
Disorders of pigmentation
Normal skin color is mixture of pigments (melanin, oxyhaemoglobin, and carotene ) , so abnormal
skin color may due to imbalance of these pigments.
Melanogenesis
Tyrosine, formed in the liver by hydroxylation of the essential amino acid phenylalanine under the
influence of phenylalanine hydroxylase, is the substrate for the reactions that occur in melanocytes . These
are the only cells in the epidermis to contain tyrosinase (dopa oxidase), the rate-limiting enzyme in
melanogenesis. This copper-dependent enzyme converts tyrosine to melanin. Dopa is formed by the
oxidation of tyrosine, and further enzymic action leads to the formation of dopaquinone. Eumelanins,
brown or black pigments, are then formed by polymerization. Phaeomelanins and trichochromes, the
pigments in red hair, are synthesized in a similar way, except that cysteine reacts with dopaquinone and is
incorporated into the subsequent polymers. Phaeomelanins and eumelanins may intermesh to form mixed
melanin polymers.
Classification of pigmentary disorder
Hypopigmentation due to decrease or complete loss of melanin.
Hyperpigmentation due to increase melanin production.
Hypopigmentation
Include
1 vitiligo
Definition:
Vitiligo is a specific, common, acquired disorder with a genetic predisposition characterized by
well-circumscribed milky-white macules devoid of identifiable melanocytes
.
Historic perspective:
د
.
و
ﺳ
ﺎ
م
ﻋ
ﻠ
ﻲ
ﻋ
ﻮ
ض
ﻟا
ﻤ
ﺤ
ﺎ
ﺿ
ﺮ
ة
ﻟا
ﺎﺜ
ﺜﻟ
ﺔ
The word vitiligo may be derived from the Greek vitelius , signifying a “ calf’s white patches
Incidence:-
Vitiligo can start at any age but in 50% of patients it develops before the age of 20 years .
In Iraq, the mean age of onset is 18 years, and in 66% of patients it develops before age of 20
years and also has been found to be common among children .
The distribution between sexes is equal . vitiligo affects all races and it is stated that it occurs in
1% of the world population,
Aetiology:
The genetic factors are undoubtedly involved but the inheritance pattern has not been fully
established.In Iraq, it was found that 25 percent of patients had a positive family history .
Pathogenesis:
The pathogenesis of vitiligo is not well understood. Many theories have been implicated in the
pathogenesis of the disease, and these include:-
I-The immune hypothesis:
This theory suggests an aberration of immune surveillance is destructive to melanocytes. Clinical
support for the immune hypothesis include the
presence of lymphocyte in the dermis of early lesions.
Decreased helper/suppressor ratio were also noted, particularly among patients with vitiligo of
less than a year .
Antityrosinase antibodies have been identified in patients with vitiligo.
II- The neural hypothesis:-
This proposed that from near- by nerve ending a neurochemical mediator is melonocytotoxic.
Support for this hypothesis is derived from numerous clinical observations: namely the appearance of
vitiligo sparing paralyzed limbs, vitiligo associated with viral encephalitis, and vitiligo with multiple
sclerosis . Onset of vitiligo following a period of emotional stress , pattern of segmental vitiligo are
also supportive observation. Increased Schwann cell basement membrane thickness was found in 75%
of dermal nerves.
III- The self-destruct hypothesis:-
Theorizes that certain tyrosine analogues and intermediates metabolites (dopa, dopachrome,,) in
melanin synthesis are known to be toxic to melanocytes. Melanocyte appear to have intrinsic
protective mechanism that eliminates toxic melanin precursors. Disruption of this labile mechanism
could permit accumulation of indoles and free radicals which destructed to melanocytes .
Clinical Features:-
The condition mainly starts as hypomelanotic macules , rarely itching in the absence of sun burn
may occur .The macules increase irregularly in size and fuse with neighboring lesions to form a large
areas, the condition is slowly progressive. The border of the lesion often being some what
hyperpigmented in lightly pigmented individuals, these white patches are first apparent in the summer
months where they fail to tan .
The depigmentation process passes through two stages of pigment loss:
Stage I (early lesions) appears as a light whitish brown color and this may stay for months before
it changes into a milky white color the so called stage II (late lesions)
Spontaneous repigmentation is noted in about 15-25% of patients, most frequently in sun-
exposed area, it is usually seen in younger patients, the repigmentation being quite trivial and mainly
perifollicular .The hair in the patches frequently remains normally pigmented, but in older lesions the
hair too are often amelanotic .
