
Dr. Faez Khalaf Abdulmuhsen
MBChB,FIBMS-CABMS(IM),MD-FACP(US), FIBMS
(GIT&HEP)
Subspecialist Gastroenterologist & Endoscopisit
Medical college ,Thi Qar U, Internal medicine department
Al Hussein Teaching Hospital –GIT Center
Member of Iraqi gastroenterology society
Hepatology lectures 2020

INFECTIONS AND THE LIVER
The liver may be subject to a number of different
infections. These include hepatotropic viral
infections, and bacterial and protozoal infections.
Each has specific clinical features and requires
targeted therapies.

Viral hepatitis
This must be considered in anyone presenting with
hepatitis liver blood tests (high transaminases).
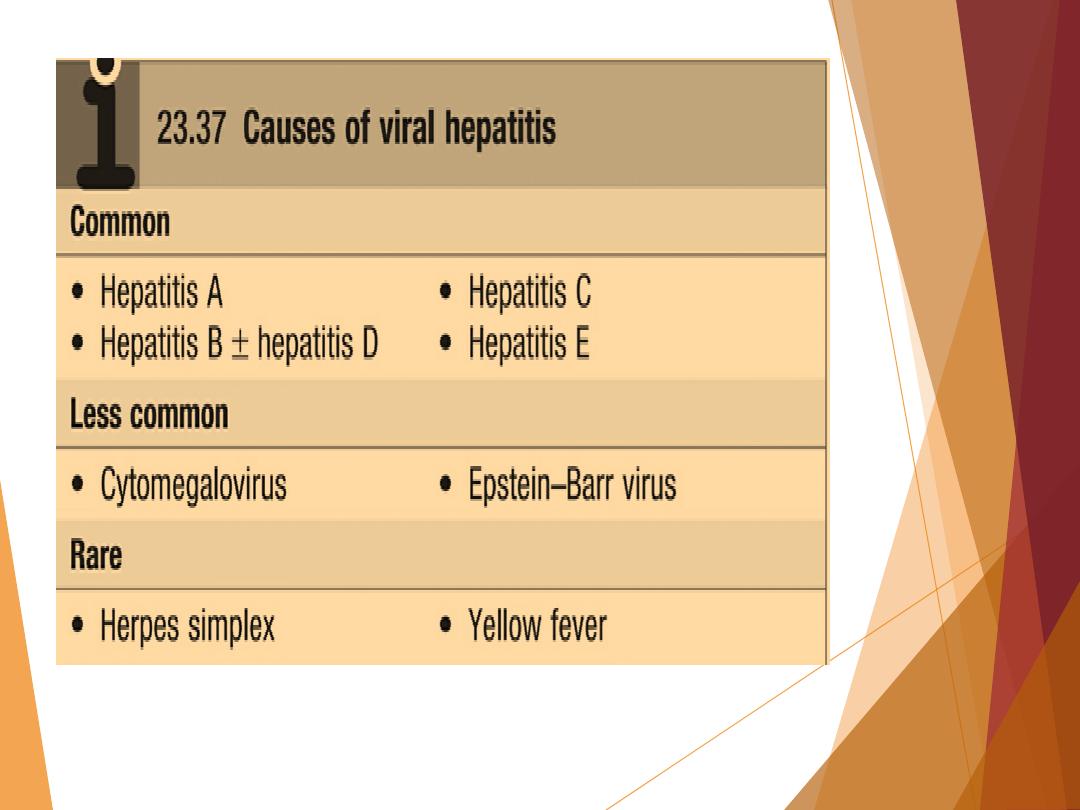
The causes are listed in Box 23.37.
All these viruses cause illnesses with similar clinical
and pathological features and which are frequently
anicteric or even asymptomatic.
They differ in their tendency to cause acute and
chronic infections.
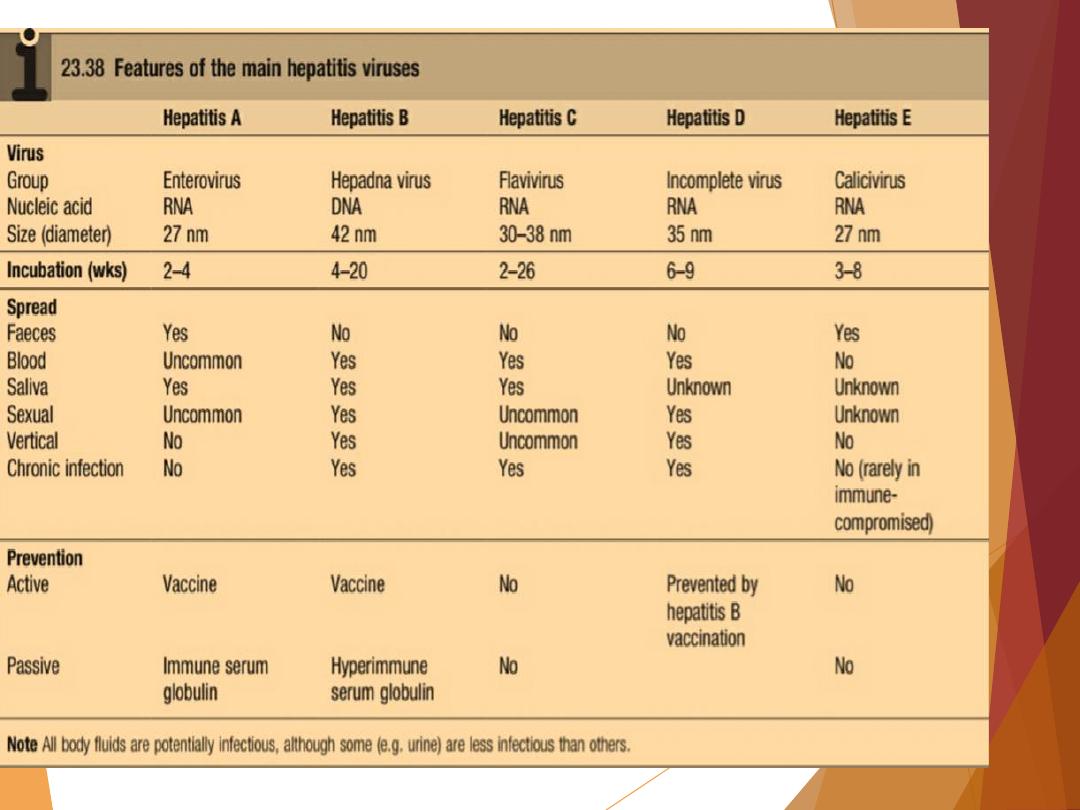
The features of the major hepatitis viruses are shown
in Box 23.38.

Clinical features of acute
infection
A non-specific prodromal illness characterised by headache, myalgia, arthralgia,
nausea and anorexia usually precedes the development of jaundice by a few
days to 2 weeks.
Vomiting and diarrhoea may follow, and abdominal discomfort is common.
Dark urine and pale stools may precede jaundice.
There are usually few physical signs.
The liver is often tender but only minimally enlarged.
Occasionally, mild splenomegaly and cervical lymphadenopathy are seen.
These are more frequent in children or those with Epstein–Barr virus (EBV)
infection. Symptoms rarely last longer than 3–6 weeks. Complications may
occur but are rare.
1- Acute liver failure 2-Cholestatic hepatitis (hepatitis A)
3- Aplastic anemia 4- Chronic liver disease
5.cirrhosis (hepatitis B and C) 6• Relapsing hepatitis

Investigations:
A hepatitic pattern of LFTs develops, with serum
transaminases typically between 200 and 2000 U/L in an
acute infection (usually lower and fluctuating in chronic
infections).
The plasma bilirubin reflects the degree of liver damage.
The ALP rarely exceeds twice the upper limit of normal.
Prolongation of the PT indicates the severity of the
hepatitis but rarely exceeds 25 seconds, except in rare
cases of acute liver failure.
The white cell count is usually normal with a relative
lymphocytosis. Serological tests confirm the aetiology of
the infection.

