External genitalia
بسم الله الرحمن الرحيم
Dr.Sumeya
INDIFFERENT STAGEIn the third week of development, mesenchyme cells originating in the region
of the primitive streak migrate around the cloacal membrane to form a pair ofslightly elevated cloacal folds .
Cranial to the cloacal membrane the folds unite to form the genital tubercle.
Caudally the folds are subdivided
into urethral folds anteriorly and anal folds posteriorly.
In the meantime, another pair of elevations, the genital swellings, becomes visible on each side of the urethral folds.
These swellings later form the scrotal
swellings in the male and the labia majora in the female.
At the end of the sixth week, however, it is impossible to distinguish between the two sexes
A and B. Indifferent stages of the external genitalia. A. Approximately4 weeks. B. Approximately 6 weeks. C. Scanning electron micrograph of the externalgenitalia of a human embryo at approximately the seventh week. AF, anal fold; arrowhead,anal opening; GS, genital swelling; GT, genital tubercle; T, tail; UF, urethral fold.
External Genitalia in the Male
A. Development of external genitalia in the male at 10 weeks. Note thedeep urethral groove flanked by the urethral folds. B. Transverse sections throughthe phallus during formation of the penile urethra. The urogenital groove is bridgedby the urethral folds. C. Development of the glandular portion of the penile urethra.D. Newborn.Figure
A. Genitalia of a male fetus at 14 weeks, showing fusion of the scrotal
swellings (S ). Arrow, epithelial tag. B and C. Dorsal and ventral views, respectively, ofthe genitalia of a female fetus at 11 weeks. The genital tubercle at this stage is longer
than in the male (A), and the genital swellings (GS ) remain unfused.
Development of the external genitalia in the male is under the influence of androgens secreted by the fetal testes and is characterized by rapid elongation of
the genital tubercle, which is now called the phallus
During this elongation, the phallus pulls the urethral folds forward so that they form the lateral walls of the urethral groove.
This groove extends along the caudal aspect of the elongated phallus but does not reach the most distal part, the glans
The epithelial lining of the groove, which originates in the endoderm, forms the urethral plate.
At the end of the third month the two urethral folds close over the urethral plate, forming the penile urethra.
This canal does not extend to the tip of the phallus.
This most distal portion of the urethra is formed during the fourth month, when ectodermal cells from the tip of the glans penetrate inward and form a short epithelial cord.
This cord later obtains a lumen, thus forming the external urethral meatus.
The genital swellings, known in the male as the scrotal swellings, arise in the inguinal region.
With further development they move caudally, and each swelling then makes up half of the scrotum.
The two are separated by the scrotal septum
Hypospadias showing the various locations of abnormal urethralorifices. B. Patient with hypospadias. The urethra is open on the ventral surface ofthe penis. C. Epispadias combined with exstrophy of the bladder. Bladder mucosa isexposed.
External Genitalia in the Female
Estrogens stimulate development of the external genitalia of the female.
The genital tubercle elongates only slightly and forms the clitoris urethral folds do not fuse, as in the male, but develop into the labia minora.Genital swellings enlarge and form the labia majora.
The urogenital groove is open and forms the vestibule.
Although the genital tubercle does not elongate extensively in the female, it is larger than in the male during the early stages of development.
In fact, using tubercle length as a criterion (as monitored by ultrasound) has resulted in mistakes in identification of the sexes during the third and fourth months of gestation.
Development of the external genitalia in the female at 5 months (A) andin the newborn (B).
Patient with Turner syndrome, which is characterized by a 45,X chromosomecomplement. Note the absence of sexual maturation. Other typical features arewebbed neck, broad chest with widely spaced nipples, and short stature.
