Third Month to Birth: TheFetus and Placenta/2
Dr.SumeyaFETAL MEMBRANES AND PLACENTA
Changes in the trophoplast
The fetal component of placenta is derived from the trophoplast and extraembryonic mesoderm(chorionic plate);the maternal component is derived from the uterine endometrium.
Human embryo at the beginning of the second month of development. At the embryonic pole, villi are
numerous and well formed; at the abembryonic pole, they are few in number and poorly developed.
Changes in trophoplast
Maternal blood is delivered to the placenta by spiral arteries in the uterus.Erosion of these maternal vessels to release blood into intervillous spaces is accomplished by endovascular invasion by cytotrophoblast cells.
These cells, released from the ends of anchoring villi invade the terminal ends of spiral arteries, where they replace maternal endothelial cells in the vessels’ walls, creating hybrid vessels containing both fetal and maternal cells.
To accomplish this process, cytotrophoblast cells undergo an epithelial-to-endothelial transition.
Invasion of the spiral arteries by cytotrophoblast cells transforms these vessels from small-diameter, high-resistance vessels to large diameter, lowr esistance vessels that can provide increased quantities of maternal blood to intervillous spaces
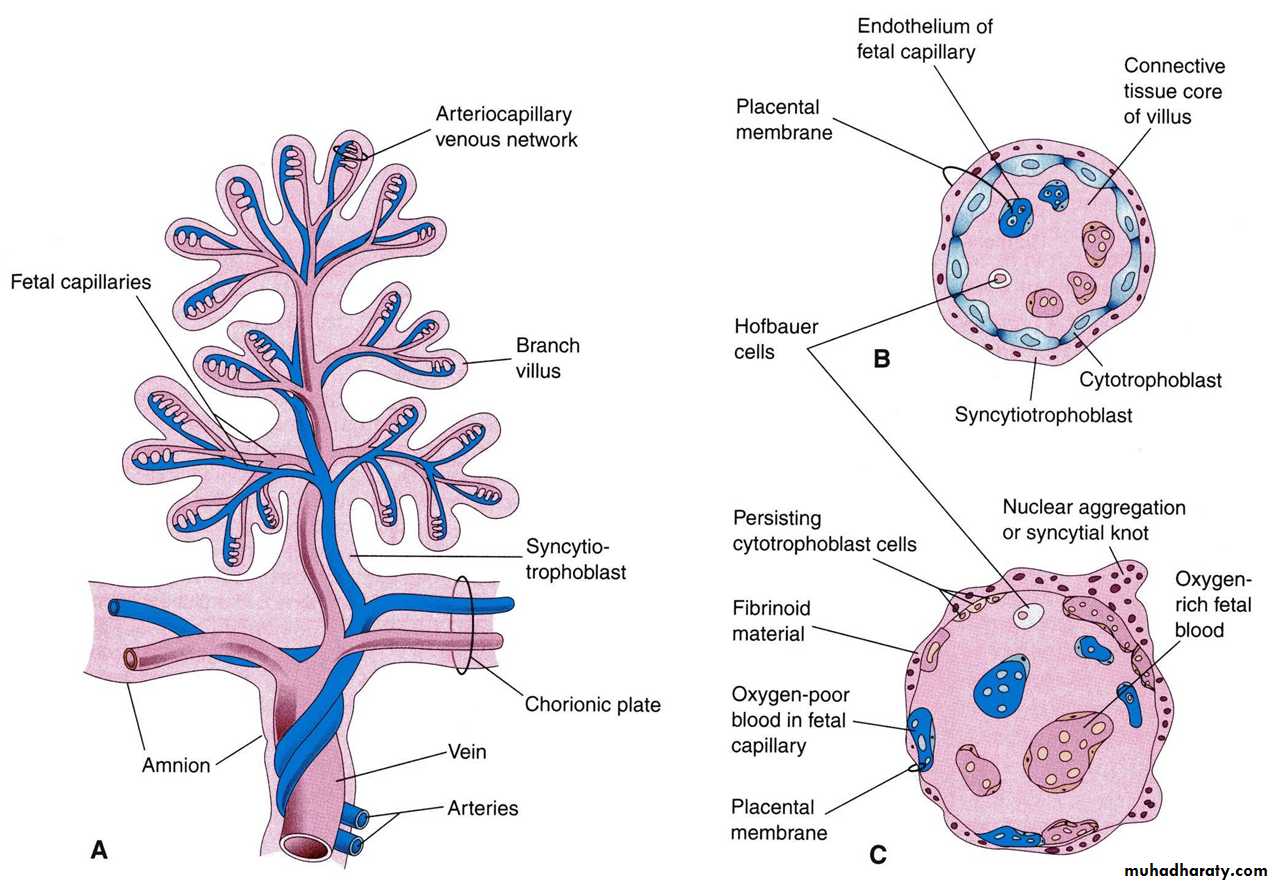
During the following months, numerous small extensions grow out from existing stem villi and extend as free villi into the surrounding lacunar or intervillous spaces.