Management in general
1.
Most individuals do not need hospital care.
2.
Drugs such as sedatives and narcotics, which are
metabolised in the liver, should be avoided.
3.
No specific dietary modifications are needed.
4.
Alcohol should be avoided during the acute illness.
5.
Elective surgery should be avoided in cases of acute viral
hepatitis (a risk of post-operative liver failure).
6.
Liver transplantation is very rarely indicated for acute
viral hepatitis complicated by liver failure.

Hepatitis A
(HAV) belongs to the picornavirus group of enteroviruses. HAV is
highly infectious and is spread by the
faecal–oral
route.
Infected individuals, who may be asymptomatic, excrete the
virus in faeces for about 2–3 weeks before the onset of
symptoms and then for a further 2 weeks or so
.
Infection is common in children but often asymptomatic
, and so
up to 30% of adults will have serological evidence of past
infection
but give no history of jaundice.
Infection is also more common in areas of overcrowding and
poor sanitation.
In occasional outbreaks, water and shellfish have been the
vehicles of transmission. A chronic carrier state does not occur.

Investigations: Only one HAV antigen has been found and infected
people make an antibody to this antigen (anti-HAV
).
Anti-HAV is important in diagnosis
, as HAV is only present in the blood
transiently during the incubation period.
Excretion in the stools occurs for only 7–14 days after the onset of the
clinical illness and the virus cannot be grown readily
.
Anti-HAV of the IgM type, indicating a primary immune response
, is
already present in the blood at the onset of the clinical illness and is
diagnostic of an acute HAV infection.
Titres of this antibody fall to low levels within about 3 months of
recovery
.
Anti-HAV of the IgG type is of no diagnostic value
, as HAV infection is
common and this antibody persists for years after infection, but it
can
be used as a marker of previous HAV
infection. Its presence indicates
immunity to HAV.

Management: Infection in the community is
best prevented by improving
social conditions
, especially overcrowding and poor sanitation.
Individuals can be given substantial protection from infection by active
immunisation with an inactivated virus vaccine.
Immunisation should be considered for individuals with chronic hepatitis B or
C infections
.
Immediate protection can be provided by immune serum globulin if this is
given soon after exposure to the virus.
The protective effect of immune serum globulin is attributed to its anti-HAV
content.
Immunisation should be considered for those at particular risk:
1- close contacts of HAV-infected patients .
2-The elderly, those with other major disease .
3-Pregnant women.
4-People travelling to endemic areas are best protected by vaccination

Immune serum globulin can be effective in an outbreak of
hepatitis, in a school or nursery, as injection of those at risk
prevents secondary spread to families.
Acute liver failure is rare in hepatitis A
(0.1%) and chronic
infection does not occur
.
However, HAV infection in patients with chronic liver
disease may cause serious or life-threatening disease. In
adults,
a cholestatic phase
with elevated ALP levels may
complicate infection.
There is no role for antiviral drugs in the therapy of HAV
infection.

Hepatitis E
Hepatitis E is caused by an RNA virus that is
endemic in India and the Middle East. An increase
in prevalence has recently been noted in northern
Europe and infection is no longer seen only in
travellers from an endemic area.
The clinical presentation and management of
hepatitis E are similar to that of hepatitis A.
Disease is spread via the faecal–oral route; in most
cases, it presents as a self-limiting acute hepatitis
and does not usually cause chronic liver disease,
although some cases have been described, usually
in immunocompromised patients. Hepatitis E
differs from hepatitis A in that infection during
pregnancy is associated with the development of
acute liver failure, which has a high mortality. In
acute infection, IgM antibodies to HEV are positive.