Patient with female pseudohermaphrodism caused by congenitaladrenal hyperplasia (adrenogenital syndrome). B. External genitalia show fusion of the labia majora and enlargement of the clitoris
Patient with androgen insensitivity syndrome, which is characterized bya 46,XY chromosome complement
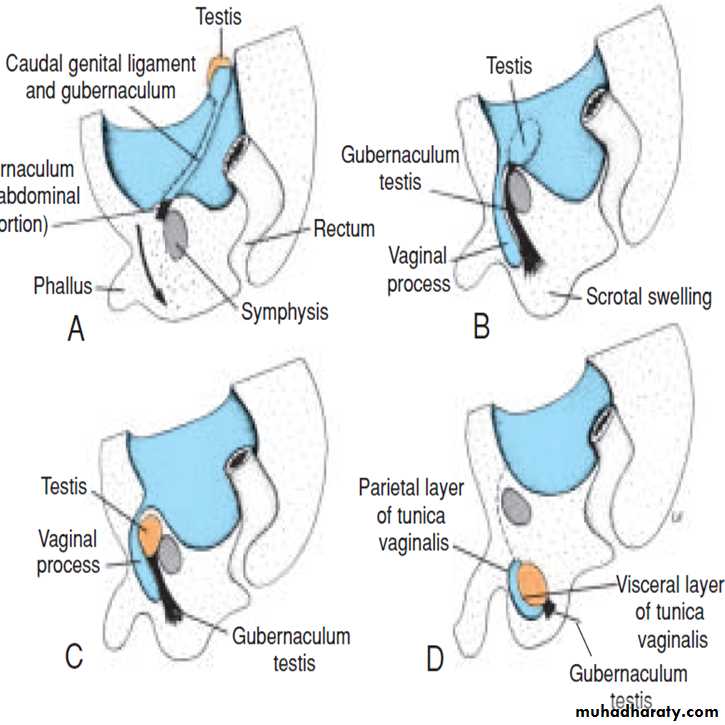
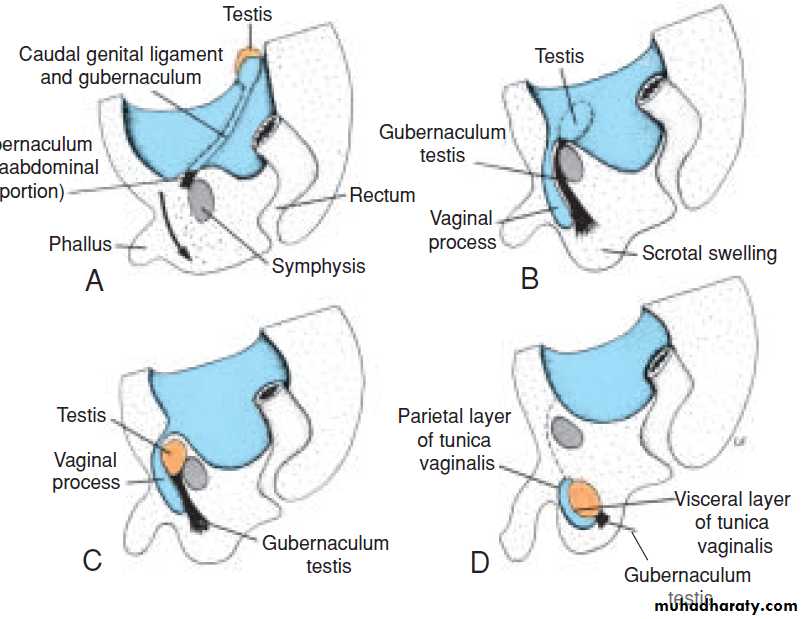
DESCENT OF THE TESTES
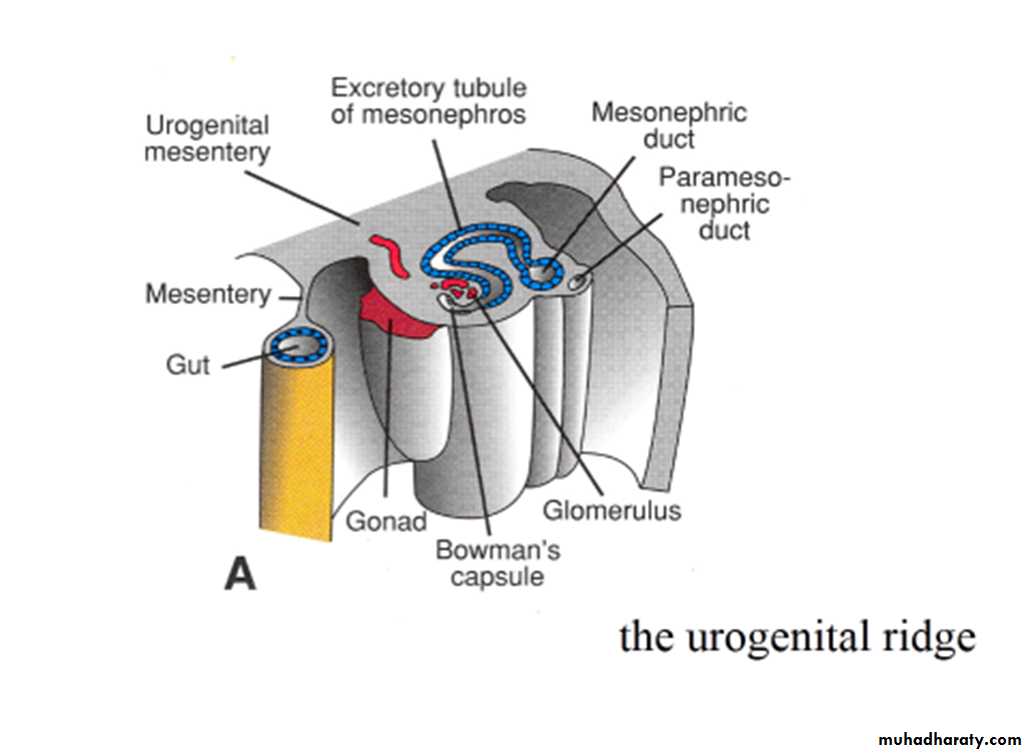
Toward the end of the second month, the urogenital mesentery attaches the testis and mesonephros to the posterior abdominal wall .
