
Pulmonary circulation
Lec4
Respiratory Physiology
Dr Suroor Mohammed
Objectives
●
List the features of the pulmonary circulation.
●
List the Factors affecting pulmonary blood flow
●
Explain the Differences in ventilation &
perfusion in different parts of the lung
●
Transport forms of o2 & co2 .
●
whats mean by oxy-Hb curve
The primary function of the pulmonary circulation is to allow
the
exchange of oxygen and carbon dioxide
between the
blood in the pulmonary
capillaries
and air in
the alveoli
.
Oxygen
is taken up into the blood whilst co2 is released
from the blood into the alveoli.
Mixed-venous blood
is pumped from the right ventricle through the
pulmonary arteries and then through the pulmonary capillary network. The
pulmonary capillary network is in contact with the respiratory surface
and provides a huge gas-exchange area
.
Gaseous exchange
occurs (co2 given up by the blood, oxygen
taken up by the blood) and the
oxygenated
blood returns
through the pulmonary veins to the left atrium.
The lungs are drained by the pulmonary veins( large veins)
carry oxygenated blood from the lungs into the left atrium of
the heart
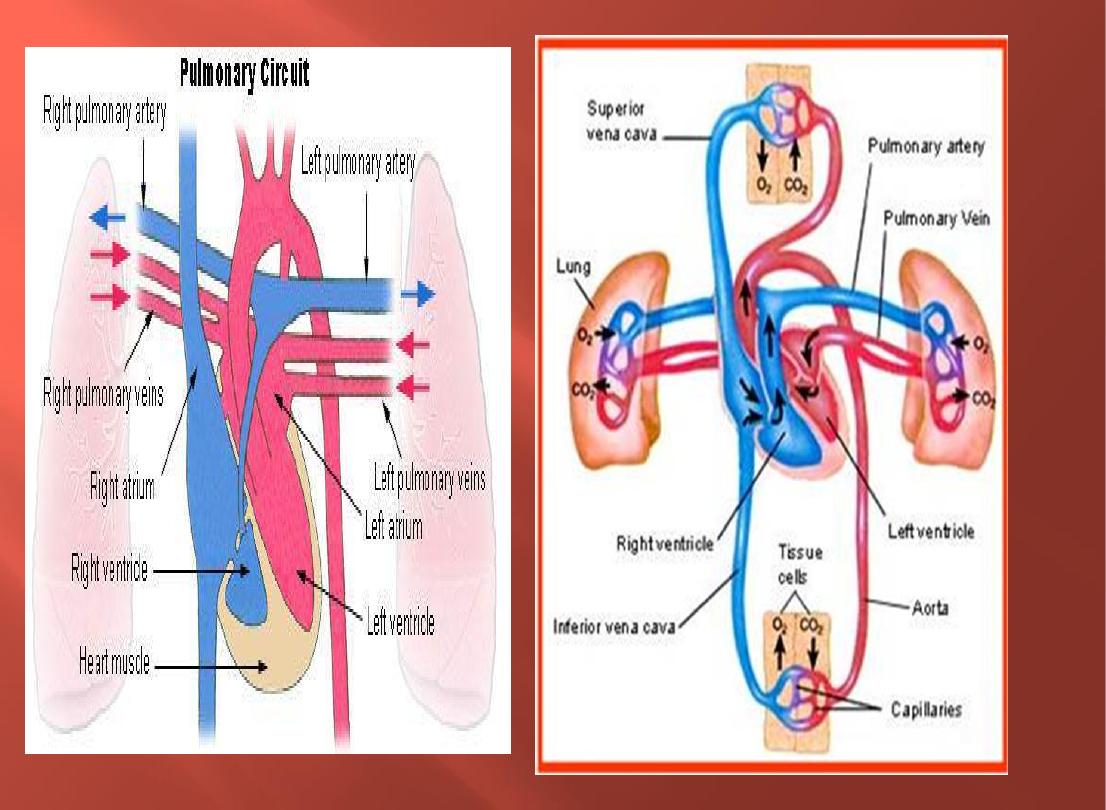

Pulmonary Circulation