Hepatitis B
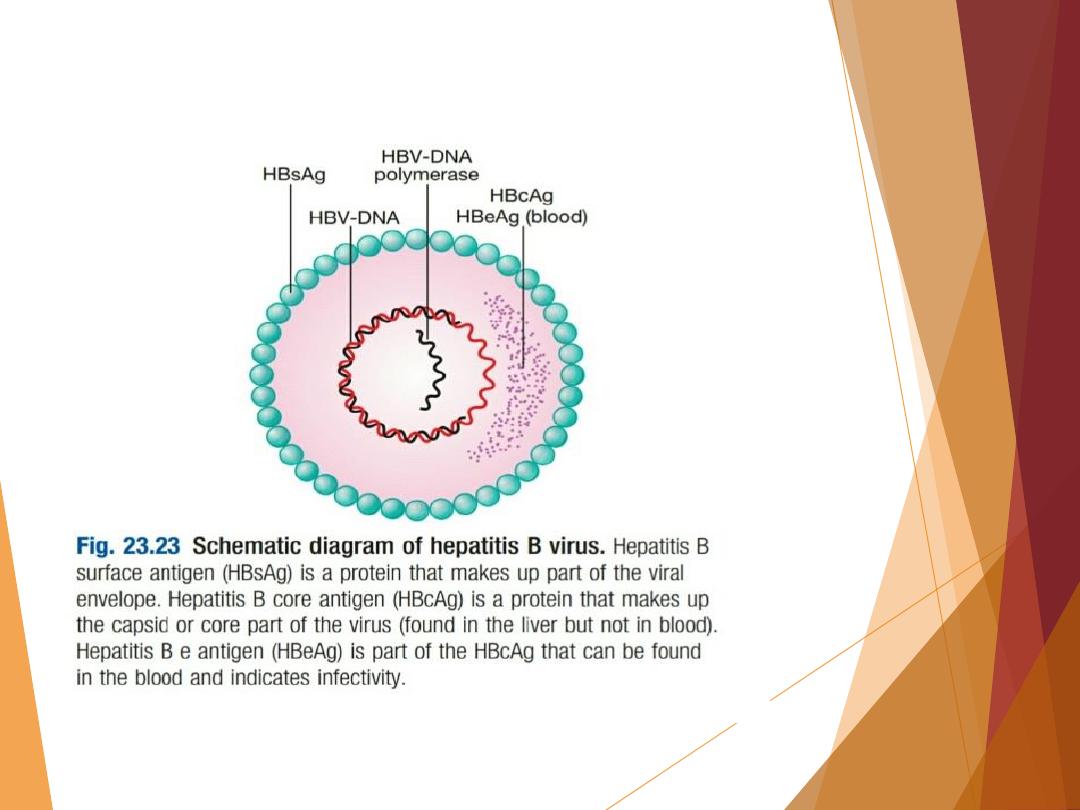
The HBV consists of a core containing DNA and a DNA polymerase
enzyme needed for virus replication. The core of the virus is
surrounded by surface protein (Fig. 23.23).
The virus, also called a Dane particle, and an excess of its surface
protein (known as hepatitis B surface antigen) circulate in the
blood.
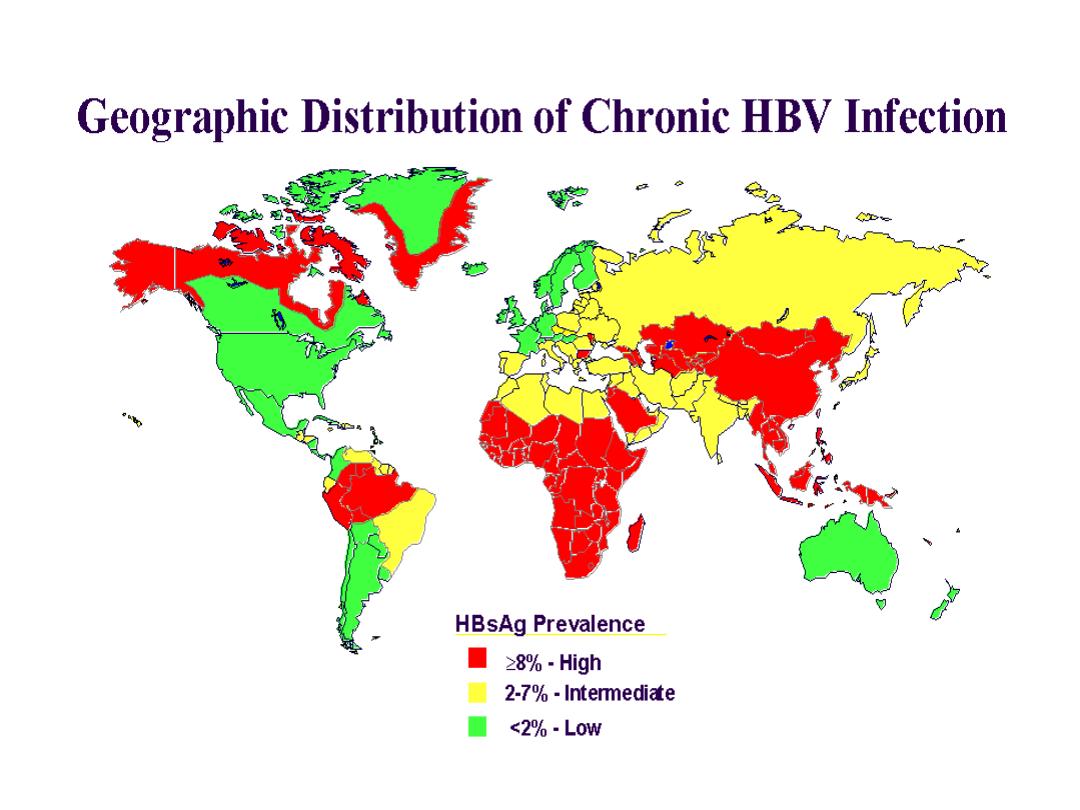
Humans are the only source of infection
. Hepatitis B is one of the
most common causes of chronic liver disease and hepatocellular
carcinoma
worldwide. Approximately one-third of the world’s
population have serological evidence of past or current infection
with hepatitis B and approximately
350–400 million people are
chronic HBsAg carriers
.
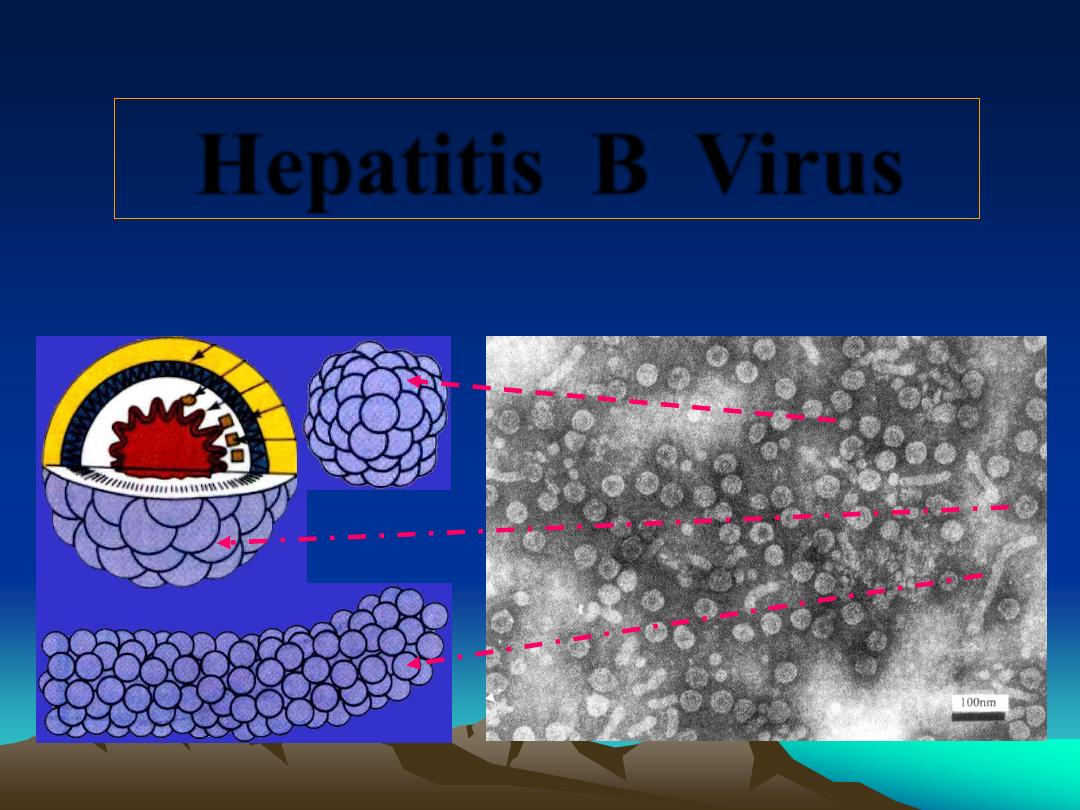
Hepatitis B Virus

