Paramyxoviruses
د.انتظار علاوي جعفرPhD. MSc. Microbiology
College of Medicine/ Thi-qar University
Microbiology department 2019-2020
Third stage
Virology
Introduction
Paramyxoviruses are roughly spherical-shaped viruses and usually vary in size from 100 to 300 nm.These viruses consist of a negative-sense single-stranded RNA genome enclosed in a helical nucleocapsid surrounded by a pleomorphic envelope.
Classification
The family Paramyxoviridae consists of three important genera1-Morbillivirus
2-Paramyxovirus
3-Pneumovirus
which contain important human pathogens responsible for causing most of acute respiratory infections and contagious diseases of children and infants.
Classification
The genus Morbillivirus includes the measles virus.The genus Paramyxovirus includes parainfluenza and mumps virus.
The genus Pneumovirus includes respiratory syncytial virus (RSV), which is responsible for majority of acute respiratory infections in infants and children
Diseases associated with some paramyxoviruses
Measles virusDisease
Measles virus
Measles, atypical measles, and subacute
sclerosing panencephalitis
Human paramyxovirus
HPIV-1,
and HPIV-3
HPIV-2,
Croup and pneumonia
• HPIV-3, and HPIV-4
Bronchiolitis and tracheobronchitis
Mumps virus
Mumps
Respiratory syncytial virus
Upper and lower respiratory tract infection, common cold
Nipah virus
Encephalitis
Measles virus
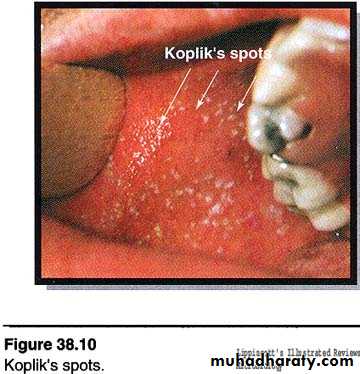
Measles is a highly communicable acute viral disease characterized by fever, conjunctivitis, and pathognomonic Koplik’s spots. It is one of the five classic exanthematous diseases of the childhood; others being chickenpox, rubella and roseola.Morphology
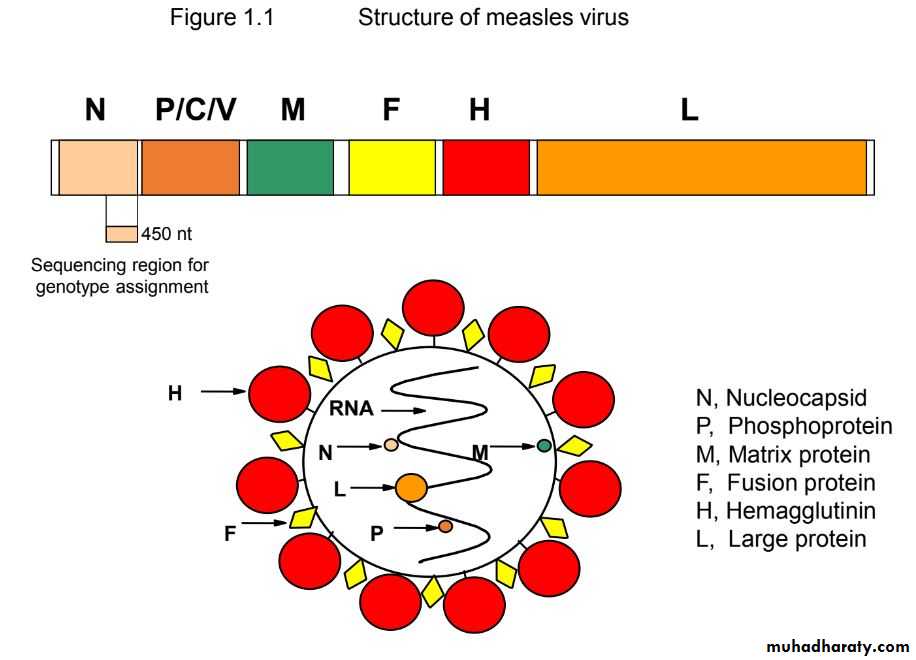
Measles virus is spherical, but is often pleomorphic, measuring 120–250 nm in diameter. It contains a negative-sense RNA genome. The helical nucleocapsid is surrounded by an envelope carrying H and F proteins on its surface.Viral replication
Measles virus replicates in the cell cytoplasm. The virus first adsorbs cell surface by its hemagglutinin, then enters the cell, and uncoats inside the cytoplasm of the cell. The viral RNA polymerase transcribes the negative-strand genome into mRNA. Multiple copies of mRNAs are produced, each of which is translated into specific viral proteins. This is followed by the assembly of nucleocapsid, and the virus is released by budding from the cell membrane.Antigenic and genomic properties
The measles virus has only one serotype and infects only humans, not any other mammals. The virus is antigenically uniform.Other Properties
The measles virus is heat labile. It is readily inactivated by ether, formaldehyde, high temperature, and ultraviolet light.
