Skin Tumors
ByDr. Alaa A. Al-Sahlany
May 17, 2020
Malignant Skin Tumors
Skin cancer is divided into:Non-melanoma skin cancer which is in turn subdivided into:
Basal cell carcinoma(BCC)
Squamous cell carcinoma(SCC)
Malignant melanoma
Basal cell carcinomaThe most common skin cancer in human
BCC occurs most frequently on the head and neck
Mortality from BCC is quite rare
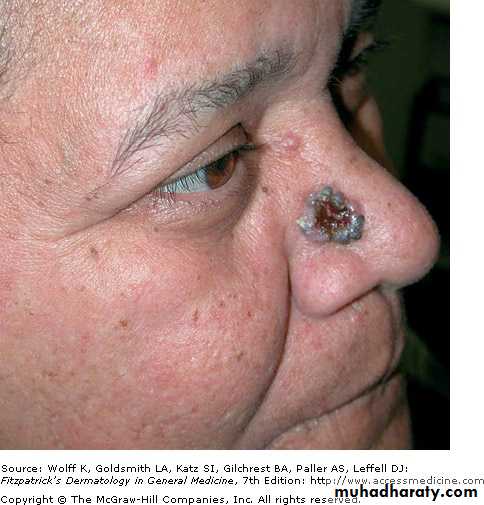
BCC typesNodular BCC: the most common type, translucent papule or nodule with telangiectasia , sometimes with a central depression or ulcer surrounded by a rolled edge
Superficial BCC
Morpheaform BCCCystic BCC
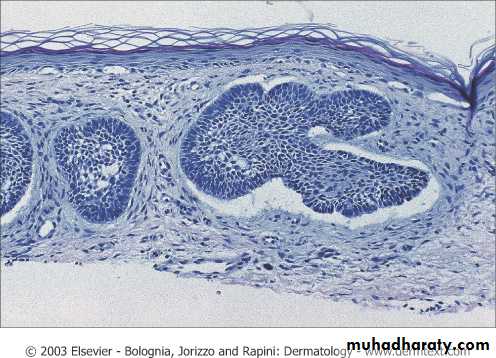
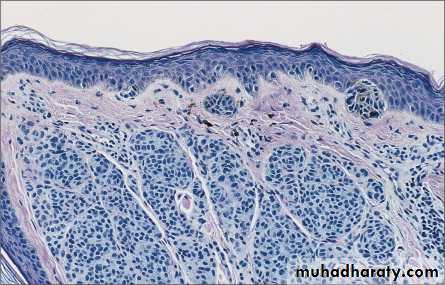
Palisading of cells at periphery
Retraction artefact(space between the stoma and cells)Mucin deposition
Squamous cell carcinoma
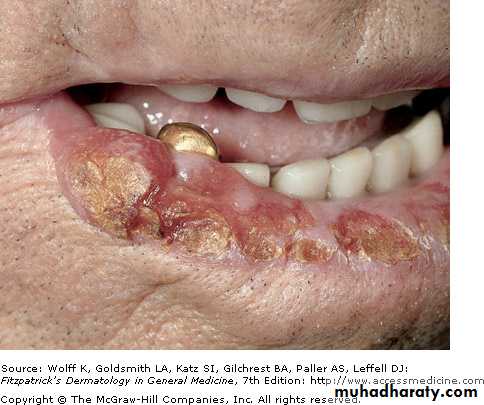
The majority of SCC occurring on the head, neck and upper extremities, present as erythematous scaly papule or noduleWhile melanoma among whites is responsible for 90% of skin cancer deaths before 50 years of age, in adults over 85 years of age, the majority of skin cancer deaths are attributable to SCC.