Hepatitis B may cause an acute viral hepatitis; however, acute
infection is
often asymptomatic
, particularly when acquired at
birth. Many individuals with chronic hepatitis B are also
asymptomatic.
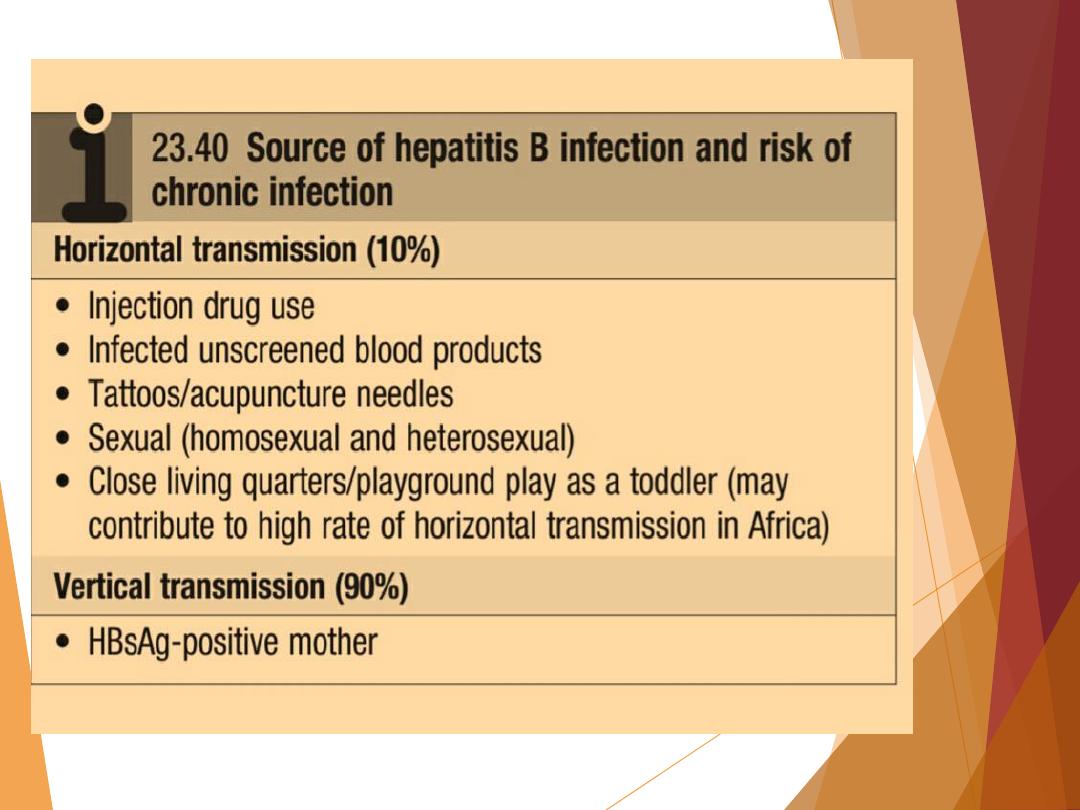
The risk of progression to chronic liver disease depends on the
source and timing of infection (Box 23.40). Vertical transmission
from mother to child in the perinatal period is the most common
cause of infection worldwide and carries the highest risk of
ongoing chronic infection.
In this setting, adaptive immune responses to HBV may be absent
initially, with apparent immunological tolerance. Several
mechanisms contribute towards this.

1-Firstly, the introduction of antigen in the neonatal period is
tolerogenic.
2-Secondly, the presentation of such antigen within the liver, as
described above, promotes tolerance; this is particularly evident
in the absence of a significant innate or inflammatory response.
3-Finally, very high loads of antigen may lead to so-called
‘exhaustion’ of cellular immune responses. However, the state of
tolerance is not permanent and may be reversed as a result of
therapy, or through spontaneous changes in innate responses
such as interferon-alpha and NK cells, accompanied by host-
mediated immunopathology.
High
Moderate
Low/Not
Detectable
blood
semen
urine
serum
vaginal fluid
feces
wound exudates
saliva
sweat
tears
breastmilk
Concentration of Hepatitis B Virus
in Various Body Fluids