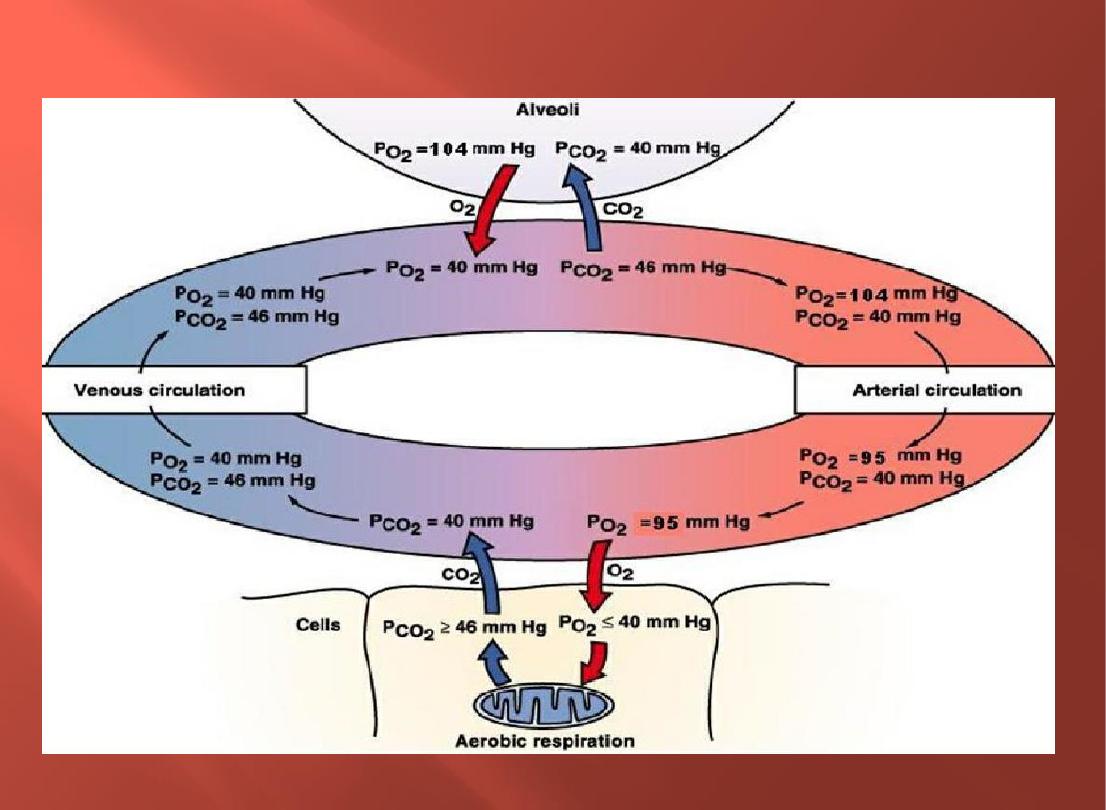
At normal P02 arterial blood is about 100 mm Hg.
● P02 level in the
systemic veins
is about
40
mm Hg.
■PC02 is
46 mm
Hg in the
systemic veins
.
■Provides a good index of lung function
●
Rate of blood flow through the pulmonary circulation is = flow rate
through the systemic circulation
. ◦ Driving pressure is about 10 mm Hg.
●
Pulmonary vascular resistance is low
. ◦ Low pressure pathway produces
less net filtration than produced in the systemic capillaries.& Avoids
pulmonary edema.
●
Autoregulation
: ◦ Pulmonary arterioles constrict when alveolar P02
decreases(hypoxia) & ◦ Matches ventilation/perfusion ratio.
In a fetus: ◦ Pulmonary circulation has a higher vascular resistance, because the lungs
are partially collapsed.
● After birth, vascular resistance decreases: ◦ Opening the vessels as a result of
subatmospheric intrapulmonary pressure.
◦ Physical stretching of the lungs.
◦ Dilation of pulmonary arterioles in response to increased alveolar P0
PULMONARY CIRCULATION
Features of pulmonary circulation
1) Lung is the only organ
receiving the entire CO
2) Less affected by
gravitational forces
compared with
systemic vessels.
