Anthrax
IntroductionThe term “Anthrax” is derived from the Greek word (Anthrakos) which means coal.
A major outbreak in Europe in 1613 killed 60000 persons.
It was the first disease conclusively proved to be caused by microorganism and the first bacterial disease for which an effective vaccine was developed.
Anthrax is considered a leading potential agent in bioterrorism or bio-warfare.
Anthrax—United States, 1951-2002
Animal vaccineAnimal vaccine
Human vaccineBioterrorism
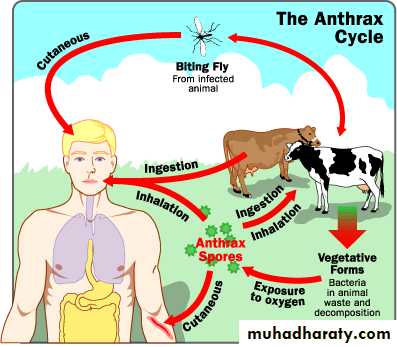
Anthrax is an acute infectious disease caused by the spore forming bacterium Bacillus anthracis. Anthrax most commonly occurs in wild and domestic lower vertebrates (cattle, sheep, goats camels, and other herbivores , but it can also occur in humans when they are exposed to infected animals or tissue from infected animals.Other names for the disease are Wool sorter’s Disease and Rag picker's Disease
What is Anthrax?
Reservoir Reservoirs of infection are animals; cattle, sheep, goats, and pigs. The animal products such as hides, skins, and hair are potential sources of infection.
TransmissionNo person to person transmission
Causative Agent
B. anthracis (Gk: anthrakos – “coal”)a Gram-positive bacterial rod that forms spores on contact with oxygen.
Non-motile
Two states
Vegetative – causes infection via toxin productionSpores
Protective in adverse environments
May subsist for years
Incubation period( it depends on the form of Anthrax)
1-7 daysBut it may be 60 days
Forms of Anthrax
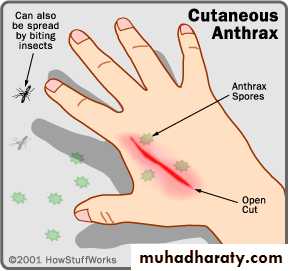
Cutaneous AnthraxIncubation period 1-12 days
Most common form (95%) Papule, then vesicle, then necrotic ulcer (eschar) with black center
Usually painless
Significant edema surrounding the lesion, and in nearby lymph nodes
Case-fatality:
without antibiotics – 5%-20%
with antibiotics – <1%
Cutaneous Anthrax
• Clinical characteristics highly suggestive of cutaneous anthrax include:
• A painless depressed ulcer covered with black eschar
• Surrounding edema out of proportion to the size of the ulcer
• Few neutrophils in vesicular fluid.
Ulcer and vesicle ring
Day 4
Notice the edemaand typical lesions.
Cutaneous Anthrax- Clinical Progression
Day 5
Day 7Day 10-12
Day 15
CDC
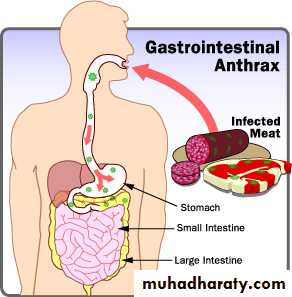
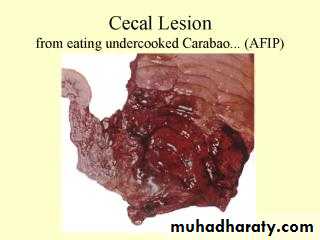
Gastrointestinal Anthrax
• Incubation period 1-7 days• Pharyngeal involvement includes oropharyngeal ulcerations with cervical adenopathy and fever
• Intestinal involvement includes abdominal pain, fever, vomiting or bloody diarrhea
• Case-fatality rate estimated at 25-60%
Oropharyngeal Anthrax
Initial diagnosis
Swelling on side of neckAfter 5 days from initial diagnosis
After 9 days from initial diagnosis
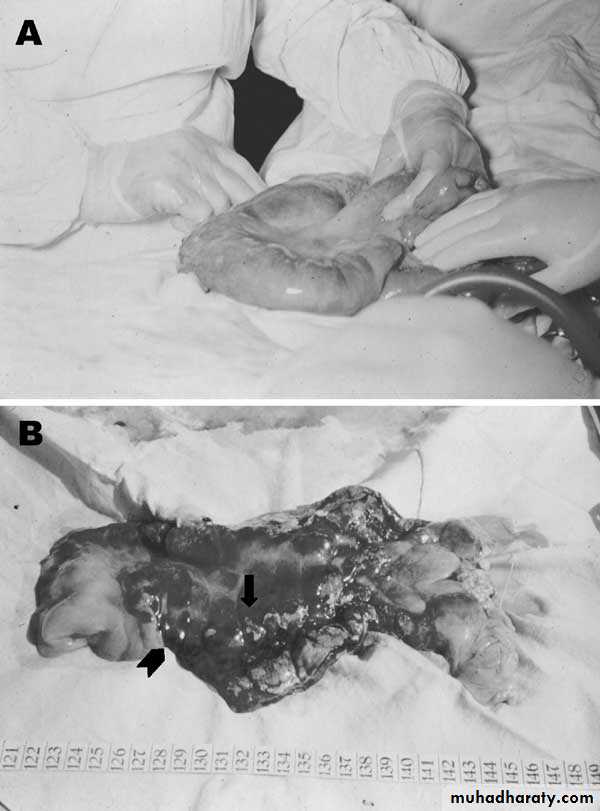
(A) Severe edema of a small bowel caused by anthrax.
