Disorders of Potassium metabolism
Potassium is an intracellular cation .About 98% is found in the intracellular Compartment , the remaining ( 2% ) is in the ECF
Plasma potassium level is a poor indicator of total body content.
The plasma level of potassium (3.5-5.3 meq/L) is critical due to the following effects:
Effects of Potassium
Neuromuscluar activitySo hypokalaemia →→→ Weakness, Hypotonia, Confusion.
Cardiac function
So Hypokalaemia →→→ Arrhythmias
Hyperkalaemia →→→ Cardiac arrest
Potassium enters and leaves the EC compartment by
1.The intestinePotassium is absorbed in the small intestine so hypokalaemia may develop in prolonged starvation diarrhea, fistula, and prolonged vomiting
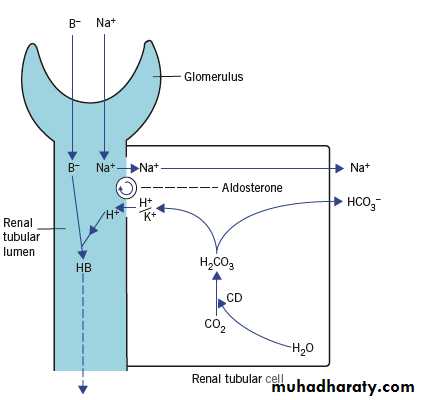
2.The tubules
Potassium is secreted in the DCT and CD in exchange for sodium. Hydrogen ions compete with potassium..
0
Potassium loss in urine depends on 3 factors
The amount of sodium available for exchangeAldosterone concentration , this is increased following fluid loss ,
(hyperkalaemia stimulates aldosterone release while hypokalaemia Inhibit It )
The relative amounts of hydrogen (H+) and potassium (K+) ions and the ability to secrete H+ in exchange with sodium (impaired in acetazolamide treatment ) and some type of renal tubular acidosis .
Potassium enters and leaves the EC compartment
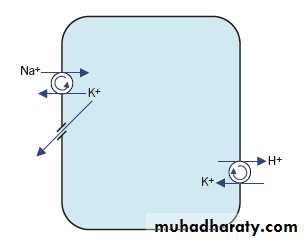
3.The cell membranes:Na+/K+- ATPase pump on cell surface maintains a high IC K+ content.
Three Na+ leave the cell and 2 K+ enter.
K+ also enters by exchange with H+.
The activity of the pump is impaired in hypoxia and ketoacidosis resulting in hyperkalaemia.
Conversely administration of insulin and glucose stimulate these pump.
Catecolamines have a similar action (This may cause hypokalaemia in MI).
Synthesis of pumps is stimulated by T4 so that there is hypokalaemia in hyperthyroidism.
potassium pump on cell membrane ) (
Relationship between hydrogen and potassium ions
There is a reciprocal relationship between K+ and H+. Consider the following:
In acidosis: H+ concentration is high in the ECF, so its pumping out of the cell in exchange with K+ is decreased , this leads to decrease the entry of potassium to all cells. In addition urinary secretion of potassium from the DCT (the 2 ions compete) is reduced. The 2 factors causes hyperkalaemia.
In alkalosis: The opposite situation is clear, there is net uptake of K+ into all cells with increased urinary loss leading to hypokalaemia.
The results are
Hypokalaemia is usually accompanied by metabolic alkalosis except some types of RTA, fistula, and CD inhibitor with which there is metabolic acidosis.
Hyperkalaemia is usually accompanied by metabolic acidosis.
Hypokalaemia
Levels less than 3.5 meq/L. The causes are:
A)- Renal causes :
-Increased Na+/K+ exchange:Primary hyperaldosteronism (Conns syndrome), secondary hyperaldosteronism, Cushings syndrome, steroid therapy, ectopic ACTH production, Bartters syndrome, Carbenoxolone therapy, and others
-Excess Na+ available for exchange: Infusion of saline, loop diuretics
-Decreased Na+/H+ exchange: Carbonat dehydratase inhibitors, renal tubular acidosis (type 1 & 2)-Impaired proximal tubular reabsorption: renal tubular dysfunction, Fanconi syndrome, hypomagnesaemia
.
b) Non-renal causes :
-Redistribution: Glucose and insulin, catecholamines, vitamine B12 therapy, certain rapidly growing tumors
-Intestinal loss: Prolonged vomiting, intestinal fistula, purgative abuse
-Reduced intake: Poor diet, IV fluid or parenteral nutrition
C)Combined causes: Alkalosis, pyloric stenosis
Hyperkalaemia
Serum potassium level more than 5.5 meq/L. Thecauses are
a)Renal causes :
-Insufficient Na+ exchange (ARF & CRF)
-Decreased Na+/K+ exchange: Hypoaldosteronism (Addisons diseases), 21-hydroxylase deficiency (CAH)
-Drugs: ACE inhibitors like captopril, potassium sparing diuretics (eg spironolactone)
.
b)Non-renal causes
-Pseudohyperkalaemia : due to in vitro haemolysis , leukocytosis, thrombocytosis , and delayed separation of plasma.
-Redistribution: Acidosis, hypoxia, sever tissue damage, in vivo haemolysis, and drugs like digoxin