Initially, these newly formed free villi are primitive but by the beginning of the fourth month, cytotrophoblastic cells and some connective tissue cells disappear.
The syncytium and endothelial wall of the blood vessels are then the only layers that separate the maternal and fetal circulations
STRUCTURE OF STEM CHORIONIC VILLUS
chorion frondosum and Decidua basalis
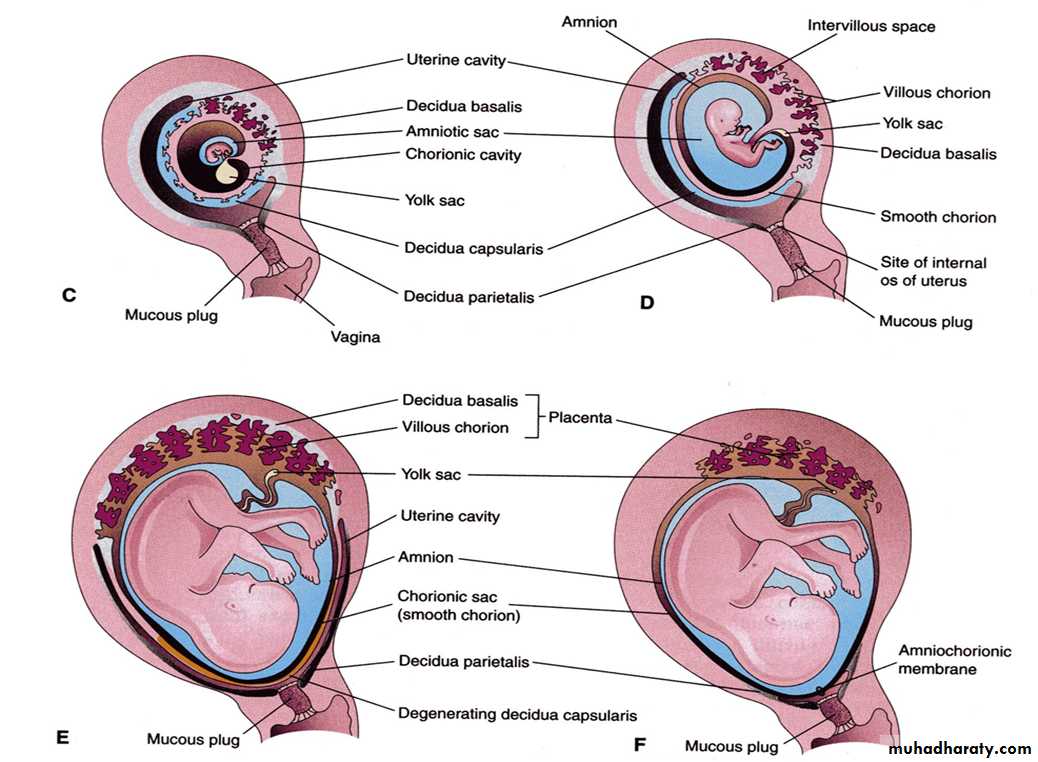
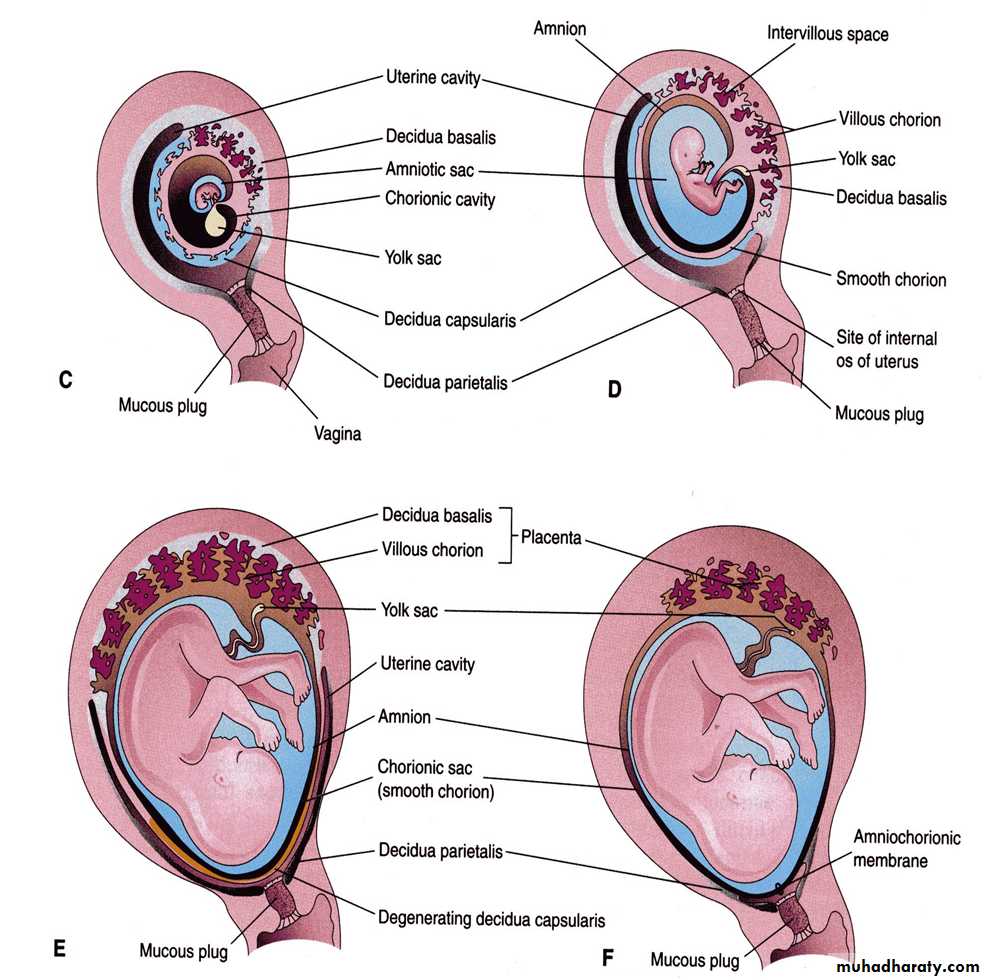
In the early weeks of development villi cover the entire surface of the chorion .As pregnancy advances villi on the emberionic pole continue to grow and expand ,giving rise to the chorion frondosum (bushy chorion ).Villi on the abemberyonic pole degenerate ,and by the third month , this side of the chorion ,now known as the chorion leave , is smooth.
The difference between the embryonic and abembryonic poles of the chorion is also reflected in the structure of the decidua, the functional layer of the endometrium, which is shed during parturition.
The decidua over the chorion frondosum, the decidua basalis, consists of a compact layer of large cells, decidual cells, with abundant amounts of lipids and glycogen.
This layer, the decidual plate, is tightly connected to the chorion. The decidual layer over the abembryonic pole is the decidua capsularis
With growth of the chorionic vesicle, this layer becomes stretched and degenerates. Subsequently, the chorion laeve comes into contact with the uterine wall (decidua parietalis) on the opposite side of the uterus, and the two fuse, obliterating the uterine lumen.
Hence, the only portion of the chorion participating in the exchange process is the chorion frondosum, which, together with the decidua basalis, makes up the placenta.
Similarly, fusion of the amnion and chorion to form the amniochorionic membrane obliterates the chorionic cavity. It is this membrane that ruptures during labor (breaking of the water).