Risk factors of BCC and SCC
ImmunologicalGenetic
Environmental
Organ transplantation, HIV infection and immunosuppressive drugs: immunosuppression causes cancer due to (1) HPV infection and(2) immunosuppression
Xeroderma pigmentosum ( DNA repair defect) cause multiple SCC
Sun exposure
• Gorlin syndrome cause multiple BCC
Ionizing radiation• Chemical exposure : tar, polycyclic hydrocarbons, nitrogen mustard and arsenic
HPV infection cause SCCOther risk factor: thermal burns and chronic ulcers , scars (Marjolin's ulcer)
Treatment
Surgical excisionElectrodesiccation and curettage
Mohs Surgery: has the highest cure rate, used for high risk tumor and when tissue preservation is necessary e.g. digits, genitaliaMedical therapy : 5-fluorouracil
Radiotherapy: elderly patient unfit for surgeryCryotherapy(by freezing)
Photodynamic therapy( light plus photosensitizer)
BCC vs SCCSCC
BCC
Has a precancerous precursor(actinic keratosis)
Doesn’t have a precancerous precursor
Related to chronic cummulative sun exposure
Related to intermittent sun exposure
Can metastasize to lymph nodes and to internal organs and cause death
Doesnt metastasize but could be invasive
HPV can cause SCC
HPV cant cause BCC
More association with scar and chronic ulcer
Less association with scar and chronic ulcer
Malignant Melanoma(MM)
Is a malignant tumor arising from melanocytes. Its incidence and overall mortality rates have been rising in recent decades. Every hour , an American dies of melanomaDeath from melanoma occurs at a younger age than for other solid tumors
Melanoma incidence in Australia is the highest worldwide
Types of melanomaSuperficial spreading : the most common in fair-skinned persons, on leg of female and trunk of male
Nodular melanoma
Lentigo maligna melanomaAcral lentignious mel:occur on palm, sole and nail appratus, commonly occur in black and Asians
Amelnotic melanoma: doesn’t have any pigment
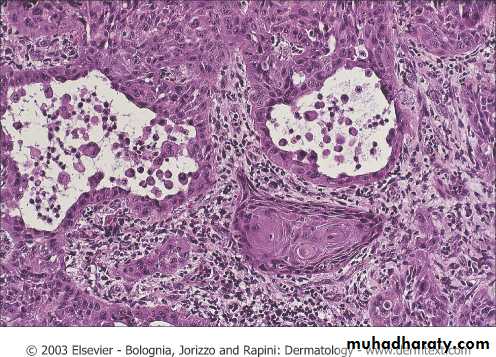
Pathology
Ill-circumscribedAsymmetrical
Loss of maturation
Single cells proliferation instead of nests