This is the samepicture as ( A.) but it has been dissected. The arrows point to the sign of infection.
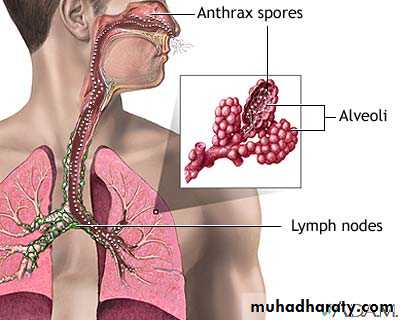
Pulmonary (Inhalation) Anthrax
• Incubation period: 1-7 days Prodrome of Cough, myalgia, fatigue, and fever
• Rapid deterioration with fever, dyspnea, cyanosis and shock, often with radiographic evidence of mediastinal widening
• Case-fatality:
• without antibiotic treatment – 80%- 90%
• with antibiotic treatment – 75% (45% in 2001)
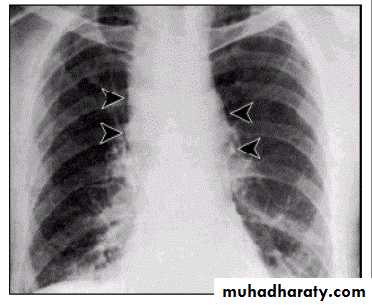
Mediastinal widening due to inhalational anthrax.
Mediastinal widening and pleural effusion on Chest X-Ray in inhalational anthrax
Hemorrhagic meningitis due to inhalation anthrax
Geographic Distribution
B. anthracis found globallyCentral and South America
Southern and Eastern Europe
Asia
Africa
Middle East
Countries with poor veterinary medicine & public health programs
Occurs in animals in United StatesFactors That Influence Natural History of Disease
• 1. Occupation• 2. Amount of organisms
• Infectious Dose: 8,000-10,000 spores
• 3. Spore size
• 2-6 um diameter
• May bind to larger particles
4. Host Factors
General health
Age
Pre-existing conditions
Immunization status
Hygienic practices
5. Treatment
Prompt(without delay)
Appropriate
People at risk
Agricultural exposure to animalsLaboratory exposure
Processors of wool, hair, hides, bones and animal products
Veterinary medical personnel
Biological war and bioterrorism
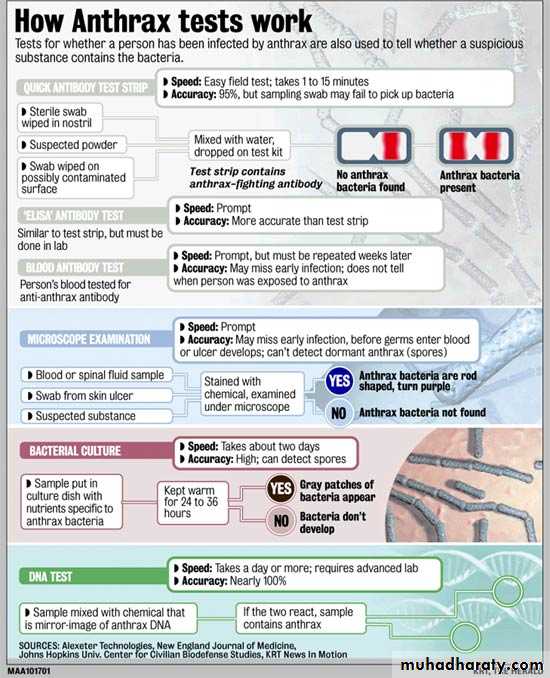
Tests for AnthraxAntibody testsQuick antibody test stripsELISA testBlood testMicroscopic analysisCulture (Blood& exudates)DNA test – PCREnvironmental samplesSwabsWipes
Tests for Anthrax
Preventive measures
Immunization for high risk persons with cell free vaccine (live attenuated vaccine) prepared from culture filtrate containing the protective agent. Recommended for laboratory workers and to protect military personnel.Education about mode of anthrax transmission
Preventive measures (contin.)