Structure of placenta
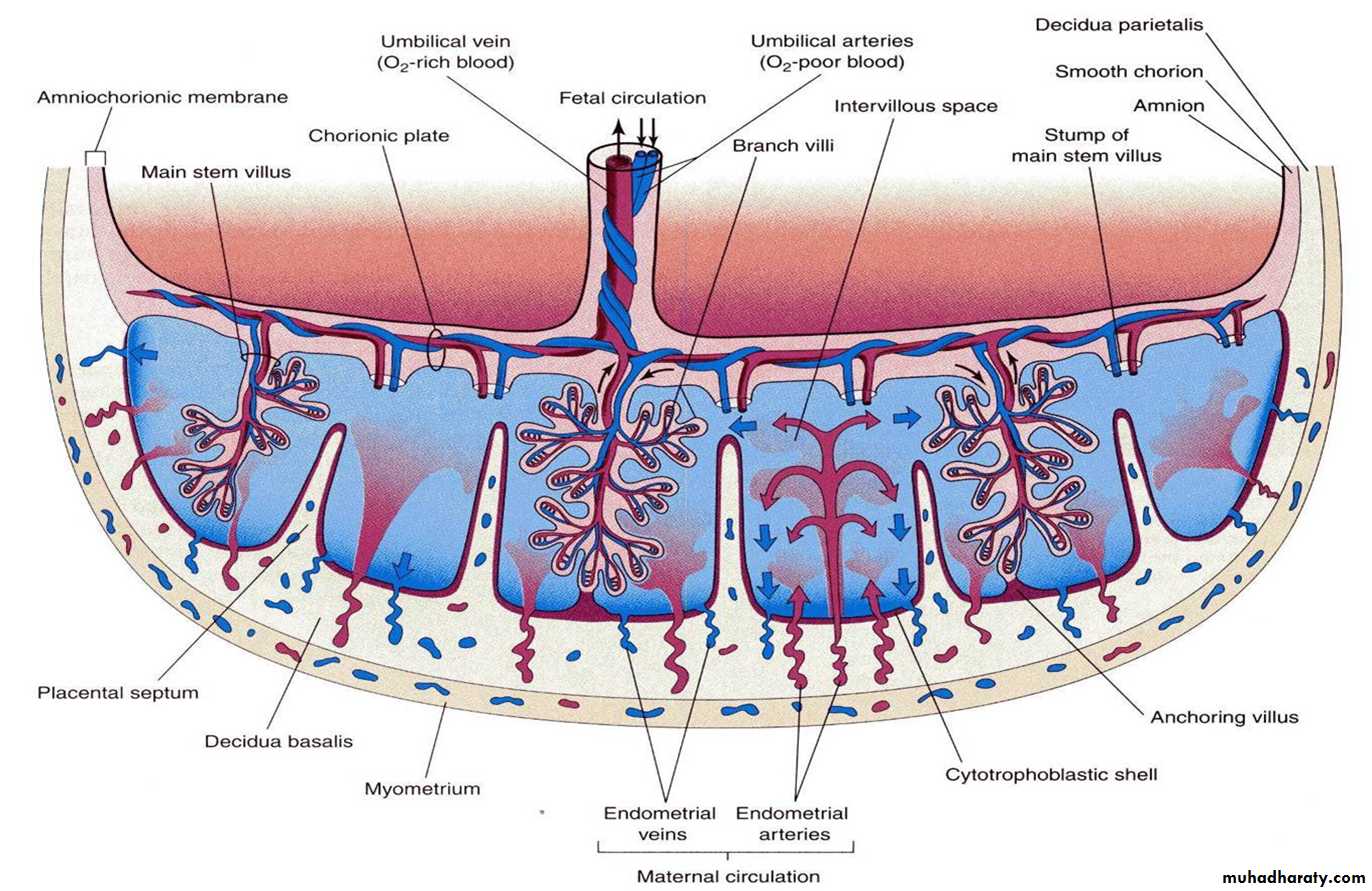
By the beginning of the fourth month, the placenta has two components: (1) a fetal portion, formed by the chorion frondosum and (2) a maternal portion, formed by the decidua basalis.On the fetal side, the placenta is bordered by the chorionic plate on its maternal side, it is bordered by the decidua basalis, of which the decidual plate is most intimately incorporated into the placenta.