Cellular atypia(pleomorhism, high N/C ratio, prominent nucleoli, multiple mitotic figures)
Staging
Stage I: skin only( up to 2 mm thick)
Stage II: skin only(more than 2 mm thick)
Stage III: Regional lymph nodes metastasisStage: IV: non-regional LN metastasis, skin , subcutaneous and visceral metastasis
DiagnosisHx: family or personal Hx of MM, a Hx of childhood sunburn , HIV or organ transplant, , change in color size, shape, bleeding , ulceration, itching
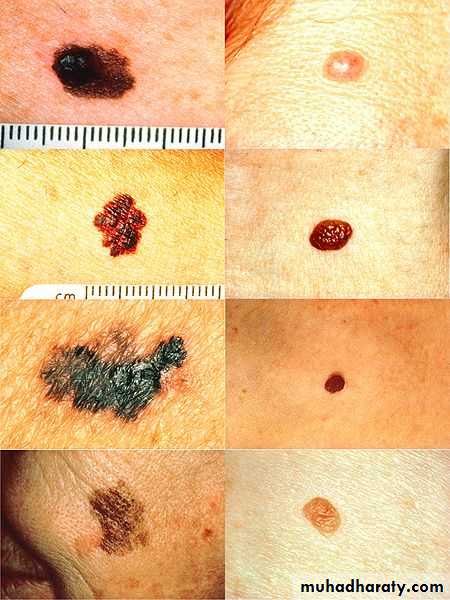
Examination: large no. of common nevi, presence atypical nevi which must have one of ABCDE ( A: asymmetry, B: irregular border, C: color variegation, D: diameter more than 6 mm, E: evolution)
Investigation:Excisional biopsy +/- Dermoscopy ,
Melanoma is immunogenic tumor given these facts:(1) incomplete or complete regression of melanoma ,
(2)occurrence of vitiligo-like depigmentation and halo nevi,
(3)a higher rate of melanoma in immunosuppressed patients
ABCDE
Treatment
Stage I/II : wide local excision of the lesion with safety marginStage III: Sentinel lymph node biopsy
Stage IV: Palliative Rx ( improve quality of life) which includes:RadioRx, chemoRx and immunoRx e.g. BCG, IL-2
Benign Skin Tumors
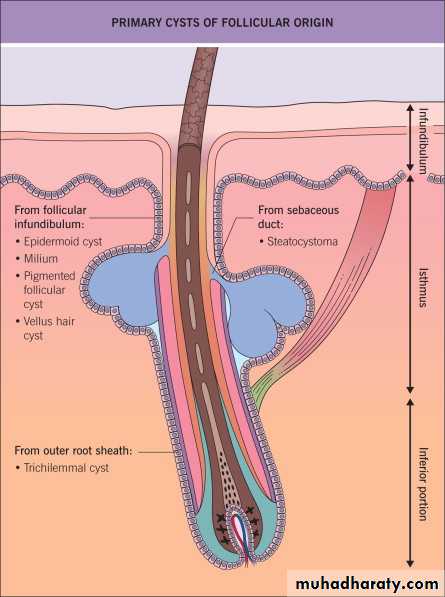
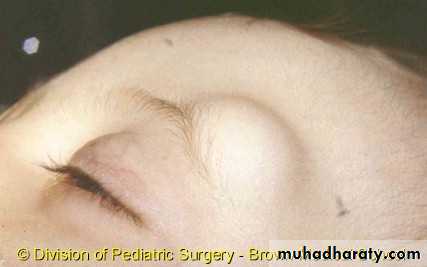
Epidermoid cyst
The most common cutaneous cystsMost common on the face and upper trunk
Present as a dermal nodules, may have a central punctum representing the follicle from which the cyst is derivedMultiple epidermoid cysts may occur in individuals with a history of significant acne vulgaris
They are asymptomatic, but, with pressure, cysts contents may be expressed that have a malodor
Rupture of the cyst wall can result in an intensely painful inflammatory reaction, and this is a common reason for presentation
Treatment: includes
Excision is curative.Inflamed epidermoid cysts may require incision and drainage +/_ systemic antibiotics
Milium
Are small epidermoid cystsPresent as 1–2 mm white to yellow papules