3)
Pulmonary blood vessels
:
Pul arteries: thin walled (30% as thick as the wall of
the aorta) little smooth muscle and elastic tissue and
have larger diameter
Pul capillaries: larger than systemic capillaries and
denser with multiple anastomoses (each alveolus
seems to sit in a capillary basket)
Pul veins: highly dispensable and act a blood
reservoir. Lying down →↑pul blood volume (400mL)
→↓ VC & orthopnea in HF
4) Pulmonary blood pressure
Pul circulation is a low-pressure circulation (24/9mmHg). Systemic
(120/80mmHg)
Pul capillary pressure is 10mmHg (systemic=30mmHg)
5)
Pulmonary blood flow is
influenced by intrathoracic pressure.
6)
Pulmonary circulation acts as a filter
which prevents emboli from reaching
the systemic circulation (fibrinolytic system)
7) The pulmonary arteries are the
only postnatal arteries that carry
deoxygenated blood
, and pulmonary veins are the only postnatal veins
that carry oxygenated blood.
8)
Lymphatic channels are abundant
in lungs
keep alveoli dry and maintain -ve intrapleural pressure
9)
ACE
produced by endothelial cells of pulmonary vessels → maintaining
blood pr
10)
Blood vessels of lung
consist of two sets
originating from two
different sources,
performing different
functions
Pulmonary
artery
Bronchial arteries
Pulmonary circulation
Systemic circulation
Deoxygenated blood
Oxygenated blood
Gas exchange
To the respiratory tree up
to the terminal bronchioles
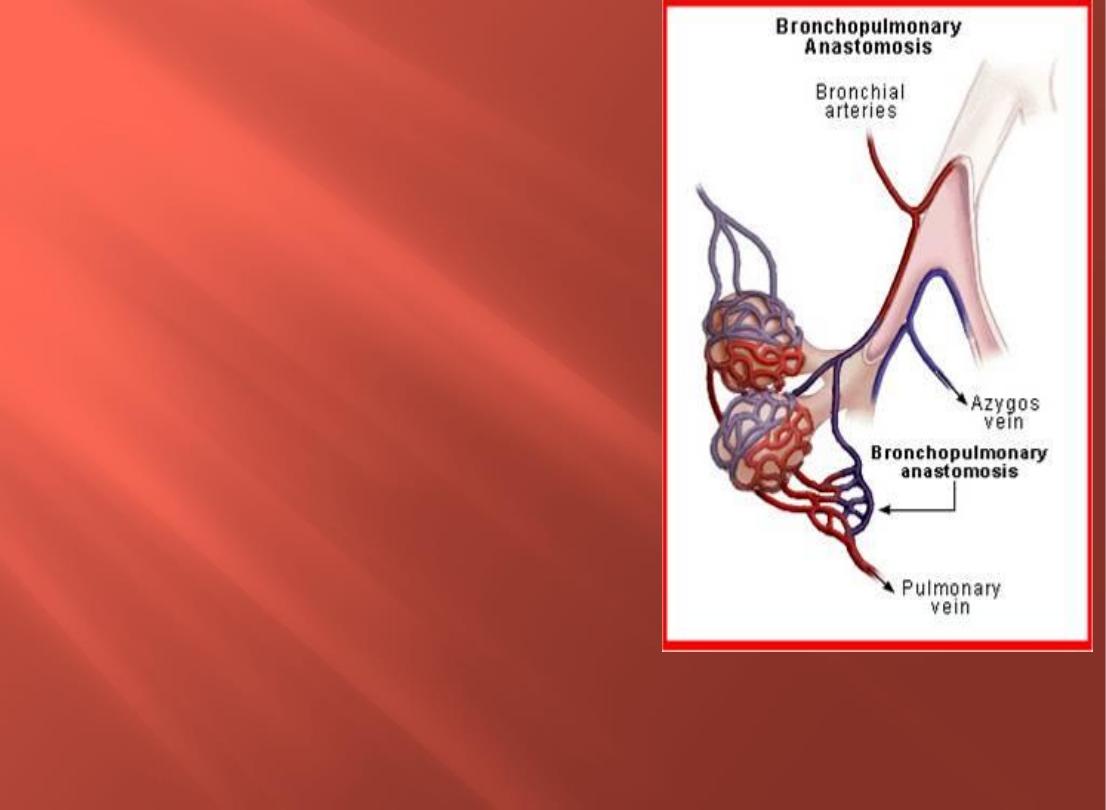
11) Physiologic shunt
●
Shunt: blood that has not been
oxygenated in the lungs is
added to systemic circulation
●
Lung: Bronchopulmonary
anastomosis.