In the junctional zone, trophoblast and decidual cells intermingle. This zone, characterized by decidual and syncytial giant cells, is rich in amorphous extracellular material. By this time, most cytotrophoblast cells have degenerated
. Between the chorionic and decidual plates are the intervillous spaces, which are filled with maternal blood. They are derived from lacunae in the syncytiotrophoblast and are lined with syncytium of fetal origin. The villous trees grow into the intervillous blood lakes.
During the fourth and fi fth months, the decidua forms a number of decidual septa, which project into intervillous spaces but do not reach the chorionic plate.
These septa have a core of maternal tissue, but their surface is covered by a layer of syncytial cells, so that at all times, a syncytial layer separates maternal blood in intervillous lakes from fetal tissue of the villi.
As a result of this septum formation, the placenta is divided into a number of compartments, or cotyledons Because the decidual septa do not reach the chorionic plate, contact between intervillous spaces in the various cotyledons is maintained.
As a result of the continuous growth of the fetus and expansion of the uterus, the placenta also enlarges. Its increase in surface area roughly parallels that of the expanding uterus, and throughout pregnancy, it covers approximately 15% to 30% of the internal surface of the uterus.
The increase in thickness of the placenta results from arborization of existing villi and is not caused by further penetration into maternal tissues.
Full-Term Placenta
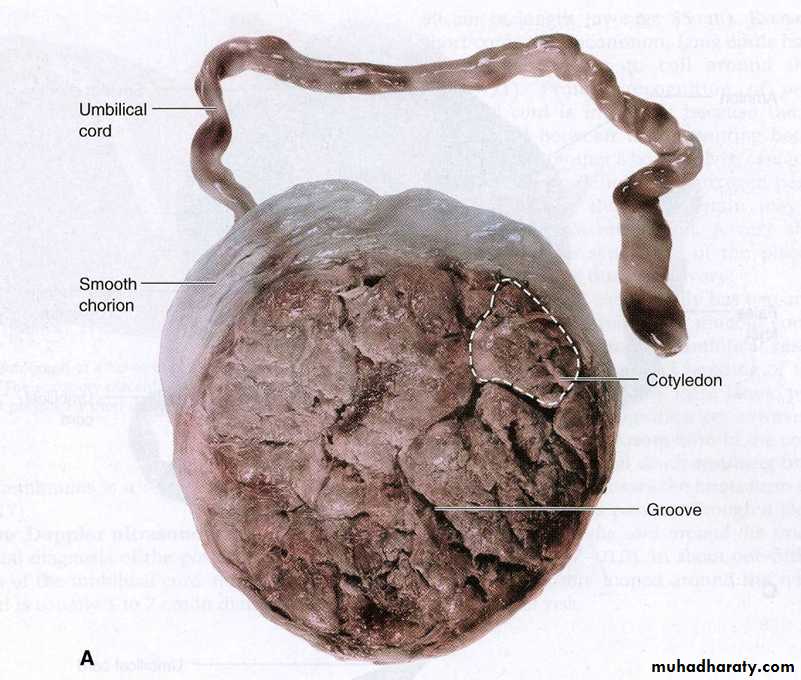
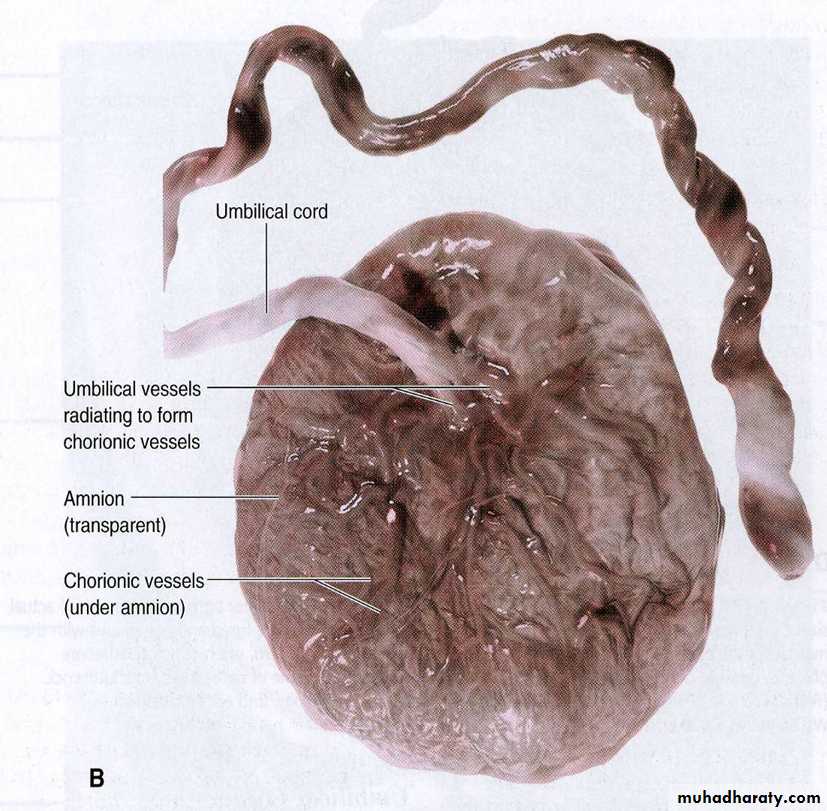
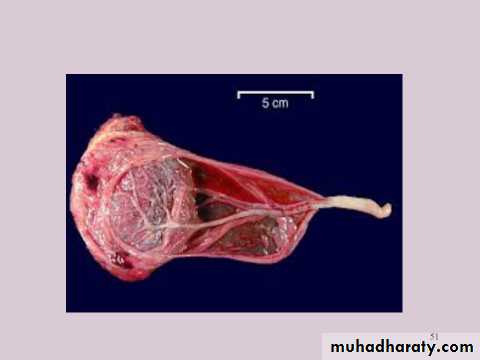
At full term, the placenta is discoid with a diameter of 15 to 25 cm, is approximately 3 cm thick, and weighs about 500 to 600 g.At birth, it is torn from the uterine wall and,approximately 30 minutes after birth of the child, is expelled from the uterine cavity as the afterbirth.
When the placenta is viewed from the maternal side, 15 to 20 slightly bulging areas, the cotyledons, covered by a thin layer of decidua basalis, are clearly recognizable Grooves between the cotyledons are formed by decidual septa.