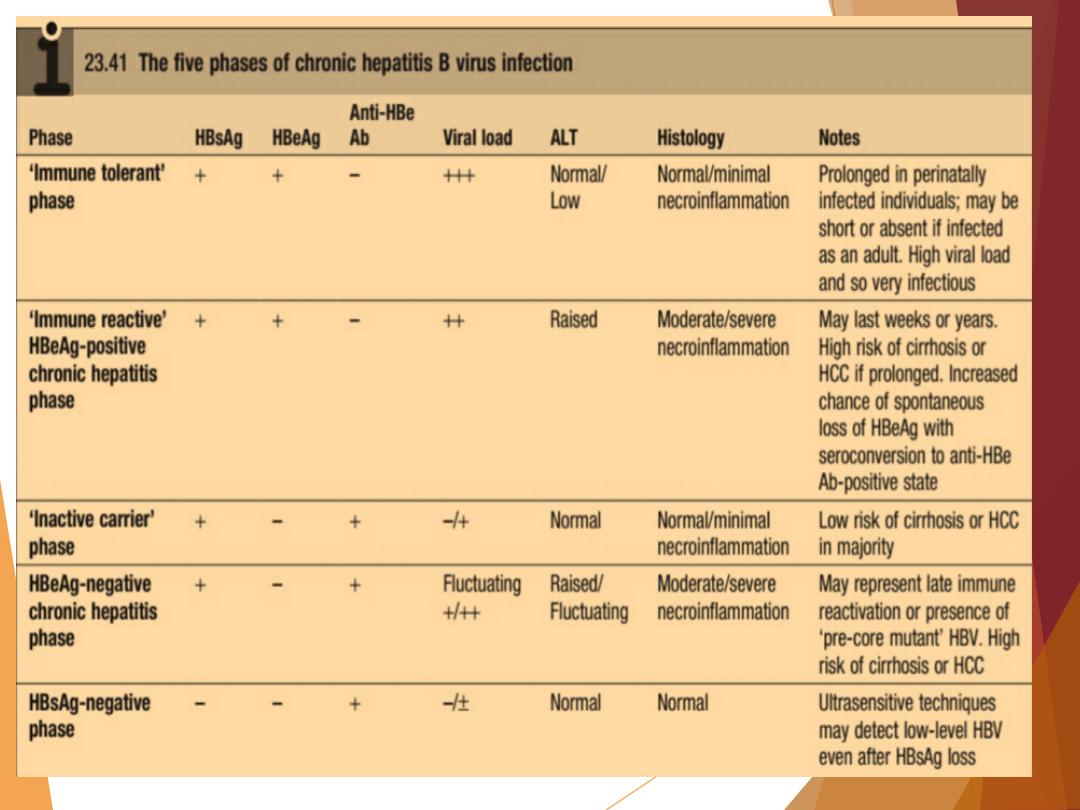
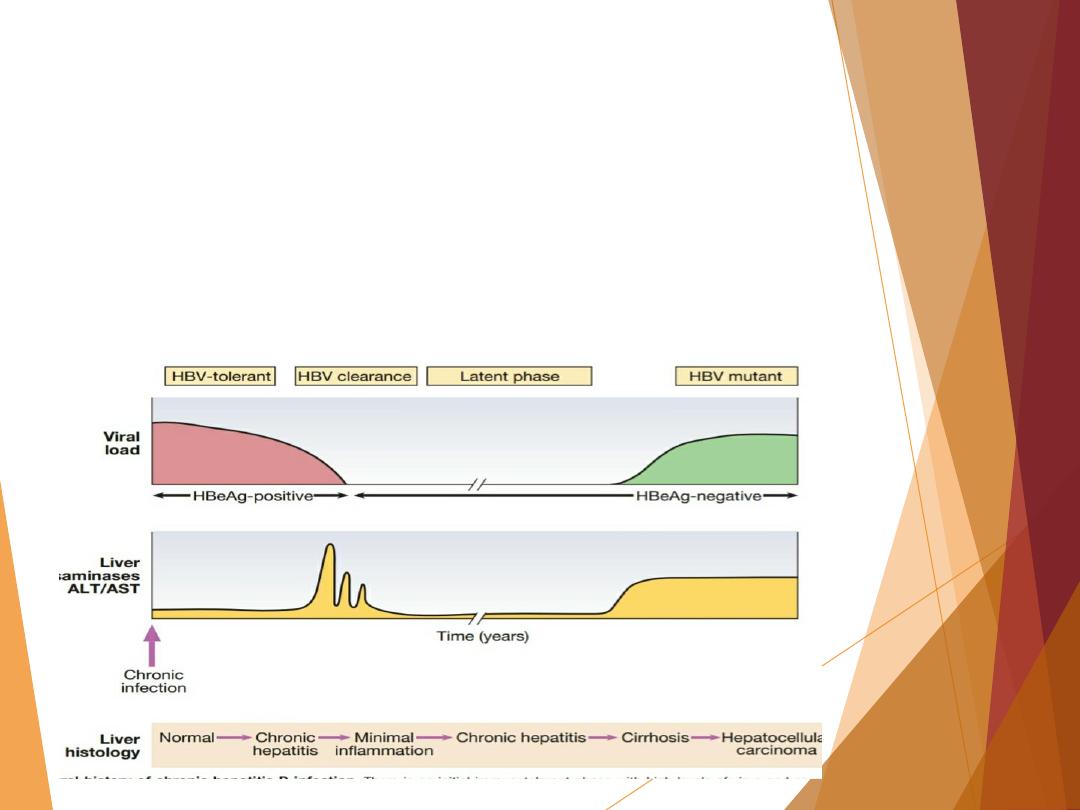
Chronic hepatitis can lead to cirrhosis or HCC, usually after
decades of infection (Fig. 23.24).
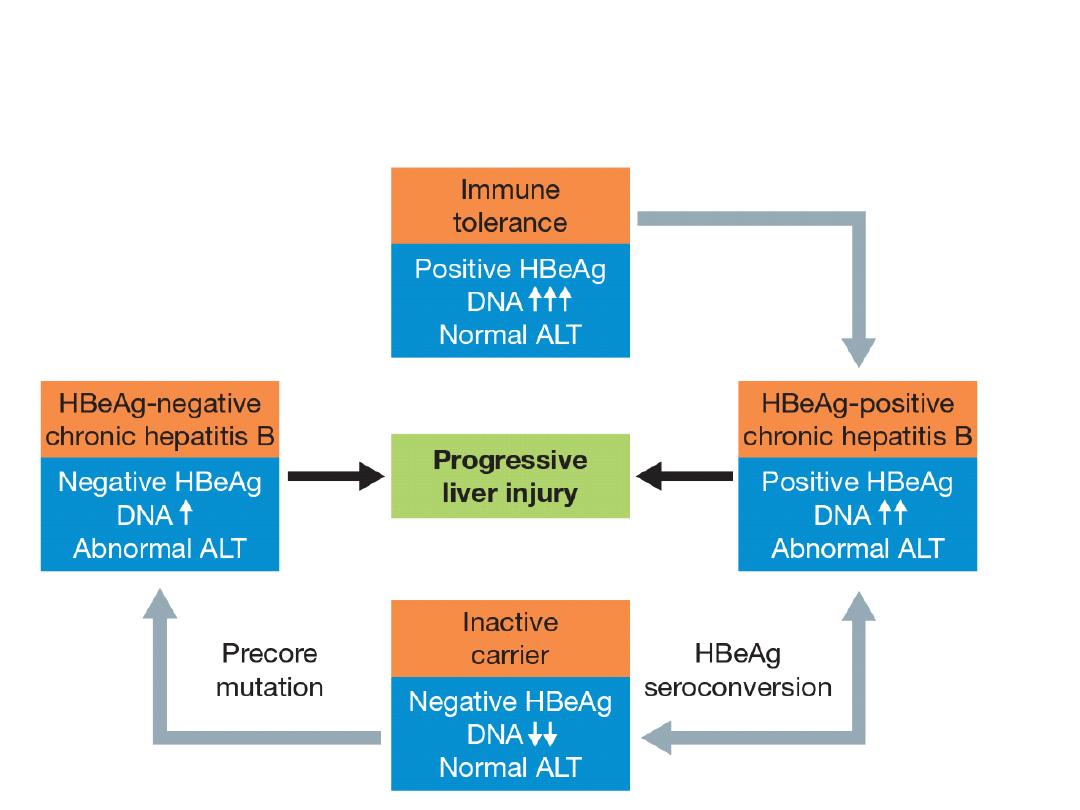
Chronic HBV infection is a dynamic process that can be
divided into five phases (Box 23.41); however, these are not
necessarily sequential and not all patients will go through
all phases.
It should be remembered that the virus is not directly
cytotoxic to cells; rather it is an immune response to viral
antigens
displayed on infected hepatocytes that initiates
liver injury.
This explains why there may be very high levels of viral
replication but little hepatocellular damage during the
‘immune tolerant’ phase.
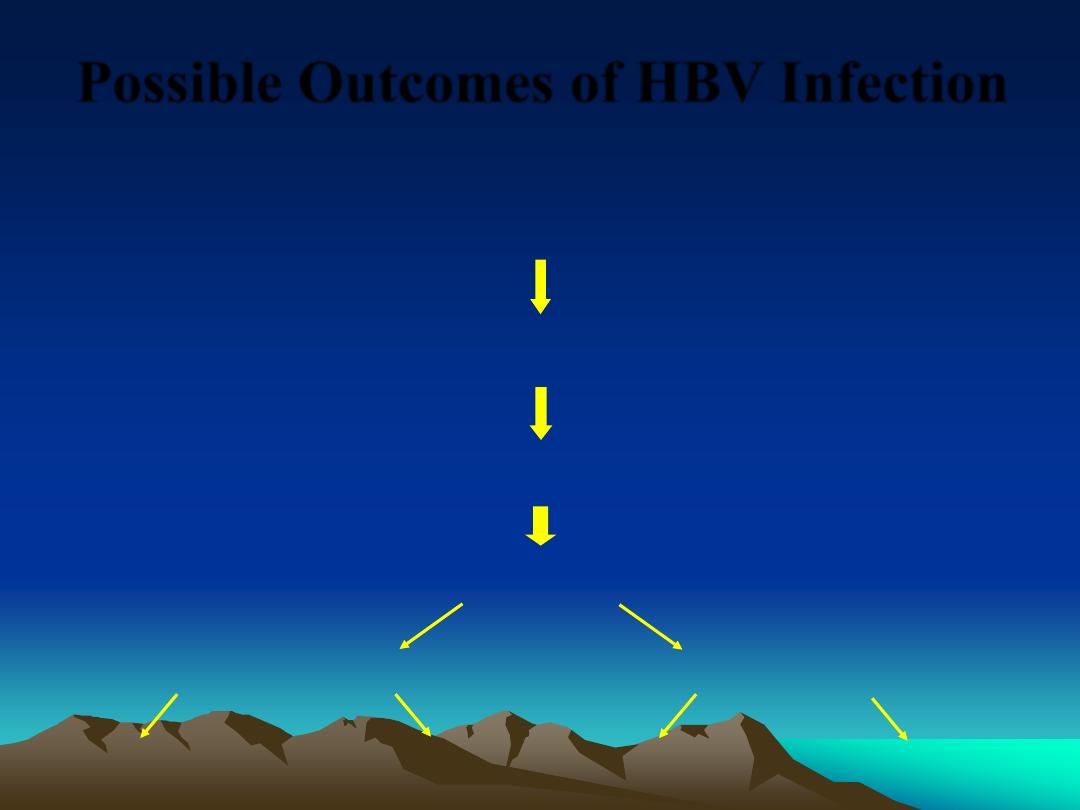
Possible Outcomes of HBV Infection
Acute
hepatitis B infection
Chronic
HBV infection
3-5% of adult-
acquired infections
95% of infant-
acquired infections
Cirrhosis
Chronic hepatitis
12-25% in 5 years
Liver failure
Hepatocellular
carcinoma
Liver transplant
6-15% in 5 years
20-23% in 5 years
Death
Death
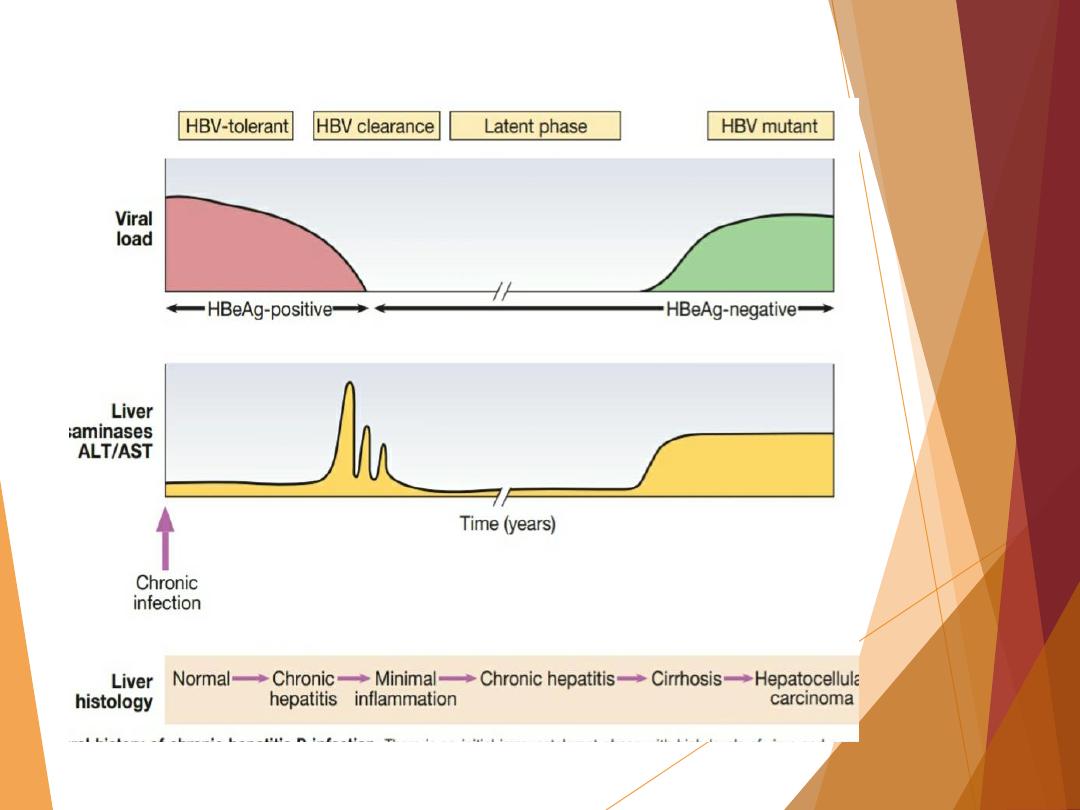
Natural history of chronic hepatitis B
HBeAg positive
HBeAg Negative
Chronic infection
Chronic hepatitis
Chronic infection
Chronic hepatitis
HBsAg
High
High/intermediate
Low
Intermediate
HBeAg
Positive
Positive
Negative
Negative
HBV DNA
>104 IU/ml
104-107 IU/ml
<2,000 IU/ml°°
>2,000 IU/ml
ALT
Normal
Elevated
Normal
Elevated*
Liver disease
Normal
Moderate/severe
None
Moderate/severe
Old terminology
Immune tolerant
Immune reactive
Hbe Ag positive
Inactive carrier
Hbe Ag negative chronic
hepatitis
Fig. 1. Natural history and assessment of patients with chronic HBV infection based upon HBV and liver disease markers. *Persistently or intermittently. HBV DNA
levels can be between 2,000 and 20,000 IU/ml in some patients without sings of chronic hepatitis.

