ACUTE LUNG INJURY:
Include:Pulmonary edema:
The condition defined as fluid accumulation in the tissue and air spaces of the lung it leads to impaired gas exchange and may cause respiratory failure.
MORPHOLOGY
pulmonary congestion and edema are characterized by heavy, wet lungs. Fluid accumulates initially in the basal regions of the lower lobes because hydrostatic pressure is greater in these sites (dependent edema).
Histologically : the alveolar capillaries are engorged, and an intra-alveolar granular pink precipitate is seen, alveolar micro-hemorrhages and hemosiderin-laden macrophages ("heart failure" cells) may be present.
ACUTE RESPIRATORY DISTRESS SYNDROME (DIFFUSE ALVEOLAR DAMAGE)
Acute respiratory distress syndrome (ARDS) is a clinical syndrome caused by diffuse alveolar capillary damage, it is characterized clinically by the rapid onset of severe life-threatening respiratory insufficiency, cyanosis, and severe arterial hypoxemia that is refractory to oxygen therapy and that may progress to extra-pulmonary multisystem organ failure.ARDS is a well-recognized complication of numerous and diverse conditions, including both direct injuries to the lungs and systemic disorders. In many cases, a combination of predisposing conditions is present (e.g., shock, oxygen therapy, and sepsis).
Morphology.
They exhibit congestion, interstitial and intra-alveolar edema, inflammation, and fibrin deposition. The alveolar walls become lined with waxy hyaline membranes . Alveolar hyaline membranes consist of fibrin-rich edema fluid mixed with the cytoplasmic and lipid remnants of necrotic epithelial cells, resolution is unusual; more commonly, there is organization of the fibrin exudate, with resultant intra-alveolar fibrosis.
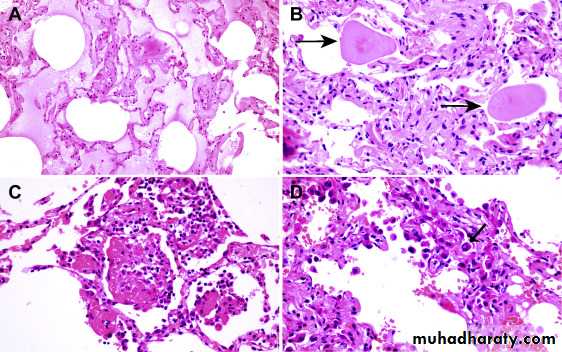
Acute lung injury and acute respiratory distress syndrome.
(A) Diffuse alveolar damage in the acute phase. Some alveoli are collapsed,while others are distended; many are lined by bright pink hyaline membranes
(arrow). (B) The healing stage is marked by resorption of hyaline membranes
and thickening of alveolar septa by inflammatory cells, fibroblasts, and collagen.
Numerous reactive type II pneumocytes also are seen at this stage
(arrows), associated with regeneration and repair.
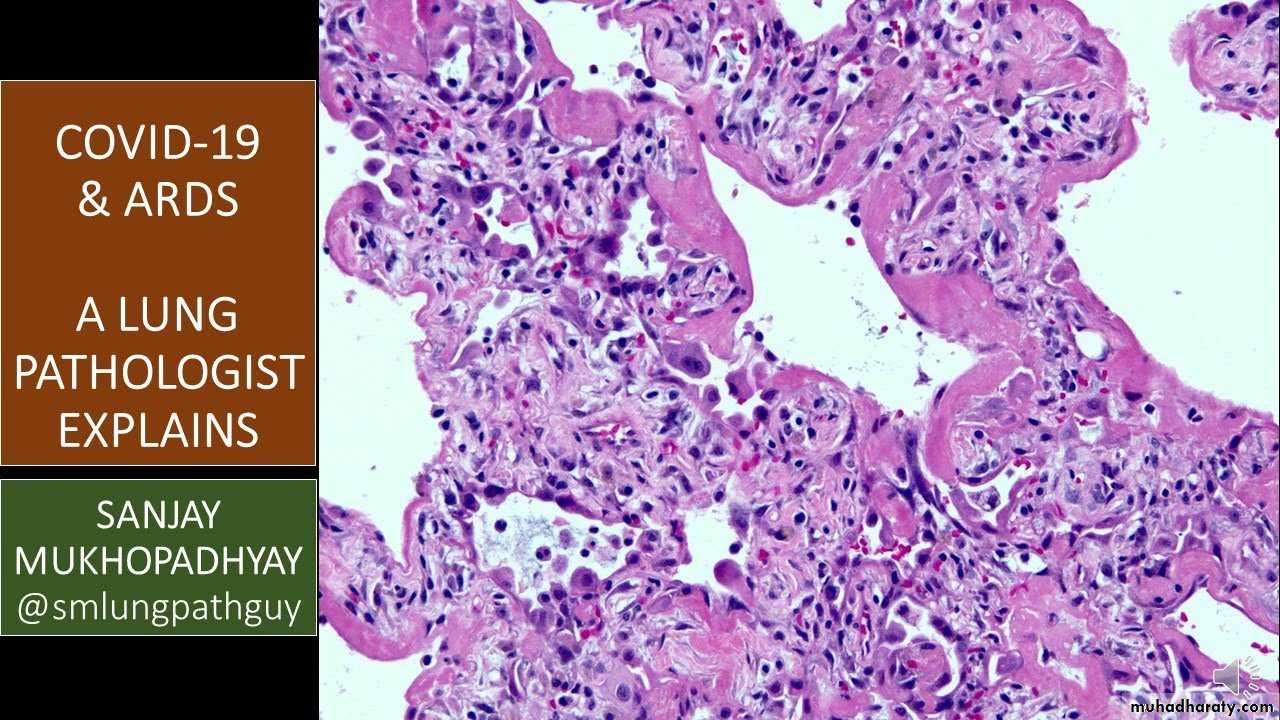
the pulmonary pathology of patient with COVID 19 infection
Lung is the most common site of infection for new global COVID 19 virus, which manifest as acute respiratory distress syndrome and mortality, pulmonary involvement is also responsible for the high viral transmission, analysis of the pathological features in the lung tissues of patients who have died with COVID-19 could help us to understand the disease pathogenesis and clinical outcomes.
