnson syndrome/Toxic
epidermal necrolysis
3. Idiosyncratic (unpredictable and can not be explained on the basis of pharmacological properties of drug)
APPROACH TO DETERMINE THE CAUSE OF A DRUG ERUPTION
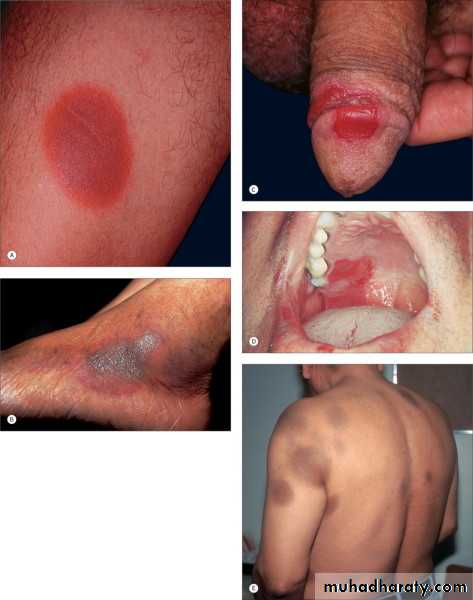
1. Clinical characteristics:Type of the lesion e.g. maculopapular lesions in morbilliform drug eruption ,
Distribution of lesions e.g. recurrence of the lesion at exactly the same site with each exposure to the same drug in fixed drug eruption ,
Mucous membrane involvement e.g. in SJS/TEN
Associated features such as fever, lymphadenopathy and visceral involement e.g. all are manifested in DRESS2. Chronological factors:
Document all drugs to which the patient has been exposed and the dates of administrationDate of eruption
Time interval between drug introduction and skin eruption because most of drug eruption occurs within 1-3 weeks after initiation of new drugResponse to removal of the suspected agent
Response to rechallenge(re-administration of drug) such as in fixed drug eruption which is not life-threatenening3. Literature search e.g medline
Note: Diagnostic or confirmatory test to identify the responsible drug is not available yetCausative drugs
Clinical manifestationType of drug reaction
Sulfonamides
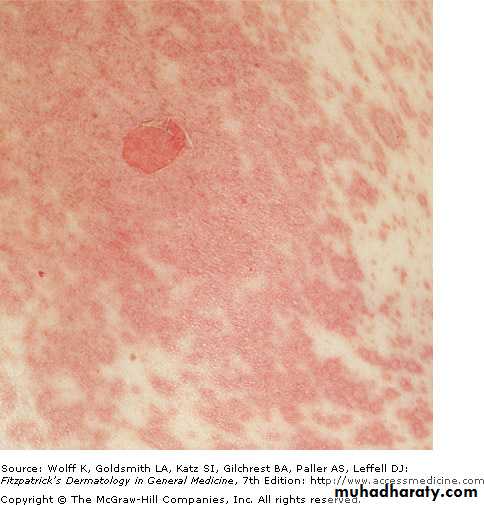
PenicillinCephalosporins
Macules and papules in symmetrical distribution which looks like a measle
Morbillliform eruption (the most common drug reaction)
PenicillinsCephalosporinsNSAIDsContrast media
Urticaria, angioedema and anaphylaxis
TMP-SMXNSAIDsTetracyclinesPseudoephedrine
Erythematous plaque with a dusky hue occur at the same site with every subsequent exposure to the same drug
Fixed drug eruption
AnticonvulsantsSulfonamidesAllopurinol
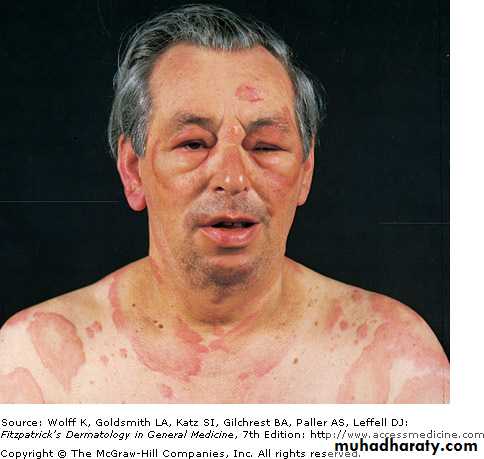
Morbilliform eruption, facial edema, fever, lymphadenopathy, visceral involvement in addition to peripheral eosinophilia
DRESS (drug reaction with eosinophilia and systemic symptoms) or hypersensitivity syndrome
AnticonvulsantsSulfonamidesAllopurinol
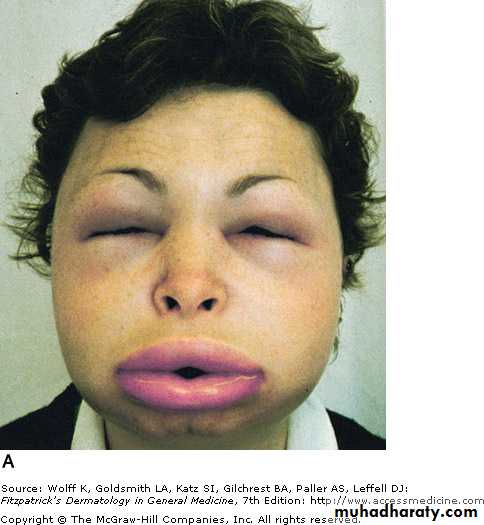
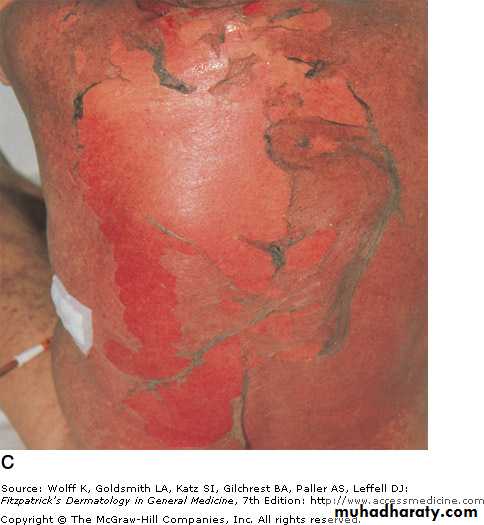
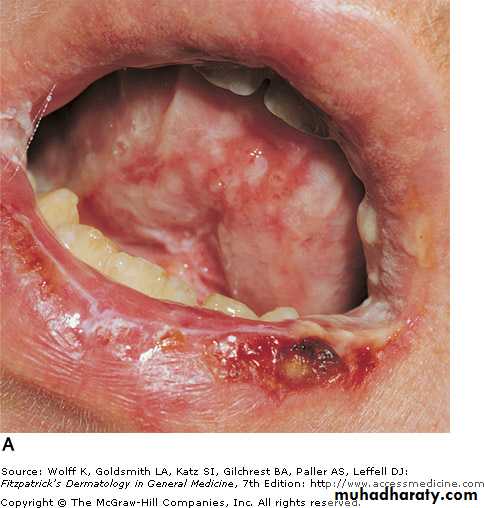
Morbillform eruption, severe mucous membrane invlovement e.g. mouth, eyes, genitalia and positive Nikolsky sign (sloughing of skin on pressure by finger)
SJS/TEN( Stevens-Johnson syndrome/ Toxic epidermal necrolysis)
Treatment
Withdrawal of suspect drug as soon as possibleIf many drugs are incriminated, stop all non-essential drugs
If the suspect drug is essential, substitute with another that does not cross-react
For mild drug eruption, start topical steroid and systemic antihistamines
For severe drug erupton such as SJS/TEN and DRESS, start systemic steroidThanks
ForWatching