Investigations
a)Serology
HBV contains several antigens to which infected persons
can make immune responses.
These antigens and their antibodies are important in
identifying HBV infection (Boxes 23.41 and 23.42), although
the widespread availability of polymerase chain reaction
(PCR) techniques to measure viral DNA levels in peripheral
blood means that longitudinal monitoring is now also
frequently guided by direct assessment of viral load.

1)
Hepatitis B surface antigen (HBsAg)
. HBsAg is an indicator of
active infection,
and a negative test for HBsAg makes HBV
infection very unlikely
. In acute liver failure from hepatitis B, the
liver damage is mediated by viral clearance and so HBsAg is
negative, with evidence of recent infection shown by the
presence of hepatitis B core IgM. HBsAg appears in the blood late
in the incubation period, but before the prodromal phase of acute
type B hepatitis; it may be present for a few days only,
disappearing even before jaundice has developed, but
usually
lasts for 3–4 weeks and can persist for up to 5 months
.
The persistence of HBsAg for longer than 6 months indicates
chronic infection.
Antibody to HBsAg (anti-HBs) usually appears after about 3–6
months and persists for many years or perhaps permanently. Anti-
HBs implies either a previous infection, in which case anti-HBc. is
usually also present, or previous vaccination, in which case anti-
HBc is not present.

2)Hepatitis B core antigen (HBcAg). HBsAg is not found in the
blood, but antibody to
it (anti-HBc)
appears early in the illness and
rapidly reaches a high titre, which subsides gradually but then
persists. Anti-HBc is initially of IgM type, with IgG antibody
appearing later.
Anti-HBc (IgM) can sometimes reveal an acute
HBV infection when the HBsAg has disappeared and before anti-
HBs has developed
(see Fig. 23.25 and Box 23.42).

3)Hepatitis B e antigen (HBeAg). HBeAg is an indicator of viral
replication. In acute hepatitis B it may appear only transiently at
the outset of the illness; its appearance is followed by the
production of antibody (anti-HBe). The
HBeAg reflects active
replication of the virus in the liver
. Chronic HBV infection is
marked by the presence of HBsAg and anti-HBc (IgG) in the blood.
Usually, HBeAg or anti-HBe is also present; HBeAg indicates
continued active replication of the virus in the liver.
The absence
of HBeAg usually implies low viral replication
;
the exception is
HBeAg-negative chronic hepatitis B (also called ‘pre-core mutant’
infection
, in which high levels of viral replication, serum HBV-DNA
and hepatic necroinflammation are seen, despite negative HBeAg.

b) Viral load and genotype
HBV-DNA can be measured by PCR in the blood. Viral loads are
usually in excess of 10
5
copies/mL in the presence of active viral
replication, as indicated by the presence of e antigen.
In contrast, in those with low viral replication, HBsAg- and anti-
HBe-positive, viral loads are less than 10
5
copies/mL. The
exception is in patients who have a mutation in the pre-core
protein, which means they cannot secrete e antigen into serum
(Fig. 23.26). Such individuals will be anti-HBe-positive but have a
high viral load and often evidence of chronic hepatitis.
These mutations are common in the Far East, and those patients
affected are classified as having e antigen-negative chronic
hepatitis.
They respond differently to antiviral drugs from those with
classical e antigen-positive chronic hepatitis.
Measurement of viral load is important in monitoring antiviral
therapy and identifying patients with pre-core mutants. Specific
HBV genotypes (A–H)
can also be identified using PCR.
In some settings these may be useful in guiding therapy, as
genotype A tends to respond better to pegylated interferon alfa,
compared to genotypes C and D.