Some bronchial venous blood (de-
oxygenated blood) enters
pulmonary veins (oxygenated
blood) bypassing the right
ventricle and returns to left side of
heart.
This constitutes 2% of blood in
systemic circulation.
PO2 of pulmonary vein (95 mmHg) is
different from that of pulmonary capillary
(104 mmHg) due to anatomic shunt
Regulation of pulmonary blood flow:
1) Cardiac out put:
↑CO → ↑ pulmonary blood flow.
2) Pulmonary vascular resistance:
Pulmonary perfusion is inversely proportional to pulmonary
vascular resistance.
3) Nervous factors:
Sympathetic → pulmonary vasoconstriction → ↓pulmonary blood
flow by (30%
Parasympathetic→ vasodilatation → ↑pulmonary perfusion.
4) Chemical factors:
Hypoxia, hypercapnia, and acidosis → vasoconstriction →↑
pulmonary arterial pressure (pul hypertension)
●
In all others areas other than lung, hypoxia produces
vasodilatation
●
COPD→ hypoxia → vasoconstriction → pulmonary
hypertension → RHF

5) Effects of gravity:
Remarkable effect on pulmonary circulation
In the erect posture (Apex of lung above the level of heart,
base below) → linear ↑ in pulmonary blood flow from the apex
to the base of the lung.
Alveoli at apex are underperfused (overventilated).
◦
Alveoli at the base are underventilated (overperfused)
6) Hormonal factors:
Pulmonary arteriolar vasoconstriction (angiotensin II,
epinephrine, norepinephrine, PGF2α)
Vasodilator (Ach, NO)
7) Phases of respiration:
Inspiration →pulmonary vasodilatation →↑ pulmonary perfusion
Expiration → vasoconstriction → ↓ pulmonary perfusion
.

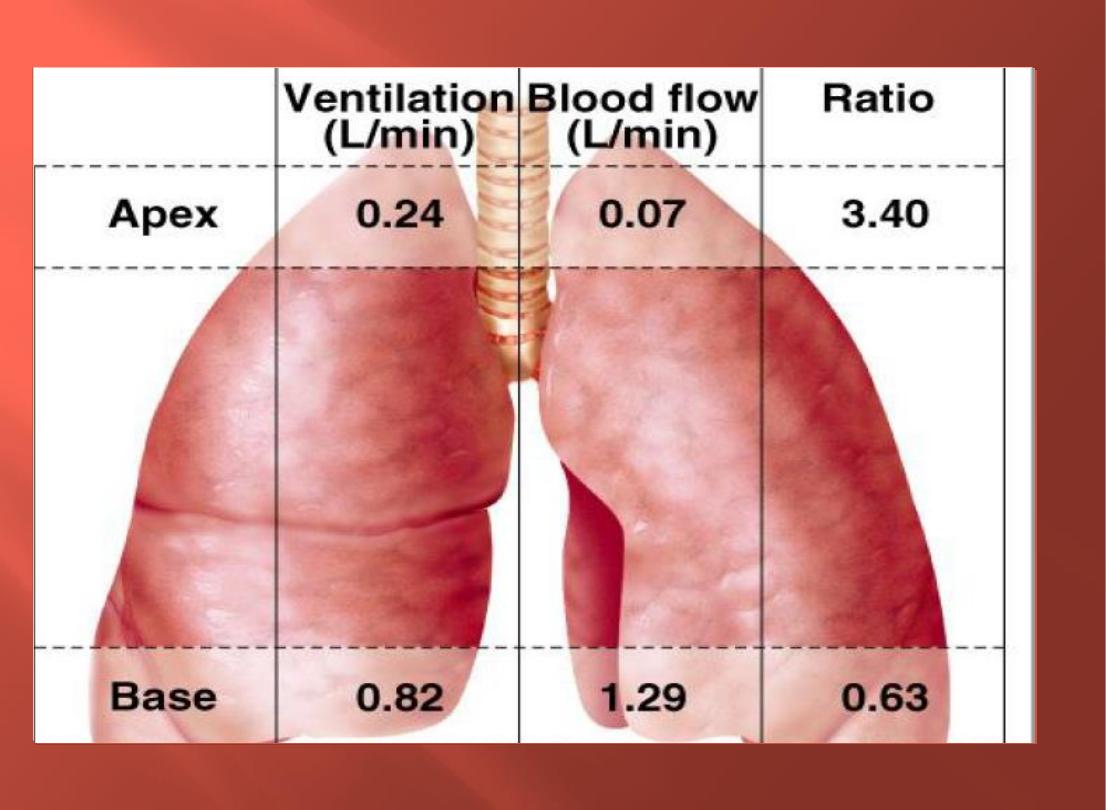
Ventilation perfusion ration(V/Q):differences
in V & Q in different parts of the lung:
●
Is the ratio between alveolar ventilation in one
min and pulmonary perfusion in one min
For proper O
2
and CO
2
exchange in the lungs, ventilation
and perfusion must be matched.
●
Resting alveolar ventilation is 4 L/min
●
Pulmonary blood flow = CO= 5L/min
V/Q=(4L/min) ÷(5L/min)=0.8 at the middle of the lung
At the apex of the lung, V/Q=3
At the base of the lung, V/Q=0.6
●
In the upright posture, ventilation and perfusion are
less at the apex and more towards the base (gravity)
In lying down posture, the posterior part of the lung is well
ventilated and perfused than the anterior part.