Types of Vitiligo:-
The following types represent the most characteristic patterns of vitiligo, namely,
generalized (type A).
segmental (type B).The differences between both as follow (table 1):-
Type A
Type B
Distribution
Nondermatoml
Dermatomal
Ratio
3
1
Onset
Any age(50%
before age20)
Young
Activity
Lifelong
Rapid spread 1 year
Associated with halo
nevus
Yes
No
Koebner’s phenomenon
Yes
No
Associated
with
immunologic diseases
Yes
No
Other forms:
-
Acro facial vitiligo: involves distal digits and periorficial areas.
-
Universal vitiligo (vitiligo universalis) describes such widespread vitiligo that there are few
remaining normal macules of pigmentation; this type has been associated with the multiple
endocrinopathy syndromes.
Other cutaneous abnormalities:
• Alopecia areata has been reported in up to 16% of vitiligo patients.

• Halo nevi appear relatively common
• Depigmented hairs are commonly found in isolated macules; leukotrichia (poliosis) has been
reported in 9 to 45 percent of vitiligo patients
• Ocular abnormalities: changes may be seen in the uveal and retinal pigment epithelium and this
can be detected by slit lamp examination .
• Otic Abnormalities: studies described familial vitiligo associated with auditory abnormalities .
Systemic Disease Associations:
Thyroid disease, particularly hyperthyroidism, hypothyroidism, Grave’s disease, toxic goiter and
thyroiditis
Diabetes mellitus: Rheumatoid arthriti
Pernicious anemia: Myasthenia gravis.
Auto-immune hemolytic anemia. Lymphoma
Lichen planus Psoriasis, and others,,
Histopathological findings
:
absence of melanocytes and melanin from the epidermis, either partial in early lesion, or complete in
late lesions.
Diagnosis:
-Clinically It’s easy to recognize the condition in-patients with progressive, chalk-white, macules in
typical sites. But some need further examination to confirm the diagnosis. For example:
- Histopathological study
-Wood’s lamp will accentuate the hypopigmented area, fluorescence ivory colored. Total body wood’s
light examination is needed for those with skin type I to III.
Treatment
General treatment
:
spontaneous resolution will occur in the 15-25% of the patients.
Emotional support and reassurance.
Patients should be encouraged to use sunscreens to protect the vitiliginous
Medical treatment
I- Topical therapy
Topical 8- methoxypsoralens with UVA (PUVA) or 8- methoxypsoralens with sun light
(PUVA SOL)
Topical steroid.
Topical tacrolimus (on the face ).
Topical iodine tincture 5%
Fluorouracil 5% cream: after dermabrading skin with a dermabrasion apparatus or sand paper. Topical
coal Tar.
Topical calcipotriol in vitiligo.
Topical lactic acid 15% therapy
Systemic therapy:
Systemic Psoralen-UVA.
Systemic PUVA sol.
Systemic Steroids .
UVA with phenylalanine .
Surgical treatment
Suction blister grafting.
Autologous minigrafting.
Transplantation of in vitro-cultured epidermis.
Other modalities
1-Narrow-band UVB.
2-Laser therapy with Excimer Laser.
Depigmentation therapy:
1 - Monobenzyl ether of hydroquinone.(Benoquin 20% , leukodenin 10%)
Use when surface area of vitiligo more than 50% of surface area.
2- Depigmentation with ruby laser

2 Post inflammatory hypopigmentation
Any skin disease after healing may give picture similar to the vitiligo which due to either absent or
damage in the melanocytes or dur to altered tyrosine metabolism or both but very good prognosis and
return to the normal color with time.
3 Pityriasis alba
Is a superficial dermatitis commonly occur in the children with peak age 6-8 years.
Clinically as hypopigmented but (not depigmented) ill demarcated patch commonly in sun exposed area.
Some time the lesion presented as well demarcated erythematous scaly patches .Treatment with topical
emollients with topical steroid.