The virus resists heating at 50°C for 1 hour.
Clinical Syndromes
Incubation period varies from 8 to 12 days. Measles is a highly contagious febrile illness. The prodromal phase is characterized by high fever, malaise, anorexia, conjunctivitis, cough, and coryza. Koplik’s spot is the typical pathogenic lesion found in the mucous membrane. These are bluish gray grain substance on a red base, which usually appear on the buccal mucosa opposite the second molar. are pathognomonic of measles. Their presence establishes the diagnosis of measles.Boy with Measles
AB
Clinical Syndromes
An erythematous maculopapular rash appears within 12–24 hours of appearance of the Koplik’s spots. The rash usually begins on the face, then spreads extensively and appears on the trunk, extremities, palms, and soles and lasts for about 5 days.Desquamation of the rashes except those of palms and soles may occur after 1 week.
Pathogenesis and Immunity
The virus initiates infection and replicates locally in the trachea and bronchial epithelial cells of the respiratory tract. After 2–4 days, the virus spreads systemically in lymphocytes, perhaps carried by pulmonary macrophages, and causes viremia.Wide dissemination of the virus causes infection of the conjunctiva, respiratory tract, urinary tract, lymphatic system, blood vessels, and the central nervous system (CNS). The characteristic rash seen in measles is caused primarily by cytotoxic T cells attacking the measles virus-infected epithelial cells in the skin.
Key Points
Encephalitis is one of the most important sequelae of the infection caused by measles. The virus causes:Encephalitis by direct infection of the neurons;
Immune-mediated conditions, such as postinfectious measles encephalopathy, believed to be immune mediated.
Transmission of infection
Infected respiratory droplets are the primary source of infection. Patients are infectious from 3 days before the onset of illness until the rash desquamates. Infectivity is maximum at the prodrome and diminishes rapidly with the onset of the rash. The infection is transmitted from person to person by inhalation of large droplet aerosols produced during the act of coughing and sneezing.Diagnosis
The clinical manifestations of typical measles cases are so characteristic that the diagnosis is self-evident.Prevention and Control
Measles vaccine along with mumps and rubella (MMR) vaccine is currently used for universal immunization of children.
Vaccines
Measles vaccine is a live attenuated vaccine,The first dose of vaccine is given to children older than 12 months in the United States, but are used for children aged 9 months in developing countries with high endemicity.
The second dose of the vaccine is given usually to school going children aged 4–6 years.
Mumps Virus
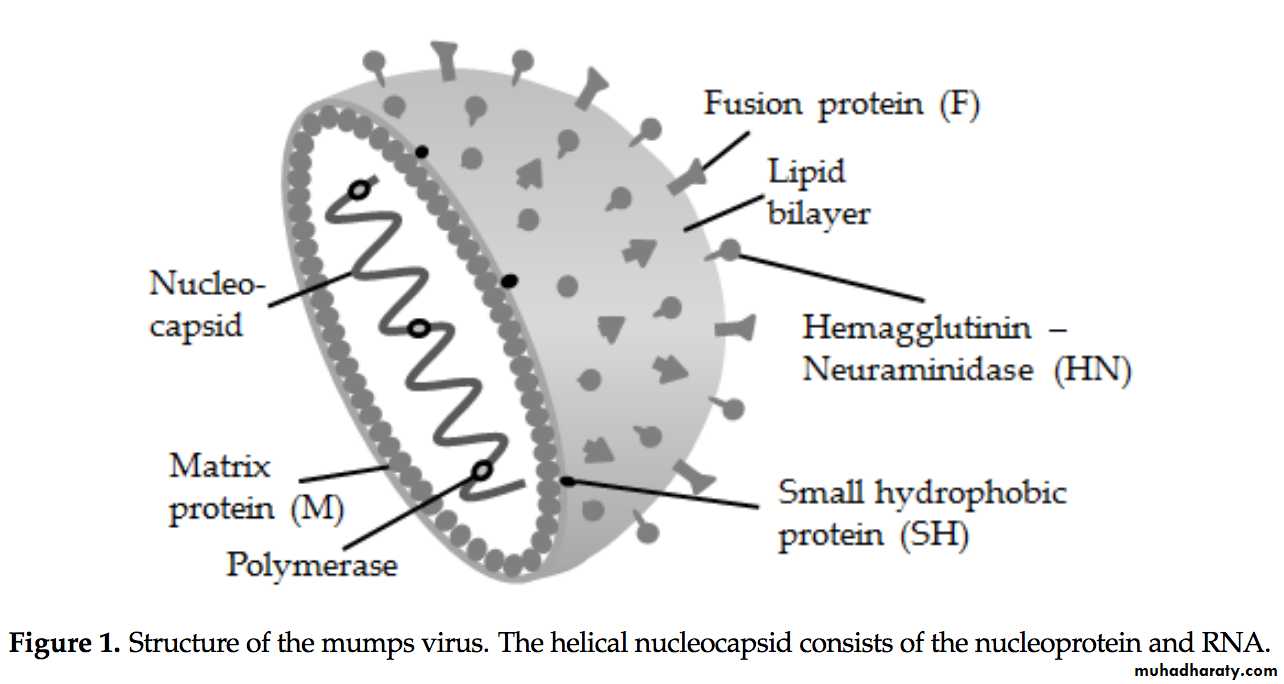
Mumps is an acute infectious disease of children, characterized by acute, nonsuppurative, painful swelling of the salivary glands (parotid gland), caused by mumps virus.Morphology
Mumps virus is a typical paramyxovirus containing a single stranded, negative-sense RNA surrounded by an envelope.It has two major surface glycoproteins:
(a) one with both hemagglutinin and neuraminidase and