With degeneration of the mesonephros the attachment serves as a mesentery for the gonad.
Caudally it becomes ligamentous and is known as the caudal genital ligament.
Also extending from the caudal pole of the testis is a mesenchymal condensation rich in extracellular matrices, the gubernaculum.
Prior to descent of the testis, this band of mesenchyme
terminates in the inguinal region between the differentiating internal and external abdominal oblique muscles.Later, as the testis begins to descend toward the inguinal ring, an extra-abdominal portion of the gubernaculum forms and grows from the inguinal region toward the scrotal swellings.
When the testis passes through the inguinal canal, this extra-abdominal portion contacts the scrotal floor (the gubernaculum forms in females also, but in normal cases it
remains rudimentary).
Factors controlling descent of the testis are not entirely clear.
It appears, however, that outgrowth of the extra-abdominal portion of the gubernaculum produces intra-abdominal migration, that an increase in intra-abdominal pressure due to organ growth produces passage through the inguinal canal, and that regression of the extra abdominal portion of the gubernaculum completes movement of the testis into the scrotum.Normally, the testes reach the inguinal region by approximately 12weeks gestation, migrate through the inguinal canal by 28 weeks, and reach the scrotum by 33 weeks
The process is influenced by hormones, including androgens and MIS.
Descent of the testis. A. During the second month. B. In the middle of thethird month. Peritoneum lining the coelomic cavity evaginates into the scrotal swelling,where it forms the vaginal process (tunica vaginalis). C. In the seventh month. D. Shortlyafter birth.
E. Scanning electron micrograph of a mouse embryo showing the primitivegonad (G), mesonephric duct (arrowheads), and gubernaculum (arrows
In 97% of male newborns, testes are present in the scrotum before birth.
In most of the remainder, descent will be completed during the first 3 months postnatally.However, in less than 1% of infants, one or both testes fail to descend.
The condition is called cryptorchidism and may be caused by decreased androgen (testosterone) production.
The undescended testes fail to produce mature spermatozoa and the condition is associated with a 3% to 5% incidence of renal anomalies.
DESCENT OF THE OVARIES
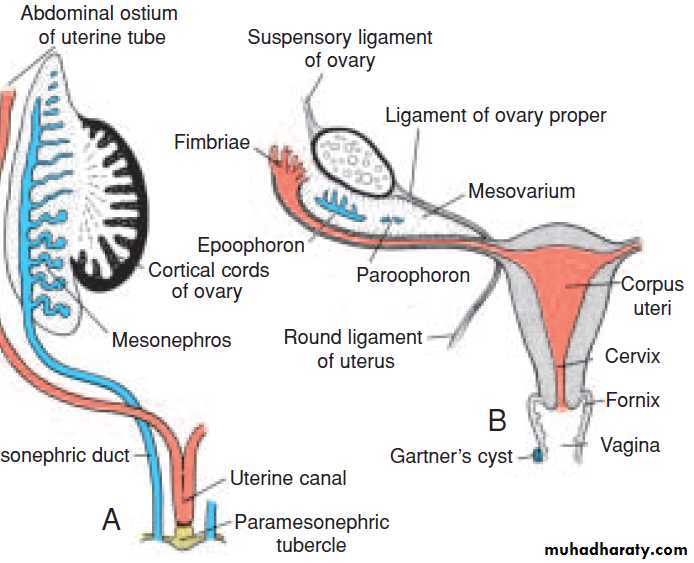
Descent of the gonads is considerably less in the female than in the male, and the ovaries finally settle just below the rim of the true pelvis.The cranial genital ligament forms the suspensory ligament of the ovary, whereas the caudal genital ligament forms the ligament of the ovary proper and the round
ligament of the uterus .the latter extends into the labia majora.