Various lung intravascular and extravascular pressures
influence pulmonary blood flow and its distribution in
the lung. Pressure in different vascular segments
(arteries, capillaries and veins), extravascular pressures
(intrathoracic or intrapleural), and transmural pressure
can vary considerably during both the cardiac and
respiratory cycles.
Because these pressures can influence the distribution of
blood flow and vascular resistance, they can affect how
well blood flow is matched to ventilation.
Gravity dependent reduction in perfusion is more
marked at the apex than reduction for ventilation →
V/Q is highest at the apex and lowest at the base in
upright posture
.

The pulmonary circulation
receives
the entire output of the
right heart, but
vascular pressures
are considerably
lower
than in systemic vessels.
Blood flow in the upright lung is distributed preferentially
to the lung base because of the influence of gravity.
However, the base also receives a greater proportion of the
ventilation than does the apex. This imbalance in
ventilation to perfusion in the upright lung can lead to a
higher VA/Q at the apex than the base
This is reflected by a
higher
alveolar PO2 and lower PCO2 in alveoli
at
the apex
than at lung base.
Composition of Alveolar Air is Kept Constant
(Po
2 =
100mHg,
Pco
2 =
40mHg)
O
2
continuously diffuses out of the alveoli into the blood stream and CO
2
continuously diffuses into the alveoli from blood
Inspired air mixes with alveolar air, replacing the O
2
and diluting the CO
2
.
●
The blood transports O
2
and CO
2
between the lungs and other tissues
throughout the body.
●
These gases are carried in several different forms:
Dissolved in plasma
Chemically combined with Hb.
Converted into a different molecule
Oxygen Transport:
* 98. % combines with hemoglobin (oxy –Hb )in RBC (Hb increases the O
2
carrying
capacity of blood 70-fold).
* 2 % dissolved in plasma
Transport of CO
2
in the blood
while
CO2 is transported in 3
forms:
- In the form of HCO3 carbonic acid …. 70%
-
- In dissolved in plasma …………... 7%
-
With Hb proteins as carbamino compounds (23%):
CO2 combines reversibly with Hb to form carbamino
Hb
CO2 + Hb Hb-CO2
CO2 does not bind to iron
, as oxygen does, but to amino groups on the polypeptide
chains of Hb & of plasma proteins
.