4 Naevus depigmentosus ( achromic naevus)
This is a circumscribed area of depigmentation, usually present at birth and changing little
thereafter. The lesions are often single but may be multiple, circumscribed and either rounded,
dermatomal or in whorls and streaks . Histology may show either normal or reduced numbers of
melanocytes. A defect in transfer of melanosomes to keratinocytes has been postulated, at least in some
cases.
5 Post burn leukoderma
After 1st and 2nd degree burn.
6 Idiopathic guttate hypomelanosis ( leukopathia symmetrica progressive)
Is very common acquired disorder that affected women than men , usually after age of forty.
Presented as very sharply defined irregular macular lesions. Mainly in the forearm and face .
7 Steroid leukoderma
Condition mainly occur after interarticular injuction of steroid, but less commnly after intradermal
injuction and rarely after topical steroid.
8 Albinism
Is heterogenous group of disease usually autosomal recessive characterized with loss of skin , hair,
eye pigments due to defect in the tyrosinase enzyme either totally lost or partially with noral number of
melanocytes.
Totally lost enzyme produce white-red skin with completely white hair while partial loss produce blond
hair with fur skin.
9 Piebaldism
Autosomal dominant disease with variable phenotype characterized by at birth white forelock
(
ﻟا
ﺎﻨ
ﺻ
ﯿ
ﺔ
) , with patchy absence of skin pigment .
Commonly the lesion involve the anterior , posterior part of the trunk. The lesion remain static during
time with hyperpigmentied macules will develop within skin lesions, medial portion of eye brow is white.
Histopathology revealed absence of melanocytes
Hyperpigmention
Included
1 traumatic & frictional types
Most important example is perioral hyperpigmentation which is commnly found in the young
peoples . Other example include Lifa disease the disease commonly among the slim people and rarely in
the obese , more common in the female than male 12-15: 1 , so when the person use the Lifa will squeeze
the skin between the skin and bony prominences . the friction will increase melanocytes function and
melanin will droped in dermis cause dermal melanosis. Common site of involvement include clavicle,
upper chest, shin, shoulder.
2 Post inflammatory hyperpigmentation
As in healed lichen planus.
3 melasma
Is acommon acquired pigmentary skin disease characterized by brown hyperpigmention of the
face. The hperpigmented patches is quite sharply demarcated. Melasma of the face have different clinical
pattern.
Included:
1 butter fly pattern (50%).
2 mask like patter (35%).
3 localized pattern to the local area of the face(10%).
4 horse show like pattern (5%).
Melasma can involve other site other than face, included as nipple, genital area, or forearm.
Etiology:
1 UV radition 90% of the cases.
2 Pregnancy and hormonal treatment OCP 50%-75%.
3 family history 25%
4 stress 60%
5 topical cosmetics
6 drugs such as antiepileptic agents.
7 Idiopathic (commonly in the male).
Types of the melasma according woods light examination
1 epidermal type in which there intensifying of the pigmentation with woods light.
2 dermal type type in which there is no enhancement of the pigment with woods light.
3 mixed type ( both feature of epidermal & dermal)
4 woods light unapparent in the dark peoples.

HPx. Increase in the number and activity of melanocytes in the epidermis
Melanophage in the dermis.
Treatment
1 during pregnancy will improved after delivery , stop OCP
2 broad spectrum sun screen.
3 bleaching agents (hydroquinone 2%, 4%) alone or in combination with topical steroid and retinoid
4 other bleaching included (azelic acid, kojic acid)
5 chemical peel
6 laser thrapy.
4 Backer nevus
Commonly around the age of 15 but at birth can occur. As back-brown patches on trunk or limb ,
commonly in male than female 3:1 . 8% of the patients showed +ve family history.
65% of the patients showed hypertichosis of the lesion.
5 café- au late macule
As in neurofibromatosis , tuberous sclerosis, Fanconys syndrome, ataxic telangiectasis,,,,
HPx. showed increase basal layer pigmentation due to increase size of melanosomes with normal number
of melanocytes.