Management of acute hepatitis B
Treatment is supportive
, with monitoring for acute liver failure,
which occurs in less than 1% of cases.
There is no definitive evidence that antiviral therapy reduces the
severity or duration of acute hepatitis B.
Full recovery occurs in 90–95% of adults following acute HBV
infection
.
The remaining 5–10% develop a chronic hepatitis B infection that
usually continues for life
,
although later recovery occasionally
occurs
.

Infection passing from mother to child at birth leads to chronic
infection in the child in
90% of cases
and
recovery is rare
. Chronic
infection is also common in immunodeficient individuals, such as
those with Down’s syndrome or human immunodeficiency virus
(HIV) infection. Fulminant liver failure due to acute hepatitis B
occurs in less than 1% of cases.
Recovery from acute HBV infection occurs within 6 months and is
characterised by the appearance of antibody to viral antigens.
Persistence of HBeAg beyond this time indicates chronic
infection.
Combined HBV and HDV infection causes more
aggressive disease.

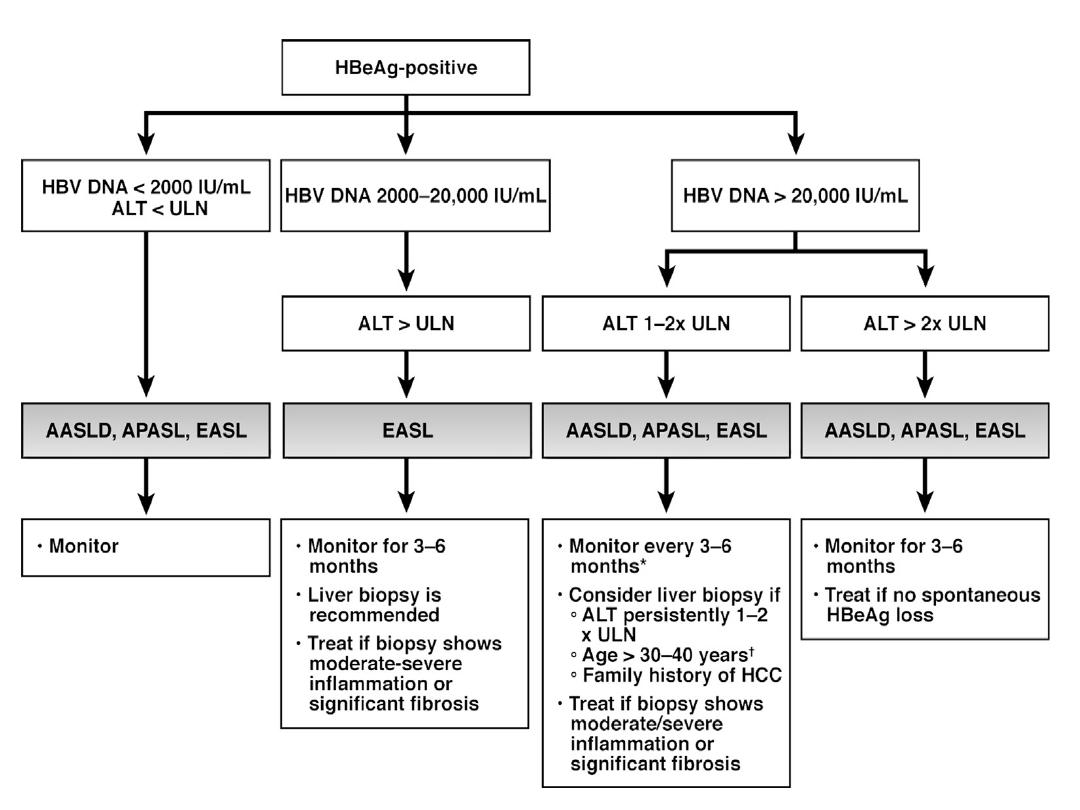
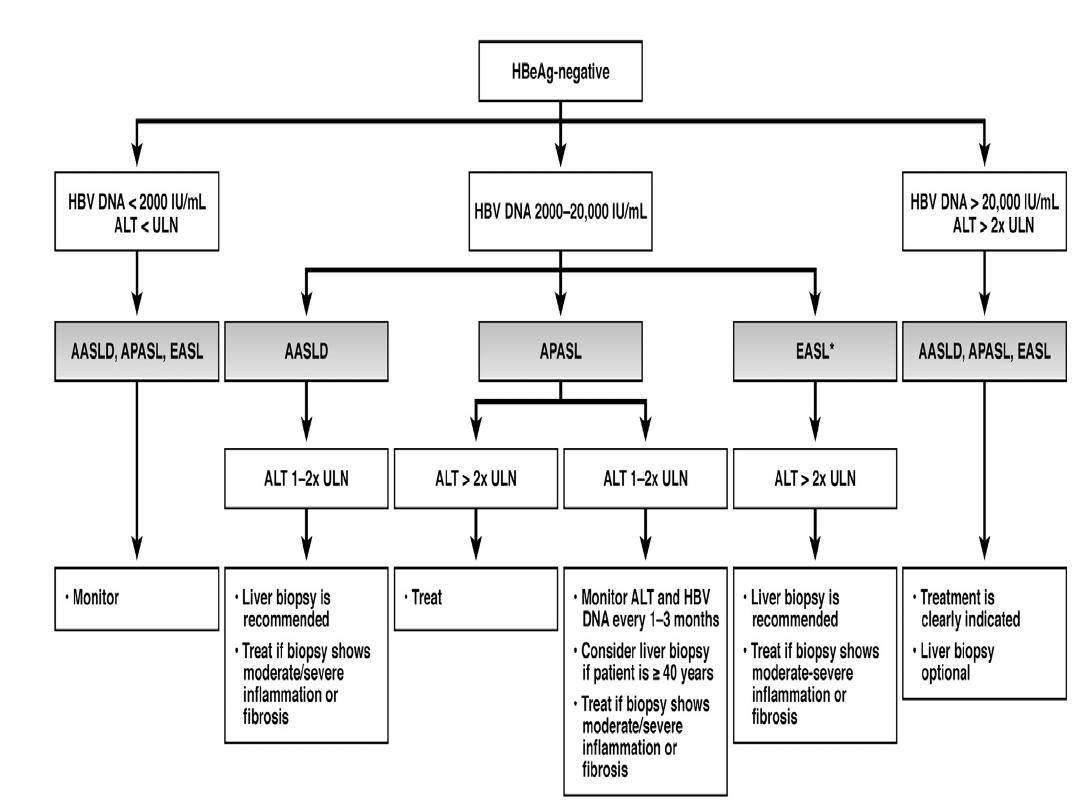
Management of chronic hepatitis B
Treatments are still limited, as no drug is consistently able to
eradicate hepatitis B infection completely (i.e. render the patient
HBsAg-negative).
T
he goals of treatment are HBeAg seroconversion, reduction in
HBV-DNA and normalisation of the LFTs
.
The indication for treatment is a high viral load in the presence
of active hepatitis, as demonstrated by elevated serum
transaminases and/or histological evidence of inflammation and
fibrosis.
The oral antiviral agents are more effective in reducing viral loads
in patients with
e antigen-negative
chronic hepatitis B than in
those with
e antigen-positive
chronic hepatitis B, as the pre-
treatment viral loads are lower.
Most patients with chronic hepatitis B are asymptomatic and
develop complications such as cirrhosis and hepatocellular
carcinoma only after many years (see Fig. 23.24). Cirrhosis
develops in 15–20% of patients with chronic HBV over 5–20 years
.
This proportion is higher in those who are e antigen-positive.
Two different types of drug are used to treat
hepatitis B: direct-acting nucleoside/nucleotide
analogues and pegylated interferon-alfa
.
*Direct-acting nucleoside/nucleotide antiviral agents
Orally administered nucleoside/nucleotide antiviral agents are the
mainstay of therapy. These act by inhibiting the
reverse
transcription of pre-genomic RNA to HBV-DNA by HBV-DNA
polymerase but do not directly affect the cccDNA (covalently
closed circular DNA) template for viral replication
,
and so relapse
is common if treatment is withdrawn
. One major concern is the
selection of antiviral-resistant mutations with long-term
treatment. This is particularly important with some of the older
agents, such as lamivudine, as mutations induced by previous
antiviral exposure may also induce resistance to newer agents.
Entecavir and tenofovir are potent antivirals with a high barrier to
genetic resistance, and so are the most appropriate first-line
agents.