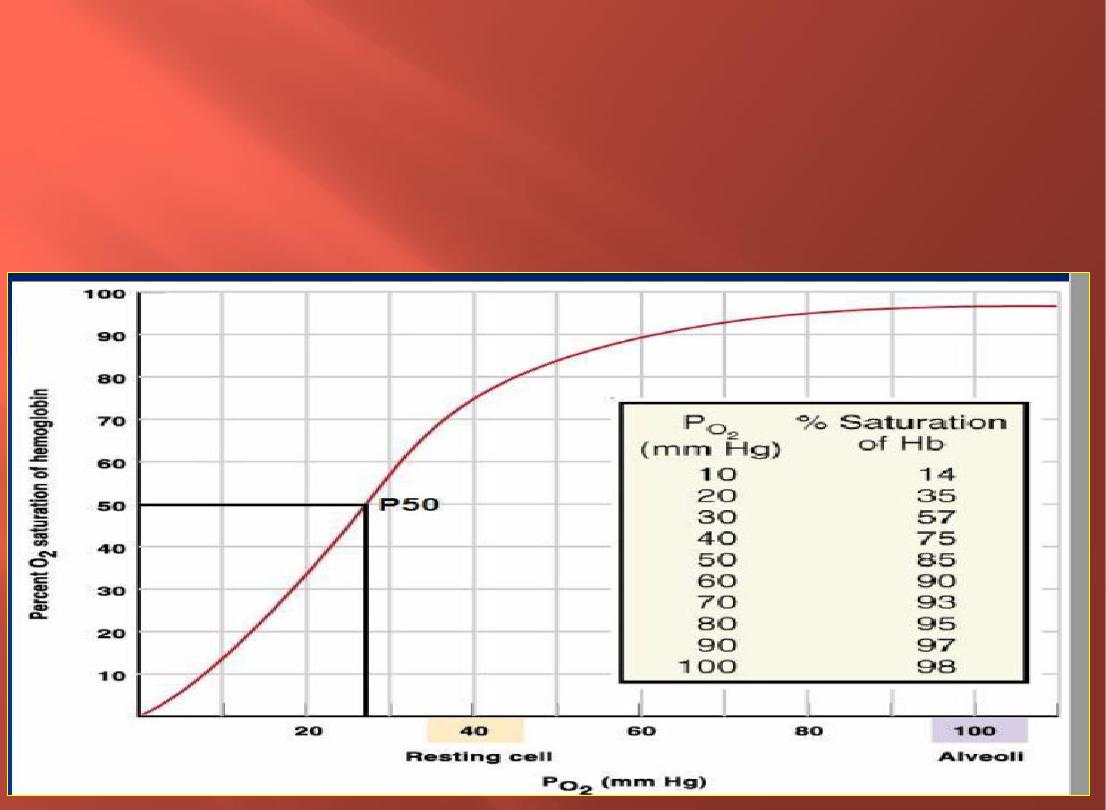
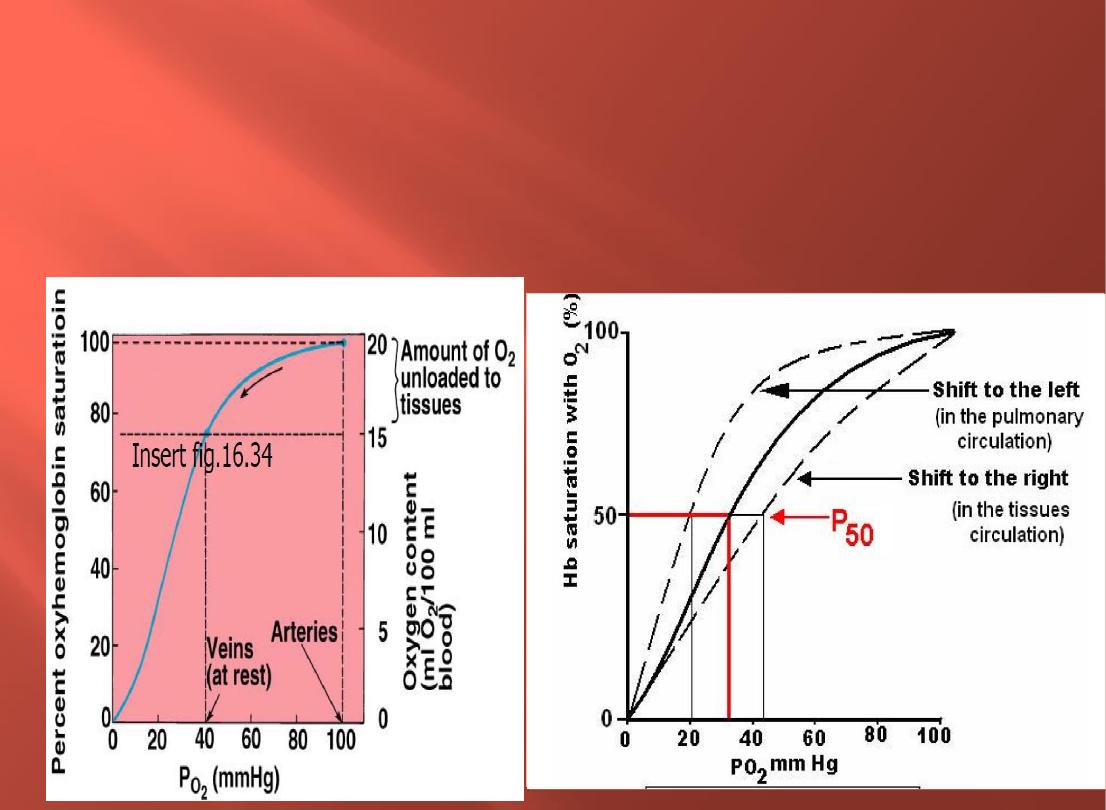
Oxyhemoglobin Dissociation Curve
It is an S - shaped curve with a steep slope between 10 and 60 mm Hg P0
2
and a flat portion between70 and 100 mm Hg P0
2
. At a P0
2
of 60 mm Hg, 90%
of the total Hb is combined with 0
2.
From this point on, a further increase in P0
2
produces only a small increase in 0
2
binding
*
60mmg=90%
The position of the curve can be defined by the Po
2
at
which 50% of Hb is bound to O
2
(P
50
).
At normal body temp (37°C) arterial blood with a pH of 7.4, a Pco
2
of 40
mmHg,
P
50
27 mmHg.
The higher the P
50
, the lower the affinity of Hb for
O
2
.when the affinity of Hb for O
2
(P
50
) the curve is
shifted to the right unloading of O
2
to the tissues
Oxyhemoglobin Dissociation Curve
Graphic illustration of the % oxy hemoglobin saturation at different values of P02
.
The curve of the relationship between blood PO2 and the percent of Hb saturated with
O2.
It is an S – shaped curve with a steep slope between 10 and 60 mm Hg PO2 and a
flat portion between 60 and 100 mm Hg PO2
.
Loading and unloading of 02 is influenced by the affinity of hemoglobin for 02.
● Affinity is decreased when pH is decreased , Increased temperature and 2,3-DPG that Shift the
curve to the
right(Affinity of hemoglobin for 02 decreases)& Greater unloading of 02
Steep portion
of the sigmoidal curve, small changes in P02 produce large differences in % saturation (unload more
02).
Decreased blood temperature
The factors that shift the curve to the
left, which means that at any given pO2,
Hb has more affinity for O2 (lower P50),
are:
The factors that displace the curve to the
right, which means that at any given
PO2, Hb has less affinity for O2 (higher
P50), are
1- Decrease in [H+] with pH increasing
from 7.4 to 7.6.
2- Decreased 2,3-diphosphoglycerate
(2,3-DPG) concentration.
3 -Decreased CO2
4-The presence of large amount of Hb-F
5-Decreased blood temperature
1-
Increased [H+] with pH decreasing
from concentration from 7.4 to 7.2.
2- Increased CO2
*3 -Increase 2 ,3- DPG a is ,2 ,3
diphosphoglycerate [phosphate
compound normally present in the blood.
4 - Increased blood temperature