May occur as a primary, or secondary following blistering diseases or following cosmetic procedures e.g. dermabrasion or topical treatment e.g. steroidsTreatment: Most milia in newborns will resolve on their own
(1)Incising the overlying epidermis and expressing the milium(2)Electrodesiccation
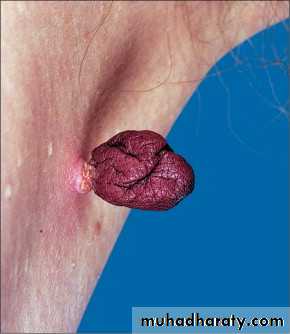
Skin Tag
Presents as a soft pedunculated papule, usually asymptomaticPredominantly on the neck, eyelid, axilla and groin
Their incidence increases with age and more commonly seen in obese individualsLarger lesions may be associated with diabetes mellitus
Treatment: simple scissor excision, electrodesiccation
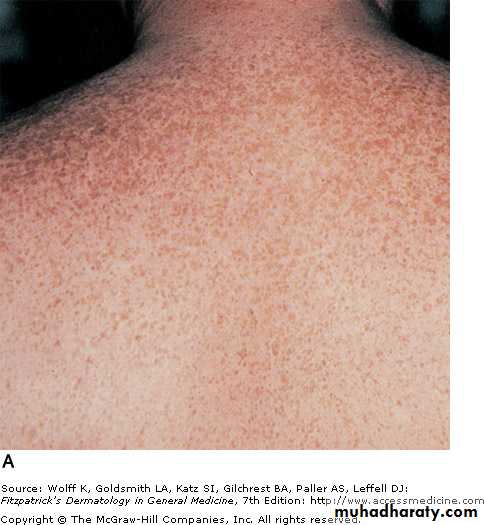
Actinic keratosis(AK)
Actinic keratoses (AK) are ‘premalignant’ and SCC would develop at a rate of 10-20%They present on sun-exposed skin of the head, neck, and extremities
Present as a rough erythematous papule with scale
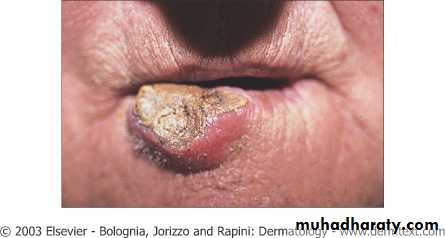
Actinic cheilitis : AK involving lower lip
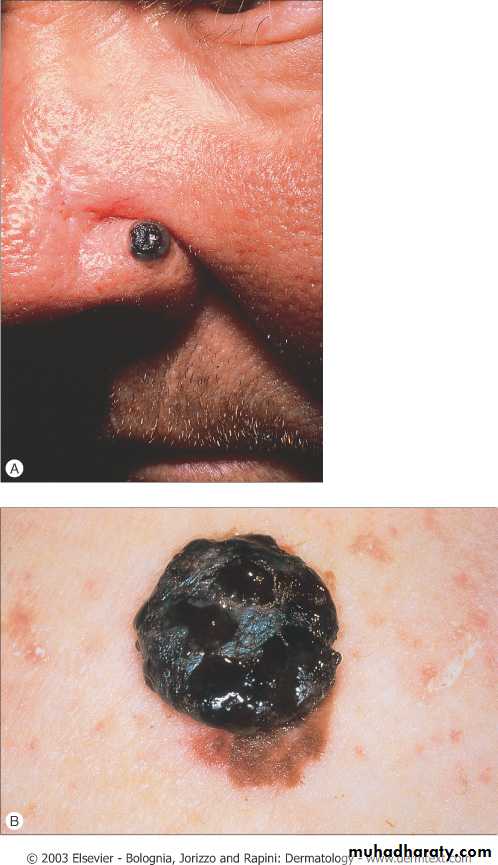
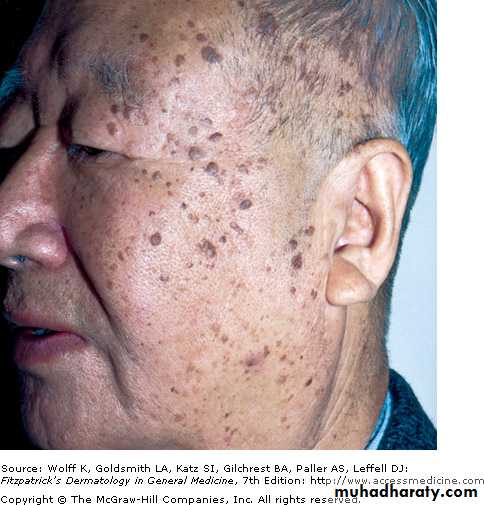
Seborrheic keratosis
Common in caucasian middle-aged individualsCan develop any where except mucosal surfaces and plams and soles
More commonly present as multiple, pigmented, sharply marginated lesions‘stuck-on’ appearanceUsually asymptomatic
Rx: curettage, cryotherapy, electrodesiccation, fractional laser.No risk of malignancy
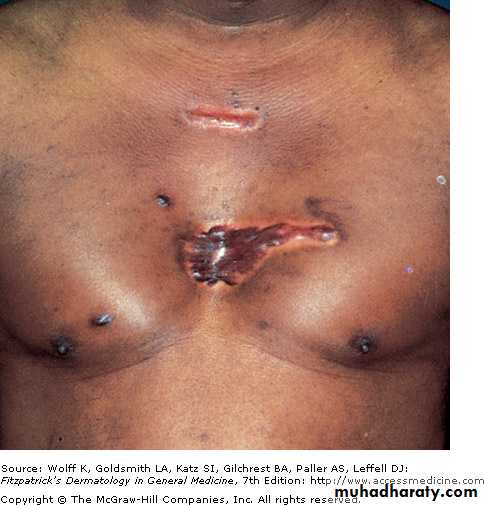
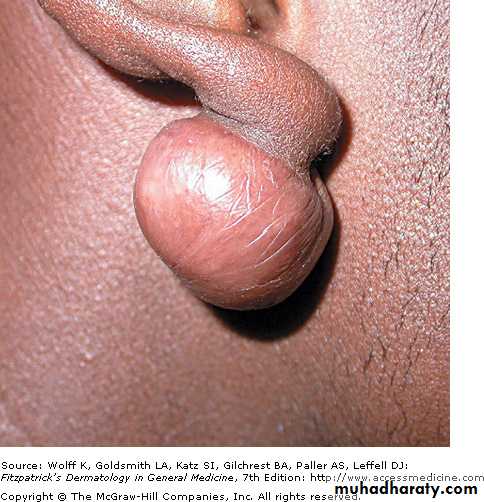
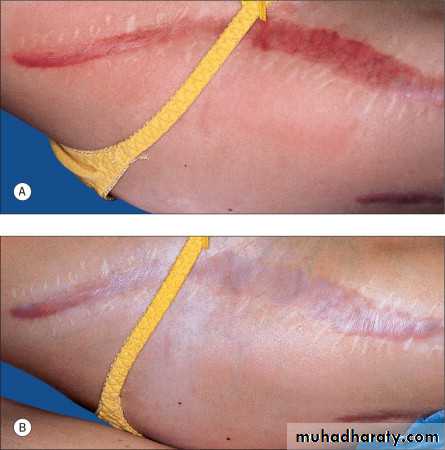
Hypertrophic scar and Keloid
Result from the uncontrolled synthesis and excessive deposition of collagen at sites of prior dermal injuryThey often occur after trauma e.g. laceration, burn, ear piercing, vaccination, or surgery or inflammation e.g. acne, or seldom spontaneously
More in darkly pigmented the skin
There is often a familial tendencyPresent as well-circumscribed pink to purple firm nodules or plaques which are painful or pruritic
Especially frequent on the earlobes, upper trunk, and the deltoid region (areas of high tension)