1. Lamivudine. Although effective, long-term therapy is often
complicated by the development of HBV-DNA polymerase
mutants (e.g. the ‘YMDD variant’), which may occur after 9
months and are characterised by a rise in viral load during
treatment.
2. Telbivudine is more potent but is also susceptible to viral
resistance.
3. Adefovir is associated with development of HBV-DNA mutants
at a lower rate than with lamivudine; 2% are identified after 2
years of treatment but this figure increases to
18% after 3 years.
4. Entecavir and 5.tenofovir. Monotherapy with entecavir or
tenofovir is more effective than either lamivudine or adefovir in
reducing viral load in HBeAg-positive and HBeAg-negative chronic
hepatitis. Antiviral resistance mutations occur in
only 1–2% after 3
years
of entecavir drug exposure. Both drugs have anti-HIV action
and so their use as monotherapy is contraindicated in HIV-positive
patients, as it may lead to HIV antiviral drug resistance.

*
Interferon-alfa: this
is most effective in patients with
a low viral load and serum transaminases greater than twice the
upper limit of normal, in whom it acts
by augmenting a native
immune response
.
In HBeAg-positive chronic hepatitis, 33% lose e antigen after 4–6
months of treatment, compared to 12% of controls
. Response
rates are lower in HBeAg-negative chronic hepatitis, even when
patients are given longer courses of treatment.
Interferon is contraindicated in the presence of cirrhosis
, as it may
cause a rise in serum transaminases and precipitate liver failure.
Longer-acting pegylated interferons that can be given once
weekly have been evaluated in both HBeAgpositive and HBeAg-
negative chronic hepatitis.
Side-effects are common and include fatigue, depression,
irritability, bone marrow suppression and the triggering of
autoimmune thyroid disease.


Liver transplantation
Historically, liver transplantation was contraindicated in
hepatitis B because infection often recurred in the graft.
However, the use of post-liver transplant prophylaxis with
direct-acting antiviral agents and hepatitis B
immunoglobulins has reduced the re-infection rate to 10%
and increased 5-year survival to 80%, making
transplantation an acceptable treatment option.

Prevention:
Individuals are most infectious when markers of continuing
viral replication, such
as HBeAg, and high levels of HBV
-
DNA are present in the blood.
HBV-DNA can be found in
saliva, urine, semen and vaginal
secretions
.
The virus is about ten times more infectious than hepatitis
C, which in turn is about ten times more infectious than
HIV
.

A recombinant hepatitis B vaccine containing HBsAg is available
(Engerix
) and is capable of producing active immunisation
in 95%
of normal individuals
. The vaccine should be offered to those at
special risk of infection who are not already immune, as
evidenced by anti-HBs in the blood (Box 23.46). The vaccine is
ineffective in those already infected by HBV. Infection can also be
prevented or minimised by the intramuscular injection of
hyperimmune serum globulin prepared from blood containing
anti-HBs. This should be given within 24 hours, or at most a week,
of exposure to infected blood in circumstances likely to cause
infection (e.g. needlestick injury, contamination of cuts or mucous
membranes).
Vaccine can be given together with hyperimmune globulin
(active–passive immunisation). Neonates born to hepatitis B-
infected mothers should be immunised at birth and given
immunoglobulin. Hepatitis B serology should then be checked at
12 months of age.


At-risk groups meriting hepatitis B Vaccination in low-
endemic areas
Parenteral drug users
Men who have sex with men
Close contacts of infected individuals
Newborn of infected mothers
Regular sexual partners
Patients on chronic hemodialysis
Patients with chronic liver disease
Medical, nursing and laboratory personnel

Hepatitis D (Delta virus)
The hepatitis D virus (HDV) is an RNA-defective virus that has no
independent existence; it requires HBV for replication and has the
same sources and modes of spread. It can infect individuals
simultaneously with HBV, or can superinfect those who are
already chronic carriers of HBV. Simultaneous infections give rise
to acute hepatitis, which is often severe but is limited by recovery
from the HBV infection. Infections in individuals who are chronic
carriers of HBV can cause acute hepatitis with spontaneous
recovery, and occasionally simultaneous cessation of the chronic
HBV infection occurs. Chronic infection with HBV and HDV can
also occur, and this frequently causes rapidly progressive chronic
hepatitis and eventually cirrhosis. HDV has a worldwide
distribution. It is endemic in parts of the Mediterranean basin,
Africa and South America, where transmission is mainly by close
personal contact and occasionally by vertical transmission from
mothers who also carry HBV. In non-endemic areas, transmission
is mainly a consequence of parenteral drug misuse.

Investigations
: HDV contains a single antigen to which
infected individuals make an antibody (anti-HDV). Delta
antigen appears in the blood only transiently, and in
practice diagnosis depends on detecting anti-HDV.
Simultaneous infection with HBV and HDV followed by full
recovery is associated with the appearance of low titres of
anti-HDV of IgM type within a few days of the onset of the
illness. This antibody generally disappears within 2 months
but persists in a few patients. Superinfection of patients
with chronic HBV infection leads to the production of high
titres of anti-HDV, initially IgM and later IgG. Such patients
may then develop chronic infection with both viruses, in
which case anti-HDV titres plateau at high levels.
Management
: Effective management of hepatitis B
prevents hepatitis D.

Other forms of viral hepatitis
Non-A, non-B, non-C (NANBNC) or non-A–E hepatitis is the
term used to describe hepatitis thought to be due to a virus
that is not HAV, HBV, HCV or HEV. Other viruses that affect
the liver probably exist, but the viruses described above
now account for the majority of hepatitis virus infections.
Cytomegalovirus and EBV infection cause abnormal LFTs in
most patients, and occasionally jaundice occurs. Herpes
simplex is a rare cause of hepatitis in adults, and most of
these patients are immunocompromised. Abnormal LFTs
are also common in chickenpox, measles, rubella and acute
HIV infection.

HIV infection and the liver:
Several causes of abnormal LFTs occur in HIV infection:
Hepatitic blood tests
• Chronic hepatitis C
• Chronic hepatitis B
• Antiretroviral drugs
• Cytomegalovirus
Cholestatic blood tests
• Tuberculosis
• Atypical mycobacterium
• Sclerosing cholangitis due to cryptosporidia