The fetal surface of the placenta is covered entirely by the chorionic plate. A number of large arteries and veins, the chorionic vessels, converge toward the umbilical cord.
The chorion, in turn, is covered by the amnion.
Attachment of the umbilical cord is usually eccentric and occasionally even marginal. Rarely, however, does it insert into the chorionic membranes outside the placenta (velamentous insertion).
Maternal side
Fetal side
velamentous insertion
Circulation of the Placenta
Cotyledons receive their blood through 80 to 100 spiral arteries that pierce the decidual plate and enter the intervillous spaces at more or less regular intervals.Pressure in these arteries forces the blood deep into the intervillous spaces and bathes the numerous small villi of the villous tree in oxygenated blood.
As the pressure decreases, blood flows back from the chorionic plate toward the decidua, where it enters the endometrial veins.
Hence, blood from the intervillous lakes drains back into the maternal circulation through the endometrial veins.
Collectively, the intervillous spaces of a mature placenta contain approximately 150 mL.
Functions Of The Placenta
• Exchange of gases• Exchange of nutrition and electrolytes
• Transmission of maternal antibodies
• Excretion
• Hormone production
Placental endocrine synthesis
The syncytiotrophoblast synthesizes protein &steroid hormonesThe protein homones
1- human chorionic gonadotropin
2- h.c. somatomammotropin
3-h.c. thyrotropin
4-h.c. corticotropin
The steroid hormones
Progesterone & Estrogens
Amnion and umbilical cord
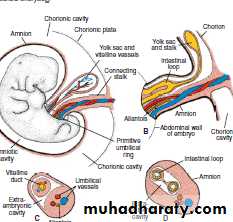
At the fifth week of development ,the following structures pass through the ring(1)the connecting stalk, containing the allantois and the umbilical vessels, consisting of two arteries and one vein;
(2) the yolk stalk (vitelline duct), accompanied by the vitelline vessels;
(3) the canal connecting the intraembryonic and extraembryonic cavities
. During further development, the amniotic cavity enlarges rapidly at the expense of the chorionic cavity, and the amnion begins to envelop the connecting and yolk sac stalks, crowding them together and giving rise to the primitive umbilical cord
The abdominal cavity is temporarily too small for the rapidly developing intestinal loops, and some of them are pushed into the extraembryonic space in the umbilical cord.