Melanocytes, Mast cells, Transforming growth factor-β (TGF-β) play a role in pathogenesis
Treatment: includes
Surgery, intralesional corticosteroids, intralesional 5-Fluorouracil, intralesional interferon, topical silicone gel sheeting and laser
Keloid
Hypertrophic ScarKey Features
Often(might be spontaneous)
Always
Preceded injury
No
Yes
Confned to wound margin
No
Yes
Spontaneous resolution
No
Yes
Contain myofibroblast
Poor
Good
Treatment Response
Acquired Melanocytic Nevus
A few nevi are present in early childhood, but they increase in number, reaching a peak in the third decade of life and tend to disappear with increasing ageCaucasians in general have greater numbers of nevi than do darker-skinned
Nevi on palms, soles, nail beds and eyes are more prevalent in blacks and Asians than in caucasians
One-third of melanomas are associated with nevi
An increased number of melanocytic nevi marks increased melanoma risk.Atypical nevus is characterized by ABCDE;
A: Asymmetry, B: Irregular Border, C: Variegated Color, D: Diameter more than 6 mm, E: Evolving which mean any change in color, size or shapeThere are three types:
Junctional nevi are a macules. Histologically present with nests of melanocytes at the junction between the epidermis and dermisCompound nevi with nests of melanocytes in both dermis and junction
Dermal nevi are papules with nests of melanocytes in dermisCongenital melanocytic nevus
Present at birthThree types; small (less than 1.5 cm in diameter), medium (1.5-19.9 cm) and giant (more than 20 cm)
There is a significant risk of development of melanoma of skin and meninges in giant nevus
Treatment:Small and medium: serial photography and annual follow-up
Giant: multiple staged excisions
Freckles vs Lentigines
Solar LentiginesFreckles (Ephelides)
Age of onset
Older age
Early childhood
Age of onset
Light and dark skin
Light skin with red or blond hair and blue eyes
Skin color
Persist for life
Fade with age
Duration
No seasonal variation
Darker in summer and lighter in winter
Relation to season
Larger
Smaller
Size