(b ) the other with cell-fusion protein. The F protein is responsible for fusion of lipid membrane of the virus to the host cell.
Beleni & Borgmann, 2018
Antigenic and genomic properties
Only one antigenic type of mumps virus is known. Neutralizing antibodies are produced against the hemagglutinin.The mumps virus is a heat-labile virus. It is sensitive to heat and rapidly inactivated at room temperature.
Treatment with formaldehyde, ether, or ultraviolet light also inactivates the virus.
Other properties
Pathogenesis of mumps
Infection by mumps virus begins after the entry of the virus into the respiratory tract. The virus then replicates locally and disseminates by blood circulation to target tissues, such as the CNS and salivary glands, particularly the parotid glands by viremia. Salivary glands, such as parotid glands, show desquamation of necrotic epithelial cells lining the ducts. The virus replicates in these target tissues and then causes a secondary phase of viremia. The virus is spread by viremia throughout the body .Clinical Syndrome
The incubation period is long and varies from 12 to 25 days. Most of the infections are asymptomatic. The onset of mumps is sudden.Fever, headache, and earache are the initial symptoms. These symptoms are followed by painful swelling of the parotid gland. Initially, it may be unilateral but may become bilateral later. The condition is accompanied by fever, local pain, and tenderness.
Epididymo-orchitis is the second most common manifestation in adults, which is usually preceded by parotitis. Orchitis may occasionally cause testicular atrophy and sterility.
Complications of mumps: Meningoencephalitis is the most frequent complication of mumps in childhood.
Transmission of infection
The infected patients are the source of infection. A patient remains infectious usually from 9 days prior to the onset of parotid swelling as long as 7 days after onset of the swelling.The infection is transmitted by direct person-to-person contact and also by inhalation of respiratory droplets. The unvaccinated people and immunocompromised people are at more risk to infection by mumps virus.
Laboratory Diagnosis
Diagnosis of mumps is usually clinical. The laboratory diagnosis is useful for diagnosis of atypical infection or manifestation of mumps without typical symptoms.Human parainfluenza viruses (HPIVs)
HPIVs are single-stranded, enveloped RNA viruses of the Paramyoviridaie family. There are four serotypes which cause respiratory illnesses in children and adults. HPIVs bind and replicate in the ciliated epithelial cells of the upper and lower respiratory tract and the extent of the infection correlates with the location involved. Seasonal HPIV epidemics result in a significant burden of disease in children and account for 40% of pediatric hospitalizations for lower respiratory tract illnesses and 75% of croup cases.Source: Branche and Falsey, 2014
Parainfluenza Virus
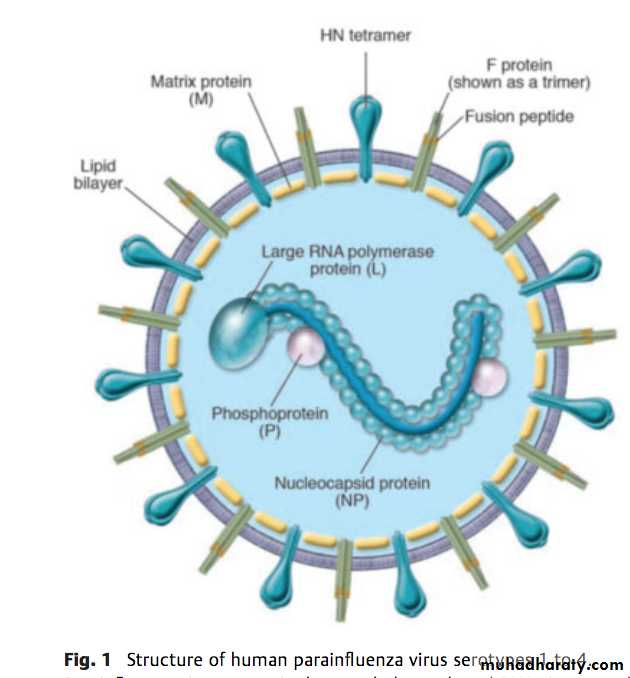
Parainfluenza viruses are pleomorphic viruses measuring 150–200 nm in diameter.The virus contains a single-stranded, nonsegmented, negative- sense RNA genome with nucleoproteins P and L. It is surrounded by a helical nucleocapsid, which contains glycoprotein spikes.