The important pathological changes seen in patent died from COVID 19 infection Interstitial inflammation, diffuse alveolar damage, and necrotizing bronchitis/bronchiolitis are general histopathological findings of lung in respiratory viral infections, diffuse alveolar damage is the most commonly observed finding with respiratory virus infections both in acute and late (organizing) stages, The characteristic features of acute diffuse alveolar damage are intra-alveolar edema. Fibrin deposition and formation of hyaline membranes lining the alveolar walls follow. Late diffuse alveolar damage stages are Type II pneumocyte proliferation, granulation tissue formation, followed by collagen deposition.
The pathogenesis of COVID 19 begins with virus interaction with host cells through the binding of its envelope protein (spike; S) to angiotensin-converting enzyme 2 (ACE-2), the corresponding receptor. ACE-2 is abundantly expressed on the surface of lung and intestinal epithelial cells .
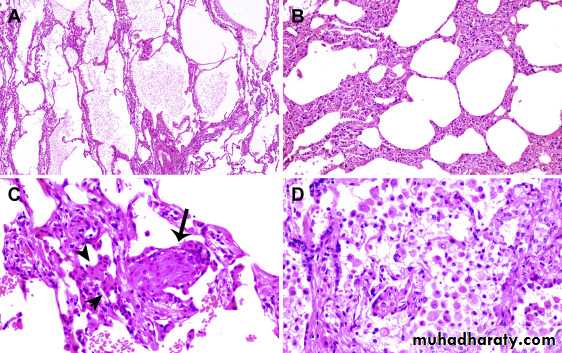
Histologic changes from case 1. (A) Proteinaceous exudates in alveolar spaces, with granules; (B) scattered large protein globules (arrows); (C) intra-alveolar fibrin with early organization, mononuclear inflammatory cells, and multinucleated giant cells; (D) hyperplastic pneumocytes, some with suspected viral inclusions (arrow).
(A) Evident proteinaceous and fibrin exudate; (B) diffuse expansion of alveolar walls and septa owing to fibroblastic proliferations and type II pneumocyte hyperplasia, consistent with early diffuse alveolar damage pattern; (C) plugs of proliferating fibroblasts or “fibroblast balls” in the interstitium (arrow); (D) abundant macrophages infiltrating airspaces and type II pneumocyte hyperplasia.
PULMONARY INFECTIONS:
Respiratory tract infections are more frequent than infection of any other organ. The vast majority are upper respiratory tract infections caused by viruses (common cold, pharyngitis) but bacterial, viral, mycoplasmal, fungal infections of the lung (pneumonia) still account enormous amount of morbidity and are responsible sixth of all deaths in the United States. Pneumonia very broadly defined as any infection of the lung parenchyma (although the same term is used for many interstitial lung diseases that are not infectious in origin, such as interstitial pneumonia).COMMUNITY-ACQUIRED ACUTE PNEUMONIAS
Community-acquired pneumonias may be bacterial or viral. Often, the bacterial infection follows an upper respiratory tract viral infection. Bacterial invasion of the lung parenchyma causes the alveoli to be filled with an inflammatory exudate, thus causing consolidation (“solidification”) of the pulmonary tissue.
Morphology.
Bacterial pneumonia has two gross patterns of anatomic distribution: lobular bronchopneumonia and lobar pneumonia. Patchy consolidation of the lung is the dominant characteristic of bronchopneumonia. Lobar pneumonia is an acute bacterial infection resulting in fibrinosuppurative consolidation of a large portion of lung or of an entire lobe.
In lobar pneumonia, four stages of the inflammatory response have classically been described: congestion, red hepatization, gray hepatization, and resolution. Present-day effective antibiotic therapy frequently slows or halts the progression.
Bronchopneumonia:
They are consolidated areas of acute supportive inflammation. The consolidation may be patchy through one lobe , multilobular, or bilateral. Well-developed lesions are usually 3 to 4 cm in diameter, dry granular, gray red to yellow.
Histologically. Suppurative, neutrophil- rich exudates that full the bronchi, bronchioles, and adjacent alveolar spaces.