These extruding intestinal loops form a physiological umbilical hernia.
At approximately the end of the third month, the loops are withdrawn into the body of the embryo, and the cavity in the cord is obliterated.
When the allantois and the vitelline duct and its vessels are also obliterated, all that remains in the cord are the umbilical vessels surrounded by Wharton’s jelly.
This tissue, which is rich in proteoglycans, functions as a protective layer for the blood vessels.
The walls of the arteries are muscular and contain many elastic fi bers, which contribute to a rapid constriction and contraction of the umbilical vessels after the cord is tied off.
PLACENTAL CHANGES AT THEEND OF PREGNANCY
At the end of pregnancy, a number of changes that occur in the placenta may indicate reduced exchange between the two circulations.These changes include
1- an increase in fibrous tissue in the core of the villus
2- thickening of basement membranes in fetal capillaries, of the villi
3- deposition of fibrinoid on the surface of the villi in the juncional zone and in the chorionic plate.
Excessive fibrinoid formation frequently causes infarction of an intervillous lake or sometimes of an entire cotyledon. The cotyledone then assumes a whitish appearance.
Amniotic fluid
The amniotic cavity is filled with a clear ,watery fluid that is produced in part by amniotic cells but is derived primarily from maternal blood .The amount of fluid increase from approximately 30 mL at 10 weeks of gestation to 450 mL at 20 weeks to 800 to 1000 mL at 37 weeks .During the early month of pregnancy ,the embryo is suspended by its umbilical cord in this fluid ,which serves as a protective cushion .
The fluid 1-absorbs jolts 2- prevents adherence of the embryo to the amnion 3- allows for fetal movements .
The volume of amniotic fluid is replaced every 3hours .
From the beginning of the fifth month ,and it is estimated that it drinks about 400mL a day ,about half of the total amount.Fetal urine is added daily to the amniotic fluid in the fifth month, but this urine is mostly water , because the placenta is functioning as an exchange for metabolic wastes.
During childbirth, the amniochorionic membrane forms a hydrostatic wedge that helps to dilate the cervical canal.
Dizygotic Twins(Fraternal Twins)
38Two eggs are ovulated and each is fertilized by a sperm cell
No more genetically similar than any other sibling in the family (can be same/different sexes)
Maternal age, use of assisted reproductive technologies are factors
39
Monozygotic Twin
• One egg is fertilized by one sperm
• Have identical genes and must be of the same sex
• (Incidence: about 3 in every 1000 births)
•
They result from splitting of the zygote at various stages of development .The earliest separation at two cell stage.
The splitting of zygote usually occurs at the early blastocyst stage.The inner cell mass splits into two separate groups of cells within the sameblastocyst cavity.
The two embryos have a common placenta and a common chorionic cavity but separate amniotic cavities.
In rare cases, the separation occurs at the bilaminar germ disc stage, just before the appearance of the primitive streak.
This method of splitting results in formation of two partners with a single placenta and a common chorionic and amniotic sac.
Although the twins have a common placenta, blood supply is usually well balanced.
Although triplets are rare (about one per 7,600 pregnancies), birth of quadruplets, quintuplets, and so forth is rarer.
In recent years, multiple births have occurred more frequently in mothers given gonadotropins (fertility drugs) for ovulatory failure.
parturition (birth)
Signals initiating parturition (birth) are not clear, but preparation for labor usually begins between 34 and 38 weeks.Labor itself consists of three stages:
(1) effacement and dilatation of the cervix,
(2) delivery of the fetus, and
(3) delivery of the placenta and fetal