The surface spikes consist of H, N (neuraminidase), and F proteins. Both H and N proteins are present on the same spike, whereas the F protein is present on a separate spike.
The F protein mediates the formation of multinucleated giant cell.
Source: Branche and Falsey, 2014
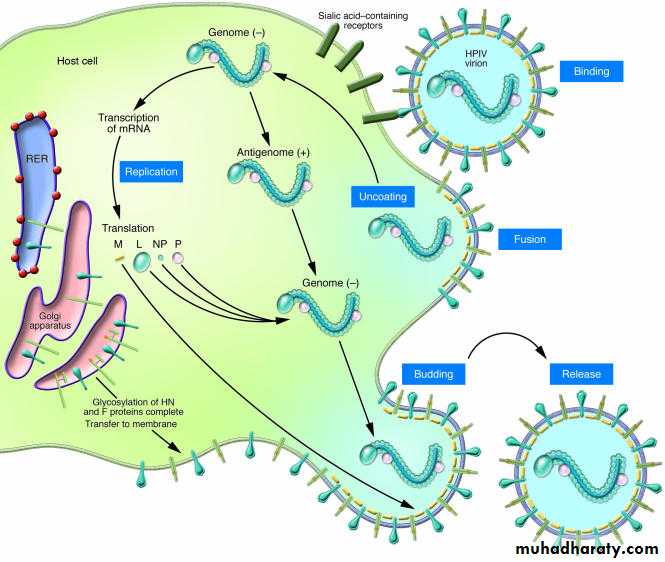
Pathogenesis of human parainfluenza virus (HPIV) infection
The virus adsorbs to the respiratory epithelial cells by specifically combining with neuraminic acid receptors in the cell through its hemagglutinin. Subsequently, the virus enters the cells following fusion with the cell membrane, mediated by F1 and F2 receptors. The virus replicates rapidly in the cell cytoplasm and causes formation of multinucleated giant cells. The virus also causes the formation of single and multilocular cytoplasmic vacuoles and basophilic or eosinophilic inclusions.The virus causes inflammation of the respiratory tract, leading to secretions of high level of inflammatory cytokines, usually 7–10 days after initial exposure. Airways inflammation, necrosis, and sloughing of respiratory epithelium, edema, and excessive mucus production are the noted pathological features associated with HPIV infections.
Moscona A. (2005).
HIPV replication cycle
Clinical SyndromesHuman parainfluenza viruses cause croup
(a heterogeneous group of illnesses that affects the larynx, trachea, and bronchi. The condition manifests as fever, cough, laryngeal obstruction), pneumonia, bronchiolitis and tracheobronchitis, and Otitis media, pharyngitis, conjunctivitis.
Reservoir, source, and transmission
of infectionParainfluenza viruses cause disease exclusively in humans. No animal reservoirs are present. Respiratory secretions from the infected humans are the source of infection. The infection is transmitted by inhalation of respiratory droplets or by direct person-to-person contact with infected secretions.
Laboratory Diagnosis
Respiratory specimens include nasopharyngeal aspirations nasal washings, and nasal aspirations1- Direct antigen detection
The ELISA, immunofluorescence assay are used to detect HPIV antigen.
2-Molecular Diagnosis: A multiplex reverse transcriptase polymerase chain reaction (RT-PCR) has been developed for simultaneous detection of
HPIV-1, HPIV-2, and HPIV-3 genome in clinical specimens.
Prevention and Control
Currently there is no vaccine against infection by HPIV, However, researchers are trying to develop one.• The risk of HPIV and other respiratory viral infections could be reduced by:
• washing your hands often with soap and water for at least 20 seconds.• avoiding touching your eyes, nose, or mouth.
• avoiding close contact with people who are sick.