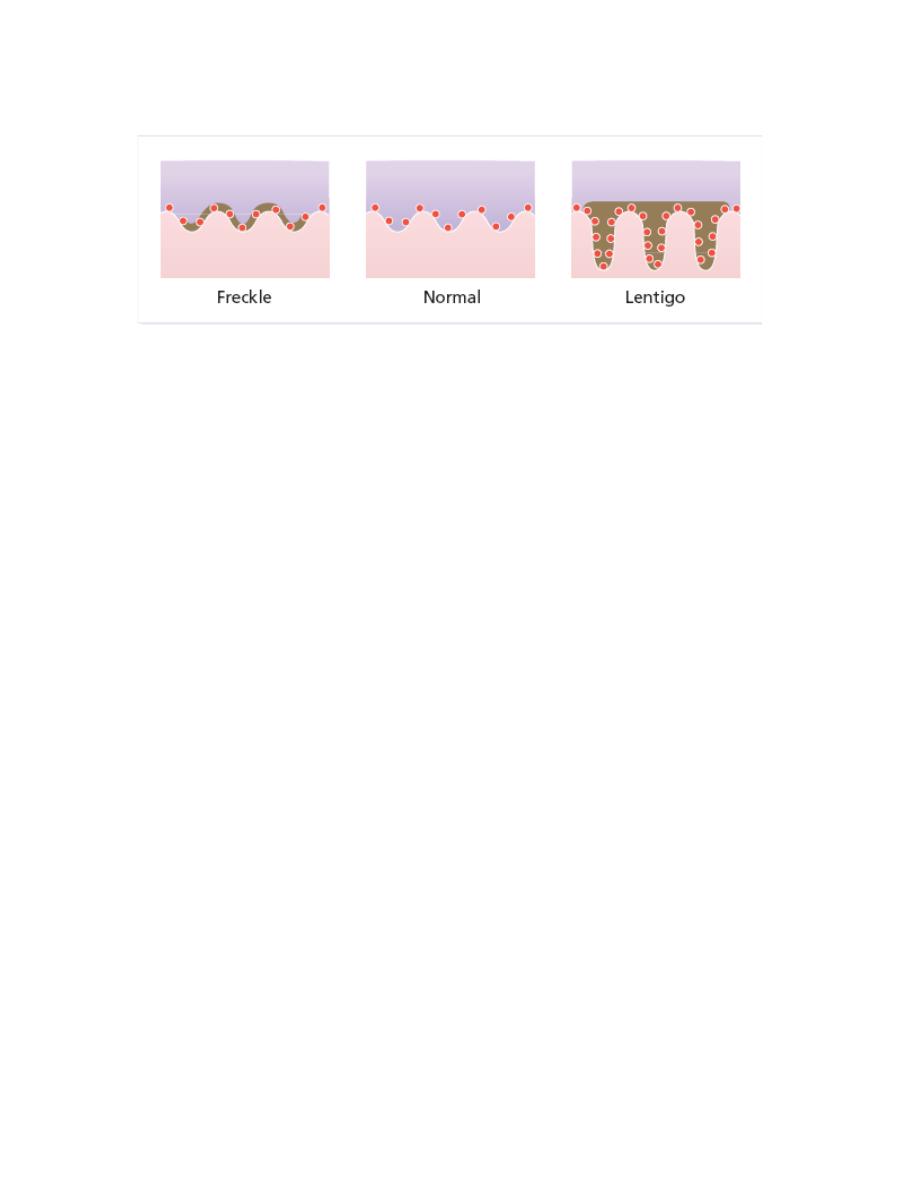
6 Freckles (ephelides)
They are seen most often in the redhaired or blond person as sharply demarcated light brown
macules, usually less than 5 mm in diameter. They multiply and become darker with sun exposure.
HPx
Increased melanin is seen in the basal layer of the epidermis without any increase in the number of
melanocytes, and without elongation of the rete ridges
7 Lentigo
Simple and senile lentigines look alike. They are light or dark brown macules, ranging from 1 mm
to 1 cm across. Although usually discrete, they may have an irregular outline. Simple lentigines arise most
often in childhood as a few scattered lesions, often on areas not exposed to sun, including the mucous
membranes. Senile or solar lentigines are common after middle age on the backs of the hands (liver
spots).
HPx.
In contrast to freckles, lentigines have increased numbers of melanocytes. With elongated of rete
pigs .
8 Phytophotodermatitis (Berloque dermatitis)
9 Xerodermapigmentosa
10 endocrine
Addisons disease .
Cushing’s syndrome .
Pregnancy
11 Metabolic
Biliary cirrhosis.
Haemochromatosis.
Porphyria.
12 Nutritional
Malabsorption
Carcinomatosis
Kwashiorkor
Pellagra