Control of animal anthrax by:
Annual immunization of all animal at risk.
Treat symptomatic animals.
Do not necropsy the animal
The preferred disposal technique is to incinerate the carcasses at the site of death.
Affected premises or areas should be quarantined to prevent infected animals from being marketed.
Preventive measures (contin.)
Disinfection of materials contaminated with B. anthracis is complicated by resistance of the spores. However, a variety of procedures are effective: Dry heat, steam under pressure, gamma radiation, and chemical substances.Control
Obligatory case report even a single case of human anthrax especially inhalation type.Concurrent disinfection of discharge.
No need for immunization of contacts.
Investigate source of infection.
Specific treatment; penicillin, tetracycline, erythromycin, ciproflaxacin or doxycycline for inhalation anthrax.
Prophylaxis
ImmunizationPre-exposure chemoprophylaxis
Post-exposure chemoprophylaxis
- Within 24 hours of exposure, if possible:
- Ciprofloxacin or Doxycycline Antibiotics for 60 days without vaccine
Antibiotics for 30 days with 3 doses of vaccine (animal studies)
Who should receive PEP?
Any one exposed to anthrax
Not for contacts of cases, unless also exposed
Anthrax Vaccine
Dosage schedule:
Six (6) doses (subcutaneous injections)
0, 2, 4 weeks
6, 12, 18 months
Annual booster required
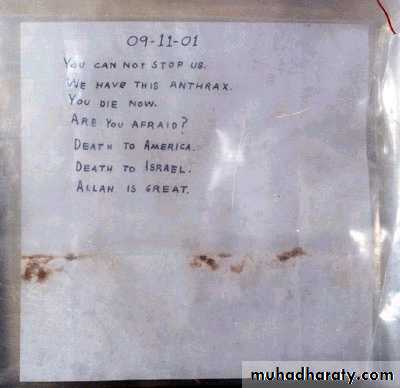
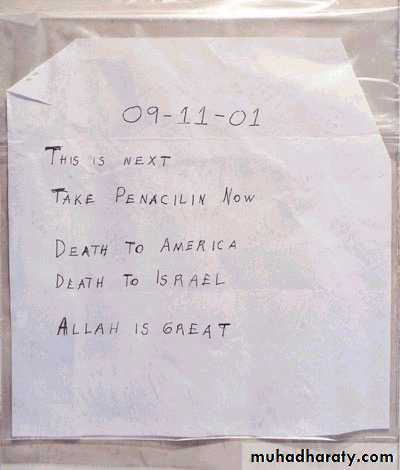
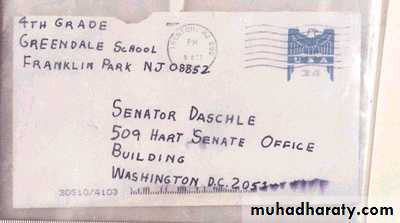
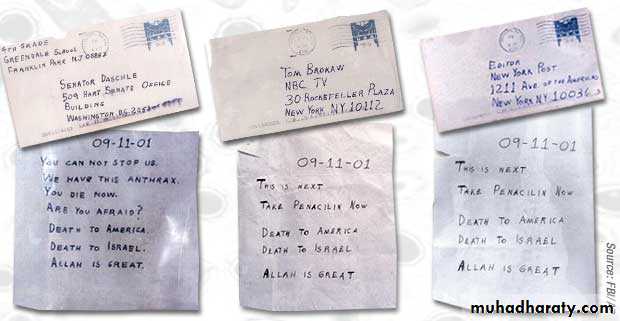
Anthrax Bioterrorism Attacks–United States, 2001
• 22 cases (11 inhalation, 11 cutaneous) in 4 states and DC• B. anthracis sent through U.S. mail
• Most exposures occurred in mail sorting facilities and sites where mail was opened